When Does Medicare Cover Substance Abuse
Medicare covers some mental health services, which includes treatment for substance abuse. Both inpatient and outpatient care may be covered, as long as the treatment is reasonable and necessary.
In all cases, the treatment must be provided by someone licensed by Medicare to offer the services. The treatment must also be approved by Medicare. If youre unsure if your provider or treatment is covered, its best to check with Medicare or your plan provider.
Other Benefits For Addiction Treatment
Many Medicare Advantage plans offer supplemental benefits you can’t get with traditional Medicare. The specific supplemental benefits you can get depend on your plan. You may have to meet certain eligibility criteria, such as getting a referral from a doctor. Some supplemental benefits that may offer additional support to people living with addiction include:
- complementary and holistic care, such as acupuncture and chiropractic care
- nutrition and wellness consultations
Which Health Providers Can Bill Medicare Directly For Mental Health And Substance Use Disorder Services And How Much Does Medicare Pay For These Services
Medicare provides coverage and reimbursement for mental health services provided by psychiatrists or other doctors, clinical psychologists, clinical social workers, clinical nurse specialists, nurse practitioners, and physician assistants. Medicare does not provide coverage or reimbursement for mental health services provided by licensed professional counselors and licensed marriage and family therapists.
Medicare fees vary by type of provider, according to the Medicare Physician Fee Schedule :
Also Check: Must I Take Medicare At 65
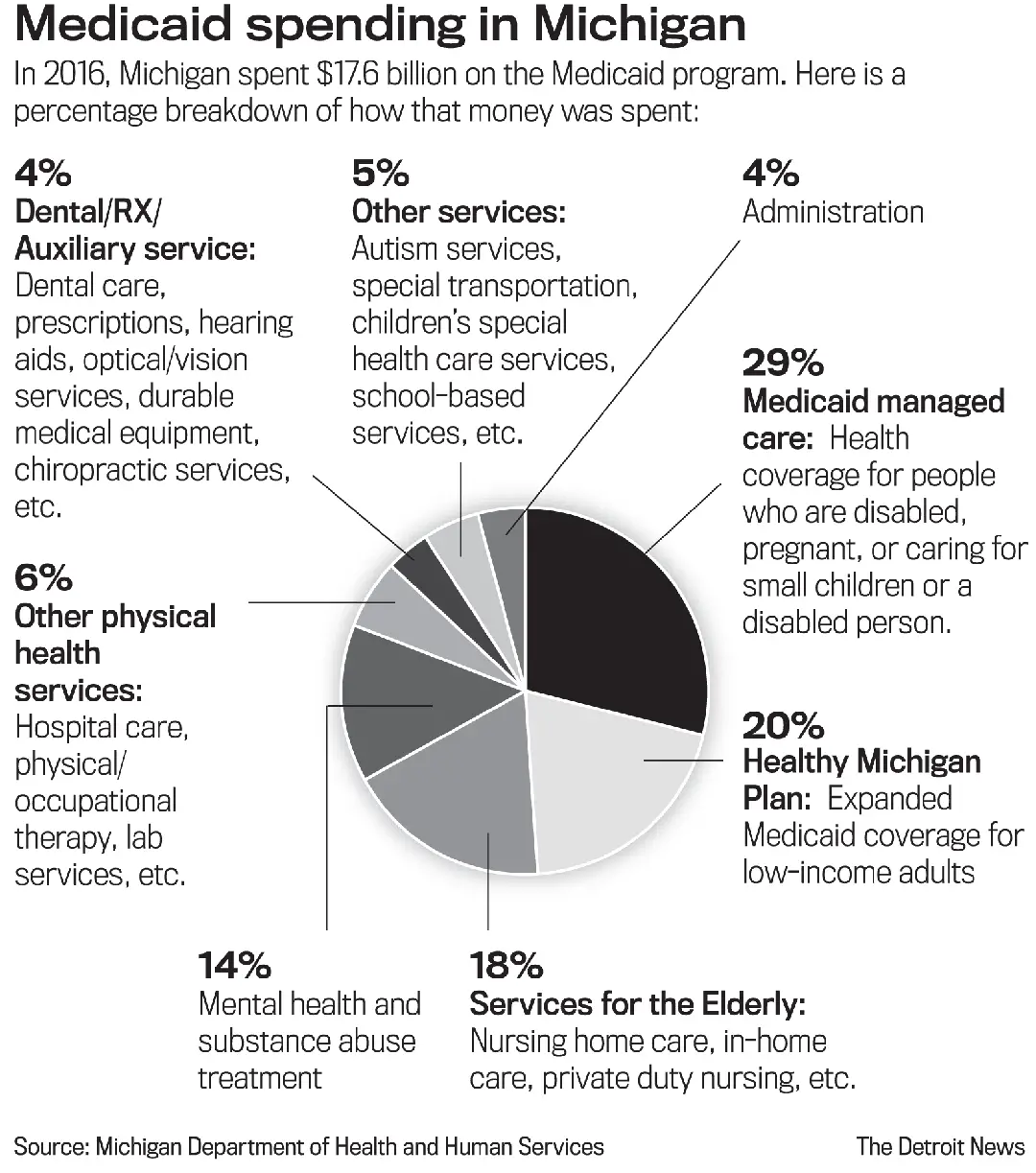
Medicaid For Drug And Alcohol Rehab
Medicaid is a public insurance program for low-income families. Under the 2010 Affordable Care Act , also known as Obamacare, insurance providers must cover all basic aspects of drug and alcohol dependency recovery. While Medicaid covers substance abuse treatment, not all facilities accept Medicaid as a form of payment. To find a recovery provider that accepts Medicaid, get in touch with the Substance Abuse and Mental Health Services Administration . Additionally, individuals can find a directory of rehabs and insurance providers here to aid in the search for local treatment centers and centers throughout the country.
Featured Centers Accepting Medicare and/or Medicaid
- Within a specified income bracket
In some states, Medicaid covers all adults below a certain income level. Those who receive Supplemental Security Income are often automatically eligible for Medicaid.
The ACA requires people to earn less than 133 percent of the federal poverty level to be eligible for Medicaid. A person living above the poverty level may still be eligible for government insurance if they fall in the right income bracket.
Even if someone meets income requirements, they may not be eligible for Medicaid. Each state has its own rules for Medicaid eligibility.
Does Medicare Cover Substance Abuse Counseling

Part A covers substance abuse counseling while you are inpatient. Part B includes substance abuse counseling when a mental health doctor provides care. Mental health professionals include psychiatrists, psychologists, and licensed clinical social workers.
Medicare pays for individual or group sessions. But it doesnt pay for support groups, peer counseling, or other informal counseling. Medicare will also pay for telehealth counseling as part of an opioid treatment program.
Recommended Reading: What Is Medicare Advantage Plus
Check If Medicare Covers Drug And Alcohol Rehab
Before choosing the right drug and alcohol addiction treatment center for you, check your Medicare policy benefits to determine which costs will be covered by your insurance company and which will be out-of-pocket for you. Call the number on the back of your insurance card or log in to your account on Medicares website to learn more about what your specific policy plan covers.
Knowing exactly what your Medicare plan covers can give you peace of mind while you or your loved one is in rehab. You can do the work of getting and staying sober without worrying about unexpected costs or financial struggles. For more information on Medicare insurance plans and to check what your plan covers, call , , or fill out the form below.
Medicare For Drug And Alcohol Rehab
Medicare is available to anyone over 65 years old and those with disabilities. Medicare is available for a monthly premium, which is based on the recipients income. People who earn less pay lower premiums.
Medicare can cover the costs of inpatient and outpatient drug rehabilitation. It consists of four parts that cover different parts of addiction recovery programs.
| The Four Parts of Medicare | |
|---|---|
| Part A | Insurance for Hospital Stays. Medicare Part A can help pay for inpatient rehabilitation. Part A covers up to 60 days in treatment without a co-insurance payment. People using Part A do have to pay a deductible. Medicare only covers 190 days of inpatient care for a persons lifetime. |
| Part B | Medical Insurance. Part B can cover outpatient care for addicted people. Medicare Part B covers up to 80 percent of these costs. Part B covers outpatient care, therapy, drugs administered via clinics and professional interventions. Part B also covers treatment for co-occurring disorders like depression. |
| Part C | Medicare-approved Private Insurance. People who want more benefits under Medicare can opt for Part C. Out-of-pocket costs and coverage is different and may be more expensive. |
| Part D | Prescription Insurance. Medicare Part D can help cover the costs of addiction medications. People in recovery often need medication to manage withdrawal symptoms and cravings. These medications increase the likelihood of staying sober. |
Don’t Miss: Does Medicare Pay For Long Term Memory Care
Do I Need Health Insurance To Receive This Service
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
What Kind Of Addiction Treatment Does Medicare Cover
Typically, young adults struggle with the highest rates of substance abuse or addiction. Substance abuse typically begins to wane around age 26 and continues to decline as individuals age. However, many older adults still struggle with addiction, including addiction to prescription drugs, which they are more likely to receive for a variety of health conditions like
The Center for Behavioral Health Statistics and Quality Short Report found that, in 2014, there were over 1 million people, ages 65 and older, with a substance use disorder 978,000 older adults with an alcohol use disorder , formerly called alcoholism and 161,000 older adults with an addiction to illicit drugs. As the baby boomer generation ages into retirement, these adults bring their unique patterns of substance abuse into their older years, which is estimated to increase rates of drug or alcohol abuse from 2.2 percent to 3.1 percent between 2001 and 2020.
With more older adults struggling with drugs and alcohol, it is important to know which resources are available to support treatment. Medically supervised detox and behavioral counseling in a rehabilitation program make up the foundation of evidence-based addiction treatment, but what is the best way to afford detox and rehabilitation?
Recommended Reading: Is Kidney Dialysis Covered By Medicare
Outpatient Vs Inpatient Alcohol And Substance Abuse Treatment
Medicare Part A covers inpatient alcohol and substance abuse treatment while Medicare Part B covers outpatient treatment.
Inpatient typically means care you receive after youve been formally admitted to a hospital. Outpatient means any treatment you may receive without being formally admitted to a hospital.
Medicare Part A helps pay for treatment you receive if you have to be hospitalized for your condition. It also covers care you receive in a specialized rehabilitation hospital or rehab facility where you will stay during your treatment.
Examples of Inpatient Treatment Services Medicare Part A Covers
- Care received from doctors and nurses in a hospital setting
- Medications needed for your treatment in a hospital setting
Medicare Part B medical insurance covers your treatment if you receive it in an outpatient setting such as a clinic, hospital outpatient department or an opioid treatment program.
Examples of Outpatient Treatment Services Medicare Part B Covers
- Alcohol misuse screenings
- Partial hospitalization in the event of intensive drug rehab
- Psychiatric evaluations
- Individual or group therapy
Medicare Part B will also help cover your telehealth treatment if you meet certain requirements. You are still responsible for 20% of the Medicare-approved cost for your doctor or other health care providers services and your Part B deductible still applies.
Does Medicare Cover Methadone Treatment
Methadone is the oldest and best-known opioid treatment. If administered to an inpatient at a hospital, Part A covers methadone. For people who are not inpatient, methadone is a highly controlled prescription drug that you cant get at a regular pharmacy.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
Patients must go to an opioid treatment center for daily doses of methadone. Medicare covers methadone and other opioid treatment services that enroll in Medicare.
Read Also: Are Canes Covered By Medicare
Paying For Rehab With Medicaid And Medicare
Start the road to recovery
Rehab Questions Info
Get confidential help 24/7. Call now for:
- Access to licensed treatment centers
- Information on treatment plans
Addiction Center is not affiliated with any insurance.
Common Questions About Rehab
Am I covered for addiction treatment?
Have a confidential, completely free conversation with a treatment provider about your financial options.
How Does Medicare Cover Inpatient Substance Use Treatment
If inpatient SUD treatment is deemed reasonable and medically necessary, Medicare covers it just as they would any other hospitalization.
The beneficiary will be responsible for paying their Part A deductible , and can get up to 60 days of inpatient treatment. If inpatient treatment is still considered medically necessary after that, Medicare will cover up to 30 additional days with the beneficiary paying $389 per day in 2022. After 90 days, the beneficiary would start using up their lifetime reserve days if they remained in inpatient care.
Medicare does not have a limit on the number of times a beneficiary can receive inpatient care in a general hospital. But if care is provided in a psychiatric hospital, there is a lifetime cap of 190 days that can be covered by Medicare.
Don’t Miss: What Are The Pros And Cons Of Medicare For All
Medicare And The Level Of Care
Medicare insurance can cover multiple levels of care that include outpatient, telehealth, and IOP programs. ChoicePoint, a leading alcohol and drug rehab center in New Jersey, accepts Medicare for the complete addiction recovery programs. So if you are still searching Does medicare cover alcohol rehab? then the short answer is yes. All you need to do is select a patient-friendly and flexible recovery center like ChoicePoint and begin your journey to sobriety.
How Much Do Medicare Beneficiaries Pay For Mental Health Benefits And Substance Use Disorder Benefits
Inpatient Services
Beneficiaries who are admitted to a hospital for inpatient mental health treatment would be subject to the Medicare Part A deductible of $1,556 per benefit period in 2022. Part A also requires daily copayments for extended inpatient hospital stays. For extended hospital stays, beneficiaries would pay a $389 copayment per day and $778 per day for lifetime reserve days. For inpatient stays in a psychiatric hospital, Medicare coverage is limited to up to 190 days of hospital services in a lifetime. Most beneficiaries in traditional Medicare have supplemental insurance that may pay some or all of the cost sharing for covered Part A and B services.
Outpatient Services
For most outpatient services covered under Part B, there is a $233 deductible and 20 percent coinsurance that applies to most services, including physician visits. However, some specific Part B services have different cost-sharing amounts :
Prescription Drugs
Those with Part D coverage face cost-sharing amounts for covered drugs and may pay an annual deductible and a monthly premium. For example, most Part D enrollees pay less than $10 for generic drugs, but many pay $40-$100 for brand-name drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing.
Read Also: Is Visiting Nurse Covered By Medicare
Medicare Insurance Coverage For Drug & Alcohol Rehab
Medicare is a federal health insurance program that helps people over the age of 65 afford quality healthcare. Does Medicare cover drug and alcohol addiction treatment? Yes, when you need addiction rehab, Medicare healthcare coverage can help with costs and cover at least some parts of your care. Depending on your plan and qualifications, it can make addiction treatment more accessible for those who need it.
This page is meant to help you find out about eligibility and how Medicare can help make the cost of rehab more affordable.
Addiction Treatment For Seniors And Medicare Eligibles
Treatment for addiction is a lot like treatment for any other disease. It starts small, often with preventive measures, and will progress according to the doctors recommendations.
Medicare pays for alcohol and substance abuse treatment for both inpatients and outpatients. Substance use disorders are drug addictions that influence a persons thoughts, feelings, and behaviors.
These disorders arent just limited to illicit drugs, such as Cocaine, Ecstasy, GHB, Hallucinogens, and Heroin, among others. They can also include misuse of legal drugs like nicotine, marijuana, or alcohol as well as legal medications like fentanyl , hydrocodone , or oxycodone .
The American Society of Addiction Medicine divides treatment into five levels of care. Heres how they relate to Medicare:
Level 0.5, Early Intervention Education and prevention for people who are at risk of developing an addiction fall under this level. Medicare can cover a conversation with your doctor about a prescription drug that may be habit-forming.
Level 1, Outpatient Treatment This level of addiction treatment refers to nine hours or less of weekly counseling services or recovery. Outpatient mental health services fall under Medicare Part B and certain Medicare Advantage plans.
Level 2, Intensive Outpatient and Partial Hospitalization
A doctor must say that PHP is medically necessary, and your treatment plan must include at least 20 hours of treatment per week.
PHP services can include:
Level 3, Inpatient Treatment
Recommended Reading: Does Medicare Need Pre Authorization
Prevalence Of Substance Abuse In Older Adults
Older adults most commonly abuse alcohol, but many also abuse prescription and illegal drugs. The percentage of older adults who met the criteria for having an addiction problem was 11.7 percent.
Drug abuse in adults older than 65 years is mainly limited to alcohol despite the prevalence of so many illicit drugs and mood-altering prescription drugs.
Inpatient Vs Outpatient Treatment And What Youll Pay
This article is reprinted by permission from NerdWallet.
Medicare does provide coverage for treatment of substance use disorders. But there are a wide variety of approaches, and Medicare pays for only the therapeutic services it considers reasonable and necessary. So its important to confirm with care providers, programs and pharmacies that Medicare reimburses them for their services.
More: How to pay for healthcare costs in retirement
Nearly 1 million Americans 65 and older were reported as living with a substance use disorder in 2018, according to federal data. Deaths attributed to opioid overdose more than doubled among those 55 and older from 2012 through 2019, as reported by the Kaiser Family Foundation, a health policy nonprofit.
And provisional data released this week by the National Center for Health Statistics indicates that, overall, drug overdose deaths in the U.S. increased nearly 30% in 2020 from 2019.
Outpatient treatment
Medicare Part B, which covers doctor bills and related services, pays for a yearly alcohol misuse screening for people who drink but dont meet the criteria for alcohol dependency. If your primary care doctor finds that youre misusing alcohol, Medicare will cover four counseling sessions annually. If needed, a primary care doctor can refer you for specialized treatment.
Inpatient treatment
What youll pay: Outpatient
What youll pay: Inpatient
Other coverage options
More From NerdWallet
Read Also: Does Medicare Cover Dtap Vaccine
Medicare Advantage Coverage For Substance Abuse
Those with Medicare Advantage coverage have access to substance abuse treatment. Its essential to use an in-network doctor, or you risk paying out-of-pocket. Some Special Needs Plans help people with specific chronic issues such as mental health or substance abuse. Options for plans vary by county.
Contact your health plan to find an in-network specialist.
How Long Does Medicare Pay For Rehab
Part A pays the full cost of 60 days of inpatient rehab in a semi-private room. For days 61 to 90, the coinsurance cost increases each day. After the 90th day, the coinsurance amount doubles, and you begin using lifetime reserve days.
Medicare only allows 60 lifetime reserve days. If youve been inpatient for over 90 days and you dont have lifetime reserve days, Medicare wont pay for care.
A supplement plan can extend the number of days you have hospitalization coverage. If you get inpatient care at a psychiatric hospital, Medicare covers 190 days of lifetime care.
The limit on lifetime days is a problem if you need intensive mental health services or suffer a relapse. The limitation doesnt apply to care in a general hospital. For most people in rehab, an inpatient stay is the beginning of the journey. After discharge, Part B will continue to pay for counseling and medical care needed to stay on track.
Read Also: Will Medicare Pay For My Nebulizer
Addiction Treatment Under Medicare Part B
Medicare Part B is designed to assist in paying fore the costs associated with outpatient treatment for drug and alcohol rehabilitation. Programs covered under Part B do not require residence in a treatment facility.
Under Part B, a physician must certify that a Medicare beneficiary requires the treatment they receive, including partial hospitalization programs. Services offered as part of partial hospitalization programs often include the following:
- Individual and group therapy
- Therapeutic drugs that cannot be self-administered
- Medically necessary diagnostic services for mental health
In addition, Medicare Part B may cover alcohol misuse assessment once per year if you are an adult who does drink but does not meet the criteria for an alcohol use disorder.
