What Durable Medical Equipment Is Covered By Medicare
The cost of durable medical equipment is covered by Medicare if it is deemed medically necessary, and has been prescribed by a doctor for use at home. The list of covered durable medical equipment includes:
- Blood sugar monitors.
Your client will pay 20% of the Medicare-approved amount for the equipment, and they will be liable for any remaining deductible under Medicare Part B.
V Frequently Asked Questions
What is the difference between home health and home care?
The difference between home care and home health care is that home health care involves skilled nursing care from trained medical professionals. On the other hand, standard home care focuses on companion care, personal care and assistance with ADLs, and household assistance. Standard home care aides do not need any nursing or medical certification, while home health aides do.
Will Medicare pay for in-home care for the elderly?
Medicare will pay for in-home care for the elderly under certain circumstances. In general only home health care, not personal or companion care, is covered. Home health care includes skilled nursing care, therapy services, and other medical services. If you need personal care and home health care and receive them both from the same Medicare-approved provider, in-home personal care should be covered.
What home health care is covered by Medicare?
Medicare covers several home health care services, including intermittent skilled nursing care , therapy services like physical and occupational therapy, and medical social services. Medicare does not cover companion care, transportation, and meal delivery.
How much does home care cost?
According to Genworth Financial, home care costs an average of $25 an hour for personal or companion care and $26 an hour for home health care. This comes out to an average of $4,481 and $4,576 per month, respectively, for 44 hours of care per week.
Medicaid Certified Home Care Agency In New Jersey
Claiming Medicaid in New Jersey requires homecare agencies to get HHA certification. The agencies need to follow certain regulations that are set by their state regarding certifications and licensing. These can be found at the Bureau of Licensing and Certification or states Department of Human Services.
Governing Body: New Jersey Department of Human Services
Also Check: How Can I Sign Up For Medicare Part B
How Do I Qualify For Medicare Home Health Care
Medicare has several requirements to cover home health aide services and other home health care:
- Your doctor must write a formal treatment plan specifying the home health services you need and certifying that you need the services to improve or maintain your condition. This is usually done in consultation with the home health agency that will be treating you.
- You must be certified by your doctor as homebound, which means you are unable to leave home without assistance or special transportation. Medicare may consider you homebound if leaving the house requires considerable and taxing effort.
- Your doctor must monitor the services you receive at home.
- Your home health agency must be approved by Medicare.
If you meet all of the above requirements, Medicare may cover part-time, intermittent home health aide services for up to 21 days. Medicare generally covers fewer than seven days a week of home health aide visits, and fewer than eight hours of care per visit.
If you need full-time, daily home health care, Medicare Part A and Part B might not cover it. The Medicare home health care benefit is only for intermittent, part-time services for less than 21 days. A Medicare Advantage plan might cover some home health care as described later in this article.
Dont Miss: Dentist In Dublin Ga That Accept Medicaid
How Can I Pay For A Long
There are a few programs that might help cover costs. Long-term care insurance is an option to consider if theres sufficient time to plan ahead. If the person has served in the U.S. military, veterans and their spouses can seek VA benefits to cover stays at selected facilities. There are also financial instruments such as reverse mortgages or even whole life insurance policies that can help.
Actually, many people start by paying for nursing home care out of their own savings, primarily because of the flexibility it offers when choosing a facility. Skilled nursing care communities have a limit on the number of government-funded patients they can admit. So, private payers gain the advantage of choice in selecting a nursing home that meets their needs. If paying privately is not feasible, Medicaid then becomes an option.
Also Check: Does Medicare Cover Ambulance Transport
What Is Medicare Skilled Nursing Care
According to the Centers for Medicare & Medicaid Services , skilled nursing care is care given by a nurse or other trained health care provider who can administer IVs and other injections, change out wound dressings, manage medication doses and more. Coverage is good for a certain number of skilled nursing care hours per day and per week.
When skilled nursing care is needed, the benefits also extend to personal care, or custodial care. This includes assistance with activities of daily living like bathing, dressing, toileting, eating, mobility and more.
Other home health care services covered by Medicare include physical, occupational and speech therapy, along with social services like counseling.
What Home Care Services Does Medicare Cover
The primary objective of Medicares home care program is to provide seniors with short-term skilled services in the comfort of their own homes as an alternative to recovering in a hospital or skilled nursing facility.
Skilled nursing services are those that must be provided by a qualified health professional, such as a Registered Nurse or a Licensed Practical Nurse .
Examples of these services include:
- Monitoring of a patients vital signs and overall health
- Wound care for a pressure ulcer or surgical incision
- Administration of intravenous drugs or nutrition therapy
- Catheter changes
- Patient and caregiver education
Skilled therapy services are those that must be provided by or under the supervision of a licensed physical therapist, occupational therapist or speech-language therapist.
- Physical therapy exercises typically focus on improving and restoring strength, balance and range of motion for optimal physical function.
- Occupational therapy assists in regaining the ability to independently engage in activities of daily living and adapting these tasks or the surrounding environment to improve functionality and accessibility.
- Speech-language therapy helps patients regain the ability to speak and communicate as well as overcome swallowing difficulties .
Don’t Miss: Does Everyone Qualify For Medicare
Does Medicare Cover In
Medicare is the health insurance of choice for nearly 20% of Americans, covering more than 63 million older adults. Depending on the plan, Medicare covers a wide variety of services from doctors visits to prescription drugs, but many seniors may require in-home care or home health care at some point during their coverage periodand many are left wondering if Medicare covers this important service.
Types Of Services Provided
Different kinds of home health care professionals deliver different services.
Registered nurses or licensed practical nurses under the supervision of a registered nurse deliver skilled nursing care.
This includes:
- Giving injections, intravenous drugs or tube feedings
- Teaching about prescription drugs and diabetes care
Some of the tasks home health aides do include:
- Checking blood pressure, breathing, heart rate and temperature
- Checking the safety of the home
- Ensuring medications are being taken correctly
- Monitoring food and drink intake
- Teaching patients and caregivers about the plan of care and how to carry it out
Professional therapists provide specific kinds of services, including physical therapy, speech therapy and occupational therapy.
Social workers provide medical social services.
“Your doctor or other health care provider may recommend you get services more often than Medicare covers,” Medicare’s website says. Or they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs. Ask questions so you understand why your doctor is recommending certain services and whether Medicare will pay for them.
Medicare home health benefits do not cover full-time skilled nursing care. They also do not cover drugs, housekeeping, meal delivery or transportation.
Editor’s note: This article was originally publised Oct. 11, 2019. It has been updated with more recent information on home health use by Medicare beneficiaries.
Recommended Reading: Should I Get Medicare Supplemental Insurance
Does Medicaid Pay For Caregivers
In most cases, the adult child / caregiver is paid the Medicaid approved hourly rate for home care, which is specific to their state. In very approximate terms, caregivers can expect to be paid between $9.00 $19.25 per hour. It is important to note that the phrase consumer direction is not used in all states.
Does Medicare Cover Durable Medical Equipment
Medicare will cover the cost of medically required equipment for in-home usage that a physician has prescribed.Canes or walkers, wheelchairs, blood sugar monitors, nebulizers, oxygen, and hospital beds are all included in this category. Patients typically pay 20% of the Medicare-approved price for such devices, plus any applicable Part B deductible.
Also Check: Does Medicare Pay For Cancer Drugs
What Kinds Of Home Health Services Does Medicare Cover
Home health services are provided in your home versus in a hospital or skilled nursing facility. Home health care is less expensive and more convenient for you because it is provided in the comfort of your home. The goals of home health services are to:
- Help you get better, regain your independence, and help you become as self-sufficient as possible
- Maintain your current level of functioning, so your condition doesnt worsen
- Slow your decline
The kinds of Medicare-covered home health services you may receive include:
- Part-time or intermittent skilled nursing care that can only be provided by a licensed nursing professional and to coordinate your plan of care
- Physical therapy to help minimize pain and improve flexibility
- Occupational therapy to help improve your ability to safely function and move around
- Speech-language pathology to help with swallowing or speech
- Medical social services to provide emotional and social support and help you access community resources
- Part-time or intermittent home health aide services to provide personal hands-on care
- Injectable osteoporosis drugs for women who have a bone fracture related to postmenopausal osteoporosis and who are unable to self-administer
Recommended Reading: Do Medicare Advantage Plans Cover Chemotherapy
When Might Medicare Cover In
In general, Medicare doesnt cover long-term home health care. Heres how Medicare coverage of in-home health care typically works.
In most cases, even when Medicare covers in-home health care, its for part-time care, and for a limited time. Some of the requirements may include:
- You must be under the care of a doctor, who must have a plan of care for you that she or he regularly reviews.
- The in-home health agency must be Medicare-approved.
- Your doctor must certify that youre unable to leave your home without some difficulty for example, you might need transportation and/or help from a cane, a walker, a wheelchair, and/or someone to help you. In other words, youre homebound.
- Your doctor has to certify that you need certain kinds of in-home care, such as:
- Skilled nursing services when you dont need constant care. That is, you need these services intermittently.
- Continued occupational therapy*
- Speech language pathology*
This may not be a complete list.
*Medicare has certain rules about covering this type of service. If your doctor orders it for you, you may want to contact your Medicare Advantage plan, or Medicare, to see if itll be covered. Contact information for Medicare is at the bottom of this page.
Don’t Miss: Does Medicare Pay For Lift Chairs For The Elderly
Will Medicaid Cover Long
Many Medicare enrollees qualify for Medicaid due to their low incomes and assets. In contrast to Medicare, Medicaid covers nursing facility care and Home and Community-Based Services .Because long-term care is so expensive, many states have more significant Medicaid income restrictions for long-term care benefits than for other Medicaid benefits. However, Medicaids asset limits typically require you to spend down your assets to qualify.
Is Physical Occupational And Speech Therapy Covered By Medicare
When physical therapy requires to help patients regain movement or strength following an injury or illness, Medicare will pay for it. Similarly, it would cover occupational therapy to rehabilitate patients functionality and speech pathology to help patients restore communication ability. So, how many hours of home health care does medicare cover
But if their condition is projected to improve in a fair amount of time. However, Medicare will fund these services. The patient requires a professional therapist to administer a maintenance program to address the injury or sickness at hand.
Recommended Reading: How To Call Medicare Office
Does Medicare Cover Living In A Nursing Home
The simple answer is no. Just like most health insurance plans, Medicare does not pay for long-term care stays. That means Medicare will not pay for any type of long-term residenceincluding assisted living and memory care facilities. However, it can help pay for the necessary doctors services and medical supplies a person might need while staying at such a facility.
In a situation where someone is admitted to the hospital and then needs further oversight to recover, Medicare will cover part of the short-term rehab stay, which could take place in a nursing home.
Medicare covers a portion of the short-term stay up to 100 days, as long as the patient continues to get better. If the patients health is not deemed to be improving, coverage will be terminated. But if the patient is making progress and needs to exceed the 100-day limit, an appeal for a longer stay can be submitted.
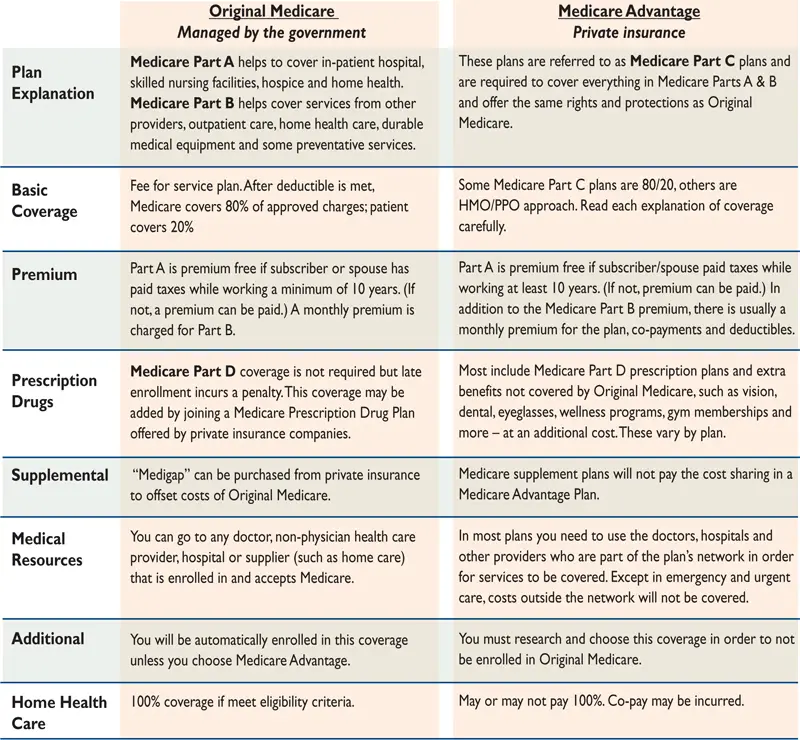
Does Medicare Advantage Cover Home Health Aide Services
Medicare Advantage plans are offered by private insurance companies. They must provide the same coverage as Original Medicare at a minimum. Some many plans offer additional benefits to their members, including expanded coverage for home health care.
Some Medicare Advantage plans may include limited home health benefits. This coverage might include coverage for at-home meal and grocery delivery, transportation to and from doctor visits, and home health aide services for custodial care not typically covered under Original Medicare.
Not all Medicare Advantage plans offer these benefits, and those that do may have limitations on how the benefits can be used. For example, the plan may choose to cover up to 50 hours per year of home health aide services, or 20 transportation trips per year. They may also require you to use a network home health agency or transportation provider. You may have a copayment or coinsurance amount for these services.
Different Medicare Advantage plans can have different extra benefits. Its important to consult your plan benefit booklet to see what Medicare home health care services are covered and the cost-sharing structure for these services.
To look for a Medicare Advantage plan that covers home health aides, enter your zip code on this page.
New To Medicare?
Becoming eligible for Medicare can be daunting. But dont worry, were here to help you understand Medicare in 15 minutes or less.
Dont Miss: Medicaid Health And Human Services
Read Also: Does Medicare Cover While Traveling Abroad
How Much Will I Have To Pay If I Qualify
With Original Medicare coverage , eligible seniors will pay nothing for home health care services that are ordered by a doctor and provided by a certified home health agency. Any additional services provided outside of the approved care plan will not be covered and must be paid for out of pocket.
Be aware that before services begin, the home health agency should provide an itemized receipt or plan of care that identifies what is eligible for Medicare coverage and what is not. A written notice called the Advance Beneficiary Notice of Noncoverage will detail any services and durable medical equipment that Medicare will not pay for as well as the costs the patient will be responsible for.
Use the guide below to determine the combination of payment options that will help your family cover home care costs.
What Are Home And Community Based Services
Home and Community Based Services allow Medicaid recipients to receive necessary services in their own homes or as part of their existing community. Eligibility for HCBS depends on the state youre applying in, but its generally based on whether the recipient would otherwise need care in an institutional setting, like a nursing home.
Many seniors are reluctant to move into nursing homes, especially if theyre currently living in a senior community or if they expect their health problems to improve over time. For these individuals, in-home care including necessary medical care and help with day-to-day tasks is often preferable.
You May Like: How Old Before Eligible For Medicare
What Home Health Aide Services Are Covered By Medicare
Original Medicare generally only covers home health aide services such as skilled nursing care, occupational or physical therapy, or speech-language pathology services. If you only need home health aide services for help with bathing, dressing, and other activities of daily living , Original Medicare typically doesnt cover those services.
For example, lets say your doctor arranges for home nursing and physical therapy visits to help you recover from a stroke. Medicare may cover part-time, intermittent home health aide services if your doctor believes they are medically necessary for your treatment plan.
Will Medicaid Pay For Home Health Care By A Family Member
When Medicaid sponsors home health services, the participants doctor coordinates with plan-participating home health providers. These providers are licensed medical professionals who can meet your loved ones medical needs, and Medicaid pays those providers directly. A home health provider must meet a number of requirements to be covered by Medicaid, so unlicensed family caregivers wont be paid for home health services.
However, in some states, Medicaid allows relatives to get paid for home care services they provide. Medicaid payments to family home care providers vary by state, but some do have programs in place that cover these payments instead of paying a home care agency. For many seniors, aging in place is preferable since they can receive the help they need surrounded by the comforts of their own homes, and for a family member, getting paid to provide home care services can make the duty of caregiving more feasible.
Read Also: Does Plan N Cover Medicare Deductible
