Qualified Medicare Beneficiary Plus
Qualified Medicare Beneficiary Plus offers the same benefits as QMB Only except for one big difference: People with QMB+ also have full Medicaid benefits.
This means that people with QMB Plus may be eligible to receive supplies through Medicaid. Coverage and plan availability will vary by state. To find out if you have QMB Plus, call the number on the back of your insurance card.
When Doesmedicare Or Medicaid Start
SSDI recipients aren’t eligible to receive Medicare benefitsuntil two years after their date of entitlement to SSDI . Because it oftentakes a year or two to be approved for disability benefits, however, SSDIrecipients often become eligible for Medicare soon after they get their awardletter from Social Security.
In the states where Medicaid eligibility is automatic for SSIrecipients, there is no waiting period for SSI recipients to receive Medicaid.In other states, you need to apply separately for Medicaid, but there is nowaiting period.
How To Choose The Right Coverage For You
Although you may be eligible for both programs, in some cases, you might be in a position to choose between Medicare and Medicaid.
If youre eligible for Medicare, you have to choose between Original Medicare or Medicare Advantage, based on your preferences. But how do you decide? Take a look at some of the key differences.
Don’t Miss: Does Medicare Cover Transportation To Physical Therapy
Key Differences Between Medicare And Medicaid
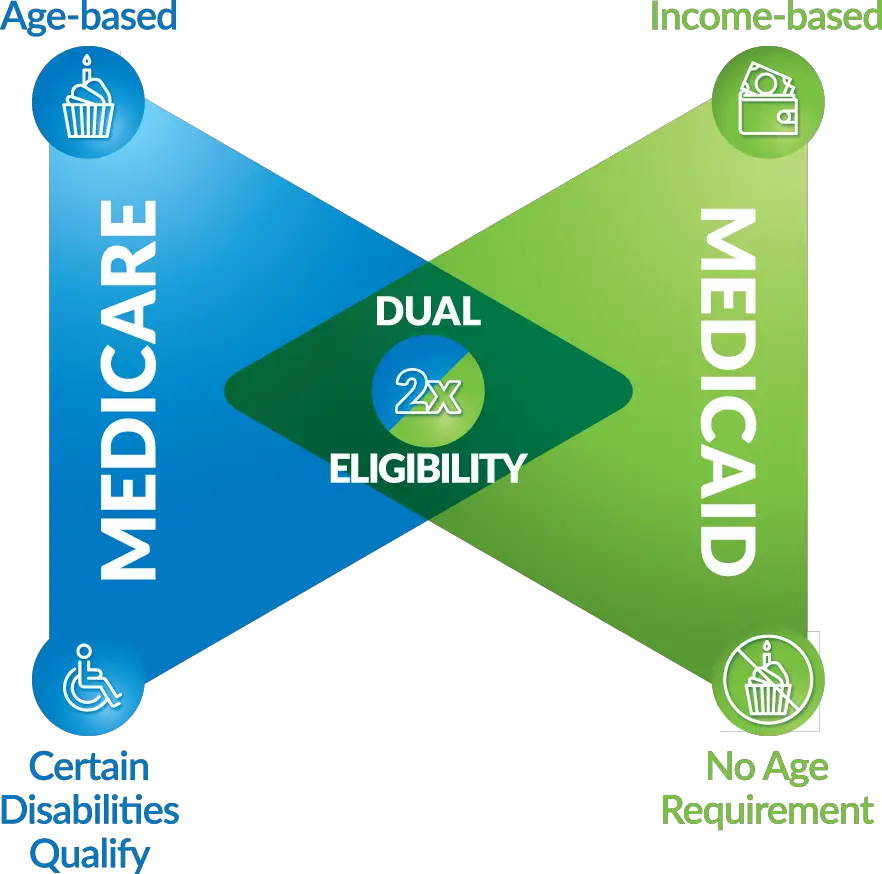
A key difference between Medicare and Medicaid is that one is mainly based on age, and the other is a welfare program for people of all ages with limited financial means.
Medicare assists people 65 or older. In some cases, people under 65 with certain health concerns may be able to sign up. This only applies to the person who qualifies, but not the person’s entire family. Medicaid is jointly run by the state and federal governments. It is for people whose eligibility is based on income rather than age or disability. It helps people and families who meet income limits get health care.
You can apply for Medicaid at any time. You do not have to wait for an open enrollment period. In most cases, people who qualify for it may be exempt from the individual penalty. There’s more on that below. When you apply for Medicare outside the time to enroll, you may have a penalty.
Youre Our First Priorityevery Time

We believe everyone should be able to make financial decisions with confidence. And while our site doesnt feature every company or financial product available on the market, were proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about , but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services.Here is a list of our partners.
You May Like: Does Aetna Medicare Advantage Cover Dental
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Q Can I Have Both Medicaid And Medicare At The Same Time
A. It depends. If you receive Supplemental Security Income from the Social Security Administration, you are automatically eligible for Medicaid and often receive Medicare as well. If you receive both Medicaid and Medicare, Medicaid will pay your Medicare premium, co-payments and deductibles. If you have both Medicare and Medicaid, you should show both cards to your medical care provider each time you receive services. Resources for Those Who Have Medicare and Full-Benefit Medicaid
Recommended Reading: Does Medicare Pay For Stem Cell Knee Replacement
Find Cheap Medicare Plans In Your Area
In the United States, there are currently two government-provided health insurance policies that citizens can enroll in: Medicare and Medicaid. While they both provide general health insurance benefits, there are differences in eligibility and coverage that are crucial to identify and be aware of the largest being that Medicare is available to adults who are over 65 years old whereas Medicaid is only available to low-income families.
Who Is Eligible For Medicare
Medicare is a program that is connected with Social Security. Medicare is available to any US citizen or permanent legal resident who has been in the US for at least 5 years and is at least 65 years old. In certain situations, it also may cover people with disabilities.
For those who are younger than 65 to be eligible for Medicare you must:
- have received 2 years of SS disability benefits or a disability pension from the RRB .
- live with Lou Gehrigs disease
- Incur permanent kidney failure and need regular dialysis or a kidney transplant
If you or your spouse have worked for at least 10 years and have paid Medicare taxes you could qualify for a premium-free Part A plan. To qualify for Medicare parts C and D, you must first enroll in Parts A and B.
Don’t Miss: What’s The Eligibility For Medicare
Are You Dual Eligible
Some people can be eligible for both Medicare and Medicaid at the same time.
Dual-eligible beneficiaries are individuals who are enrolled in Medicare Part A and/or Part B and receive full Medicaid benefits and/or assistance with Medicare premiums.
People who are dual eligible share costs with state-run Medicare Savings Programs , which provide help with premiums, deductibles, coinsurance and copayments, depending on the participant’s income level and the specific MSP. There are programs where eligible participants may have no copayments or cost shares.
This material is provided for informational use only and should not be construed as medical advice or used in place of consulting a licensed medical professional. You should consult your doctor to determine what is right for you.
Humana is a Medicare Advantage HMO, PPO and PFFS organization and a stand-alone prescription drug plan with a Medicare contract. Humana is also a Coordinated Care plan with a Medicare contract and a contract with the state Medicaid program. Enrollment in any Humana plan depends on contract renewal.
Some links on this page may take you to Humana non-Medicare product or service pages or to a different website.
Y0040_GNHKMBZEN
Which Statesmake Medicaid Decisions Based On Ssi Standards
Some states use the same eligibility standards as the federalSSI program but insist on making their own Medicaid decisions. In these states,enrollment in Medicaid isn’t automatic when you are approved for SSI, and youmust file a separate application with the state Medicaid agency to get enrolledin the Medicaid program.
These states, called “SSI criteria states,” are:
|
Alaska |
|
Utah |
Don’t Miss: How Do Zero Premium Medicare Plans Work
How To Get Medicaid
Medicaid differs from Medicare because it is based on finances and not age. These factors are looked at when seeing who qualifies for it:
- Income.
- Disability.
- Family status.
People who may be eligible for Medicaid may include: people who are pregnant, teenagers living alone, parents of sick children, people with high medical costs, blind or disabled people, or people and families with low incomes.
Each state decides on who qualifies financially for the program. Some states that have expanded Medicaid include higher income levels in their eligibility criteria than states who have not expanded it.
You can find out if your state is growing Medicaid and see if you qualify for it based on income or if you can get any other savings on health care.
Medicare Vs Medicaid Compare Benefits
In the context of long term care for the elderly, Medicares benefits are very limited. Medicare does not pay for personal care . Medicare will pay for a very limited number of days of skilled nursing . Medicare will also pay for some home health care, provided it is medical in nature. Starting in 2019, some Medicare Advantage plans started offering long term care benefits. These services and supports are plan specific. But they may include:
- Adult day care
Read Also: Will Medicare Pay For Handicap Bathroom
Which Statesuse Their Own Criteria For Granting Medicaid
Theremaining states do not automatically grant Medicaid to persons withdisabilities who qualify for SSI because they use their own criteria fordetermining whether someone is eligible for Medicaid. These states may haveincome limits that are higher or lower than SSI’s, different asset limits, ordifferent requirements for what makes someone disabled.
Inmost of these states, however, the income limitsfor Medicaid aren’t too different from the income limit for SSI . And many of them use thesame resource limit as SSI program, although several have a lower assetlimit than SSI , and a couple states have a higher asset limit .
These states are called “209 states,” named after a sectionof the legislation that created the SSI program in 1972. This legislationprohibited states from making their Medicaid eligibility criteria stricter thanthe criteria the states were using in 1972. In these states, you must apply forMedicaid with your state’s Medicaid agency or health and human services department.
The 209 states are:
|
Virginia |
Note that Indiana ceased being a 209 state in 2014.
Even though some 209 states have lower income limits than theSSI program, these states have to let Medicaid applicants deduct their medicalexpenses from their income when their eligibility for Medicaid is beingdetermined. This is called “spending-down.” This means that SSIrecipients with high medical bills will qualify for Medicaid in these states.
Opting For Part A Only
Some people choose only to have Medicare Part A coverage so that they dont have to pay the monthly premiums for Medicare Parts B and D. If you still have insurance through an employer , you can add the other parts later with no penalty.
However, if you decline Parts B and D and don’t have another insurance plan in place, you’ll face a late enrollment penalty when you add the other parts later.
In the past, Medicaid programs typically didn’t offer a lot of choice in terms of plan design. Today, most states utilize Medicaid managed care organizations . If there’s more than one MCO option in a given area of the state, you may be allowed to select the one you prefer.
Read Also: Does Medicare Cover Dexa Scan
How Do I Know If I Have Medicare
Since Medicare is a national program, all Medicare insurance cards look the same. Heres an example:
People with Medicare Advantage will have two insurance cards: One for traditional Medicare, and one for their Medicare Advantage plan. Medicare Advantage cards will look different from each other, depending on the plan.
Can I Be Enrolled In Medicare And Medicaid At The Same Time
Q: Can I be enrolled in Medicare and Medicaid at the same time?
A: In many cases, yes. Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they dont have any out-of-pocket healthcare costs.
Beneficiaries with Medicare and Medicaid are known as dual eligibles and account for about 20 percent of Medicare beneficiaries . Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits.
Full-benefit dual eligibles have comprehensive Medicaid coverage, while partial benefit dual eligibles receive help with Medicares premiums and cost sharing through a Medicare Savings Program .
The federal government oversees Medicare eligibility meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs and income limits for these programs vary widely.
Don’t Miss: Does Medicare Cover Family Counseling
What If Iwas Approved For Ssi But Denied Medicaid
If you receive SSI but were denied Medicaid benefits in a 209state or any state for that matter, you should appeal the decision to yourstate’s Medicaid agency. Your state has to follow certain federal Medicaidrules in notifying you of the denial and holding a hearing. To learn more, readNolo’s article on appealinga Medicaid denial.
Self-help services may not be permitted in all states. The information provided on this site is not legal advice, does not constitute a lawyer referral service, and no attorney-client or confidential relationship is or will be formed by use of the site. The attorney listings on this site are paid attorney advertising. In some states, the information on this website may be considered a lawyer referral service. Please reference the Terms of Use and the Supplemental Terms for specific information related to your state. Your use of this website constitutes acceptance of the Terms of Use, Supplemental Terms, Privacy Policy and Cookie Policy. Do Not Sell My Personal Information
Medical Supplies Covered By Medicare
The following medical supplies could be covered by Medicare, depending on individual needs:
Urology Supplies Catheters, insertion kits, lubricant, condom catheters, & more.
Diabetic Supplies Test strips, blood glucose monitors, lancets, test solution, & more.
Ostomy Supplies Skin barriers, 2 piece pouch systems, drainage bags, & more.
Wound Care Supplies Bandages, foam dressings, tape, gauze, hydrogels, & more.
Note: Medicare does not cover absorbent incontinence supplies.
Recommended Reading: Does Medicare Pay For Ensure
Is Medicare A Disability Or Medicaid
Disabled people who are approved for Social Security disability insurance benefits will receive Medicare, and those who are approved for Supplemental Security Income will receive Medicaid. However, SSDI recipients arent eligible to receive Medicare benefits until two years after their date of entitlement.
Q How Do I Join A Managed Care Organization

A. After being notified that you are eligible for Medicaid , you will receive in the mail a packet of information about the different MCO plan options for receiving your Medicaid benefits. You may choose any plan described in this mailing. You probably want to choose a Managed Care Organization to which your doctor belongs. If you need help making this decision, call the Health Benefit Manager at the phone number in the mailing.
Read Also: Can Medicare Take Your House
Understanding Medicare And Medicaid
Medicare is health and hospitalization insurance for people age 65 and older and those under 65 with certain disabilities or end-stage renal disease. Some portions of Medicare are free and others cost money, with premiums typically deducted from your Social Security benefit checks.
Even if you have private insurance you should apply for Medicare. If you wait until after your 65th birthday to apply, you may end up paying a late penalty or higher premiums. For most people, the initial enrollment period is the seven-month period that begins three months before the month in which they turn 65. If you miss that window, you may enroll between January 1 and March 31 each year, although your coverage won’t begin until July 1.
There are four types of Medicare coverage available.
How The Programs Differ
Medicare is an insurance program while Medicaid is a social welfare program.
Medicare recipients get Medicare because they paid for it through payroll taxes while they were working, and through monthly premiums once theyre enrolled.
Medicaid recipients need never have paid taxes and most dont pay premiums for their Medicaid coverage .
Taxpayer funding provides Medicaid to eligible needy people in a manner similar to other social welfare programs like Temporary Assistance for Needy Families Women, Infants and Children and the Supplemental Nutrition Assistance Program.
Also Check: How Much Does Medicare Pay For Dental
I Have Been Receiving Health Care Through Medicaid Will I Lose This Coverage When I Become Eligible For Medicare
En español | You will not lose Medicaid eligibility just because you become entitled to Medicare. As long as your income falls under the limits for Medicaid eligibility in your state, you will receive both types of coverage. More than 8 million people have both Medicare and Medicaid.In this situation, Medicare becomes your primary insurance and settles your medical bills first and Medicaid become secondary, paying for services that Medicare doesnt cover and also paying most of your out-of-pocket expenses in Medicare .When you become eligible for Medicare, you must begin receiving your prescription drug coverage from Medicares Part D drug program, not from Medicaid. You will automatically qualify for the federal Extra Help program, which enables you to receive Part D drug coverage without paying premiums or deductibles and paying only low copays for your drugs. But to get this coverage, you still have to choose a Part D drug plan and enroll in it. To ensure that you pick a plan that gives you maximum coverage at the lowest cost, you may want to contact your state health insurance assistance program , which provides personal help from trained counselors on all Medicare and Medicaid issues free of charge. To find the main toll-free number of your SHIP , go to www.shiptacenter.org and select your state. For more information on the Extra Help program, see section 2 of AARPs consumer guide to the Part D program.
Most People Who Are Approved For Disability Benefits Through The Social Security Administration Get Medicare Or Medicaid Eventually
By Bethany K. Laurence, Attorney
Generally, if you are approved for Social Security disabilityinsurance benefits, you will receive Medicare, and if you are approvedfor Supplemental Security Income , you will receive Medicaid. However, thisisn’t true in all states. Medicaid is operated by the states,and the states are allowed to set eligibility criteria that are different thanSSI’s criteria. As a result, whether getting approved for SSI gets you Medicaiddepends on your state, as we’ll discuss below.
You May Like: When Can You Apply For Part B Medicare
