Who Is Eligible For An Aarp Medicare Supplement Insurance Plan
To enroll in an AARP Medicare Supplement plan, you must be enrolled in Original Medicare with Part A and Part B coverage. Keep in mind that while you might be automatically enrolled in Medicare Part A once you turn 65, enrollment in Part B isnt always automatic.Contact Social Security for enrollment information.
The open enrollment for a Medicare Supplement insurance plan is the six-month period starting the month you turn 65. When you sign up during the Medicare Open Enrollment Period, you can get a supplemental insurance plan regardless of your health.
There are no health questions to answer and no medical examinations. Understand, though, that if you dont enroll at this time, you might be unable to get supplemental insurance at a later time.
If you apply for Medicare Supplement insurance after your open enrollment period, acceptance is determined after medical underwriting. This means you might be ineligible for coverage if you have pre-existing health issues, or you might pay a higher monthly premium.
Here are a few key points on how AARPs Medicare Supplement insurance plans work:
- AARP Medicare Supplement plans only cover one person. Spouses must have their own plan.
- Its illegal to buy a Medicare Supplement insurance plan if you are enrolled in a Medicare Advantage plan. The only exception is if you switch back to Original Medicare.
- The best time to purchase an AARP Medicare Supplement insurance plan is when youre first eligible to avoid medical underwriting.
Coverage Including Exclusions Or Limits
For an individual to qualify for a Medigap plan with the AARP, they must become a member. AARP membership $12 the first year, and then $16 annually.
When someone has an AARP Medigap plan, they can use any Medicare-approved doctor or healthcare provider across the U.S.
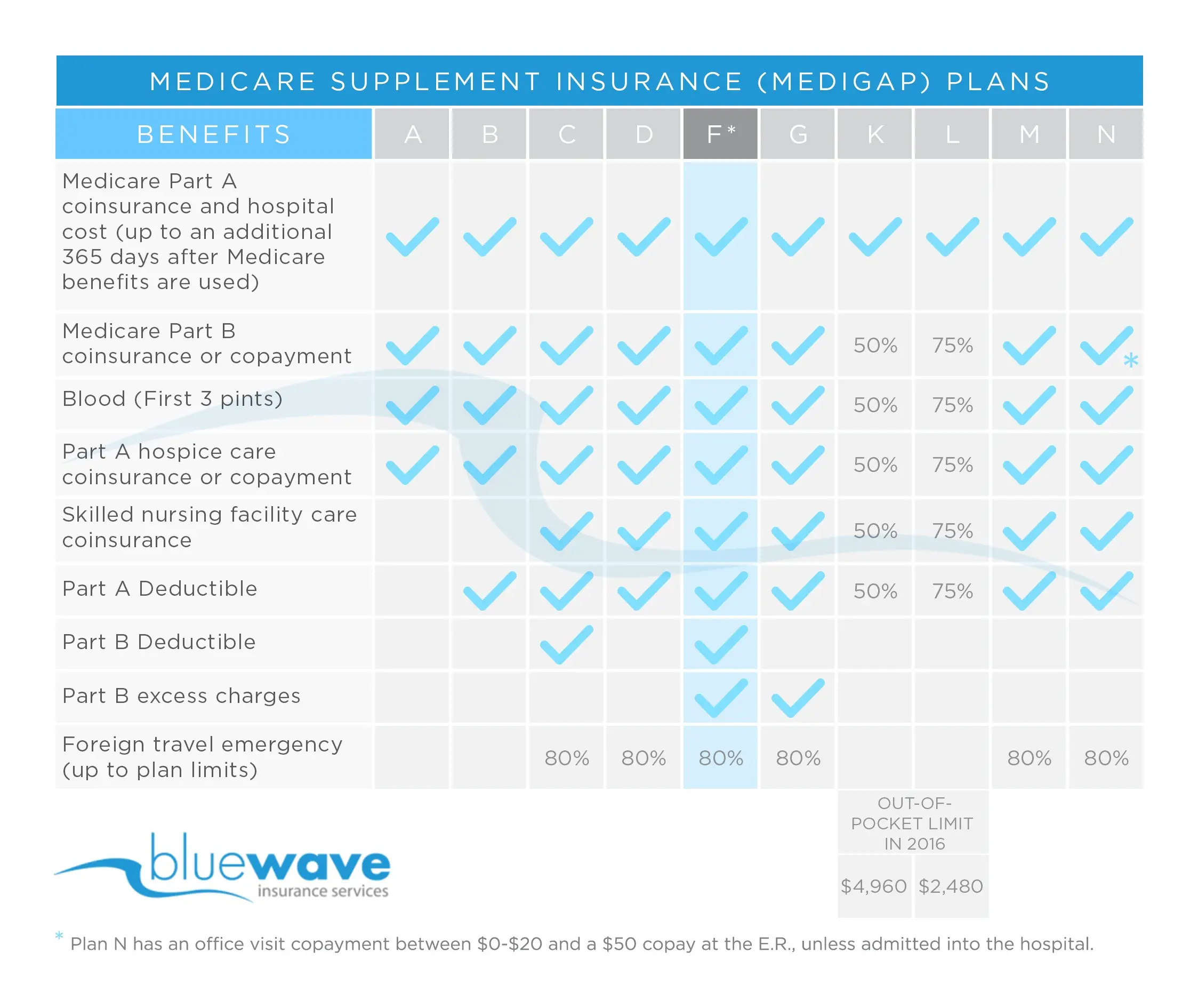
Medicare standardizes the coverage for each Medigap plan. The table below shows some of the benefits covered through the AARP Medigap plans. A person can check the complete coverage details for all AARP plans online.
| Benefit |
|---|
| 50%Plan K |
Plans K and L have annual limits that a person must reach before the insurer begins to pay. In 2021, Plan Kâs out-of-pocket limit is $6,220, and the out-of-pocket limit for Plan L is $3,110.
The Costs Of Medicare Part A Hospitalization
Premium. Most people dont pay premiums for Medicare Part A, which covers inpatient stays in hospitals and skilled nursing facilities, some home health services and end-of-life hospice care. You dont have to pay Part A premiums if you or your spouse had Medicare taxes deducted from your paychecks for at least 40 quarters of work, the equivalent of 10 years or more. The quarters dont have to be consecutive.
If you dont qualify for premium-free Part A, you can choose not to buy it. But if you do have to pay, youll also need to pay for Part B. The Part A premiums in 2022:
- $274 a month if you or your spouse paid 30 to 39 quarters of Medicare taxes
- $499 a month if you or your spouse paid fewer than 30 quarters of Medicare taxes
Deductible. You must pay a $1,556 Part A deductible for each benefit period youre hospitalized in 2022. This benefit period begins when you are admitted to a hospital or skilled nursing facility as an inpatient thats an important distinction because so many places also have outpatient centers and ends when youve been out of the hospital or facility for 60 days in a row.
Coinsurance. You may also have to pay a portion of the costs, called coinsurance, if you stay in a hospital or skilled nursing facility for a long time. Medicare covers the first 60 days as an inpatient in the hospital, but in 2022 you have to pay $389 a day for days 61 to 90 and $778 a day for up to 60 lifetime reserve days.
Don’t Miss: Are Urgent Care Visits Covered By Medicare
Can You Switch Yes But Theres A Catch
Its logical to consider enjoying the cost savings of a Medicare Advantage plan while youre relatively healthy, and then switching back to regular Medicare if you develop a condition you want to be treated at an out-of-town facility. In fact, switching between the two forms of Medicare is an option for everyone during the open enrollment period in the fall. This Annual Election Period runs from October 15 to December 7 each year.
Heres the catch. If you switch back to regular Medicare , you may not be able to sign up for a Medigap insurance policy. When you first sign up for Medicare Part A and Part B, Medigap insurance companies are generally obligated to sell you a policy, regardless of your medical condition. But in subsequent years they may have the right to charge you extra due to your age and preexisting conditions, or not to sell you a policy at all if you have serious medical problems.
Some states have enacted laws to address this. In New York and Connecticut, for example, Medigap insurance plans are guaranteed-issue year-round, while California, Massachusetts, Maine, Missouri, and Oregon have all set aside annual periods in which switching is allowed. If you live in a state that doesnt have this protection, planning to switch between the systems depending on your health condition is a risky business.
What Is Not Covered By Medigap
Medigap is extra health insurance that you buy from a private company to pay health care costs not covered by Original Medicare, such as co-payments, deductibles, and health care if you travel outside the U.S. Medigap policies dont cover long-term care, dental care, vision care, hearing aids, eyeglasses, and private-
You May Like: Do You Have To Be To Get Medicare
Benefits That Differ Between Plan G And Plan N
Medigap Plan G and Plan N have two differences in coverage.
Part B excess charge coverage
Medigap Plan G covers Medicare Part B excess charges, while Plan N doesnt. If a health care provider is legally permitted to charge more than Medicares approved amount and does so, whats left over after Medicares approved amount is an excess charge.
Most health care providers have made an agreement with Medicare to accept the Medicare-approved amount for services, which means they cant bill you for excess charges.
You can search for health care providers in your area that have made these agreements at medicare.gov/care-compare.
Part B coinsurance coverage
Medigap Plan G and Plan N both include Medicare Part B coinsurance coverage, but the level of coverage differs between the two plans. Plan G covers all of your Part B coinsurance, but Plan N doesnt.
Rather than covering your entire Part B coinsurance, Medigap Plan N requires you to pay out of pocket for these visits:
-
Office visits: Copay is up to $20 for certain office visits.
-
Emergency room visits: Copay is up to $50 if youre not admitted to hospital inpatient care.
After those copays, Plan N covers any additional Part B coinsurance for the visit. Plan N also pays the full Part B coinsurance for other types of visits covered by Medicare Part B.
» MORE:Compare Medicare Supplement Insurance plans
Medicare Supplement Plan N Cost
Lets talk a little bit more about the differences between the two plans, and more specifically what other charges you could incur on Medicare Plan N.
Again, if youre somebody who doesnt go to the doctor very oftenand I have clients who never got to the doctor who loves Plan N because they pay lower premiums all year long.
So they absolutely love it. They know if something happens to them, theyve got outstanding coverage, but their out-of-pocket expenses are going to be minimal, even on a Plan N.
So they love Plan N because they dont go to the doctor very often, but they know they are protected very, very well, God forbid something major happens.
Also Check: Will I Lose Medicare If I Start Working
Medicare Supplement Plan N Eligibility And Enrollment
Like other Medigap plans, youre eligible to enroll in Plan N if:
- You are enrolled in both Medicare Part A and Part B
- There is a Plan N available in your service area.
The best time to enroll in Medigap Plan N is during your Medigap Open Enrollment Period, which is the six-month period that automatically starts on the first day of the month that you are both 65 or older and enrolled in Medicare Part B. During this time, you have a guaranteed-issue right to enroll in any Medigap plan available in your service area, regardless of any pre-existing conditions* or disabilities you may have. Insurance companies arent allowed to reject you based on your medical status or charge you more if you have health problems. After your Medigap Open Enrollment Period is over, you may have more difficulty enrolling in a Medicare Supplement plan if you have health problems. Insurance companies are also allowed to use medical underwriting after this period and may charge you higher premiums based on your health status. You may also be denied coverage entirely due to your health status.
Do you have questions about Medigap Plan N and whether it may work for your situation? Feel free to use our eHealth plan finder tool to compare Plan N or other Medigap options in your location just enter your zip code into the tool on this page to get started. If you need immediate assistance, contact eHealth to speak with a licensed insurance agent and get answers to your Medicare questions.
New To Medicare?
What Insurance Company Offers The Best Medicare Supplement Plan G For 2021
Medicare Supplement Insurance benefits are standardized by the federal government. That means Medigap Plan G purchased through AARP will feature the same basic benefits as a Plan G purchased through a different carrier.
The only thing that differentiates one Plan G from another is the cost and any extra incentives the carrier may offer in exchange for your enrollment such as SilverSneakers membership or discounts for multiple policyholders form the same house which some insurance companies may offer.
Recommended Reading: Will Medicare Pay For In Home Caregivers
What Medigap Plans Does Aarp Offer
AARP members can choose from 8 standardized Medigap plans offered through United Healthcare. These plans are A, B, C, F, G, K, L, and N.
Although all 50 states have at least one of these plans, people may not find all 8 plans offered in their state. A person can use this online tool to find a plan in their state.
In addition, if a person became eligible for Medicare on or after January 1, 2020, they cannot purchase Medigap plans C and F that pay for the Part B deductible.
Enrollment For Medigap Plan N
Enrollment begins the first day of the month you turn 65 and are covered under Medicare Part B and ends six months after your birthday month. Applying for benefits during this time is the most beneficial, as insurance companies are not permitted to use medical underwriting. That means you could get the lowest prices available.
Applying for benefits outside of the six-month time window could mean higher premiums or a denial of coverage due to your health.
Recommended Reading: How Much Money Is Deducted From Social Security For Medicare
What Does Medicare Supplement Plan N Cover
Medigap Plan N has coverage for four basic areas:
Additionally, Medicare Supplement Plan N pays for skilled nursing facility care and the Medicare Part A deductible for hospitalization.
What Should I Know About A Plans Drug List
Medicare Part D and Medicare Advantage plans have a drug list that tells you what drugs are covered by a plan. Medicare sets standards for the types of drugs Part D plans must cover, but each plan chooses the specific brand name and generic drugs to include on its formulary. Here are some important things to know:
- A plans drug list can change from year to year.
- Plans can choose to add or remove drugs from their drug list each year. The list can also change for other reasons. For example, if a drug is taken off the market. Your plan will let you know if theres a coverage change to a drug youre taking.
- Many Part D plans have a tiered formulary.
You May Like: How Do I Report A Lost Medicare Card
You May Like: Who Is My Medicare Carrier
Aarp Medicare Supplement Plan K
Looking for more basic Medicare Supplement coverage at a lower cost? Plan K might be the right choice for you. Plan K offers partial coverage for many of the costs youd pay out of pocket. This includes:
- 100% of your coinsurance payments for inpatient hospital care
- 50% of your Part B coinsurance or copayments
- 50% of up to 3 pints of blood
- 50% of your Part A hospice care coinsurance or copayment
- 50% of your coinsurance for care provided in a skilled nursing facility
- 50% of your Part A deductible
An Additional Benefit of Plan K
Plan K is one of only two Medicare Supplement plans that includes an annual out-of-pocket limit. In 2020, this limit is set at $5,880. Once youve spent this amount, your plan will cover 100% of your Medicare costs for the remainder of the year.
Who Is Eligible For Aarp/unitedhealthcare Plan F
To be eligible for Medicare Supplement Insurance, you must be enrolled in both Medicare Part A and Part B.
To be eligible for Plan F, you must have been eligible for Medicare prior to Jan. 1, 2020.
And to be eligible for AARP/UnitedHealthcare Plan F, you must live in an area in which AARP/UnitedHealthcare sells Plan F and you must also be an AARP member.
Don’t Miss: How To Find Out If My Medicare Is Active
What Are The Eligibility Requirements For Aarp Medicare Supplement Plan G
You must be enrolled in Medicare Part A and Part B before you can apply for Medicare Supplement Insurance Plan G. And you must be at least 65 years old to purchase Medigap in some but not all states. Lastly, you must live in the area that is serviced by the plan. While Medigap can be used anywhere that Original Medicare is accepted, it can only be purchased in the county or zip code in which you reside.
To apply for AARP Medicare Supplement Plan G or any other Medigap plan from AARP, you must be an AARP member. Memberships are $16 per year in 2021 and include a number of savings and discounts on travel, dining, shopping and more.
Aarp Medicare Supplement Plan C
One of the most exhaustive Medicare Supplement options, Plan C covers most out-of-pocket expenses. However, Plan C is being phased out. Those who became eligible for Medicare after January 1, 2020, will not be able to purchase this plan.
Plan C includes all of the benefits offered under Plan A. For those who are eligible, AARPs Plan C also covers:
- Coinsurance for care provided in a skilled nursing facility
- Your Medicare Part A deductible
- 100% of approved foreign travel emergency costs
You May Like: When Do You Sign Up For Medicare
Aarp Medicare Supplement Plan G
Like Plan F, Plan G is one of the most comprehensive Medicare Supplement plans available. Plan G does not cover your Medicare Part B deductible. However, it does cover all of the standard benefits included with Plan A. It also includes:
- Medicare Part B excess charges
- Coinsurance for care provided in a skilled nursing facility
- Your Medicare Part A deductible
- 100% of approved foreign travel emergency costs
AARP Medicare Supplement Plan G: The High-Deductible Option
AARP also offers a high-deductible version of Plan G. This option will require you to pay a deductible of $2,340 before the plan begins to assist with costs. Once youve met your deductible, the plan will pay 100% of covered costs for the remainder of the year. This plan does not cover your Part B deductible. However, it will count your payment toward your Plan G deductible.
Which Medigap Plan Is Right For You
For many years, Plan F dominated the market as the most-popular plan for beneficiaries. However, in recent years Plan G and Plan N have been gaining in popularity. There are many people out there who would rather have lower premiums and then just pay the Part B deductible and doctor copays IF they need to use those services.
Its up to you but heres a great infographic to help you see a side by side example. In this image we are using rates for a male, non-tobacco user turning 65 in Texas in 2022.
Recommended Reading: Is Evenity Covered By Medicare Part B
Plan N Lets Look At An Example
Karen tells her agent that she visits the doctor only once or twice a year. She feels that a full coverage Plan F isnt really necessary due to her low usage. Her agent explains that Plan N has premiums about 30% less than Medigap F if she would be willing to take on copays for a few minor things.
For inpatient care, Medicare Supplement Plan N fully covers the hospital deductible for admitted patients. For outpatient care, Karen will pay the Part B deductible upon her first doctor visit of the year. She then pays a copayment of up to $20 when she sees her physicians during the rest of the year. She may pay an excess charge if her doctor is not a participating Medicare doctor. Lets look at how these expenses on Plan N might affect her.
Lets say Karen visits her podiatrist in the middle of the year, after her deductible has already been met. Medicares assigned rate for a visit to this foot specialist is $100. If the doctor does not accept assigned rates, he can balance bill Karen for up to 15% beyond the approved rate for this visit, or a maximum of $15 in this case.
Karen owes her $20 copay, and her Supplement will pay the remainder of the approved charges.
If you find that Plan N is hard to understand because of the excess charges and copays, but you still like the idea of lower premiums, then you might check out Plan G. On Plan G, excess charges are covered by your Medigap plan. On Plan G, your cost-sharing is limited to the Part B deductible only.