Does Humana Cover Home Health Care
- Some Humana Medicare Advantage plans can cover home health care services such as care managers, home meal delivery, medical transportation, prescription drug deliver, caregiver support and more. Learn more and find a Humana Medicare plan that offers the home health benefits you need.
Many Humana Medicare Advantage plans may cover home health care and other benefits designed to help seniors age in place at home. Plan benefits and availability can vary, so its a good idea to compare plan details online or call to speak with a licensed insurance agent who can help you find out what benefits are offered by Humana Medicare plans available where you live.
Many Medicare beneficiaries who choose to enroll in a Medicare Advantage plan typically might do so because of the extra benefits that many of these plans may offer that are not included in Original Medicare .
Some Humana Medicare Advantage plans may cover home health care along with prescription drugs, dental, vision, hearing, transportation, home meal delivery and more, all of which arent available with Original Medicare coverage.
Medicare Covers Home Care Services Under Medicare Parts A And B
Both Medicare Part A and Part B cover a range of home care services, but its important to understand the differences of what each plan covers.
For example:
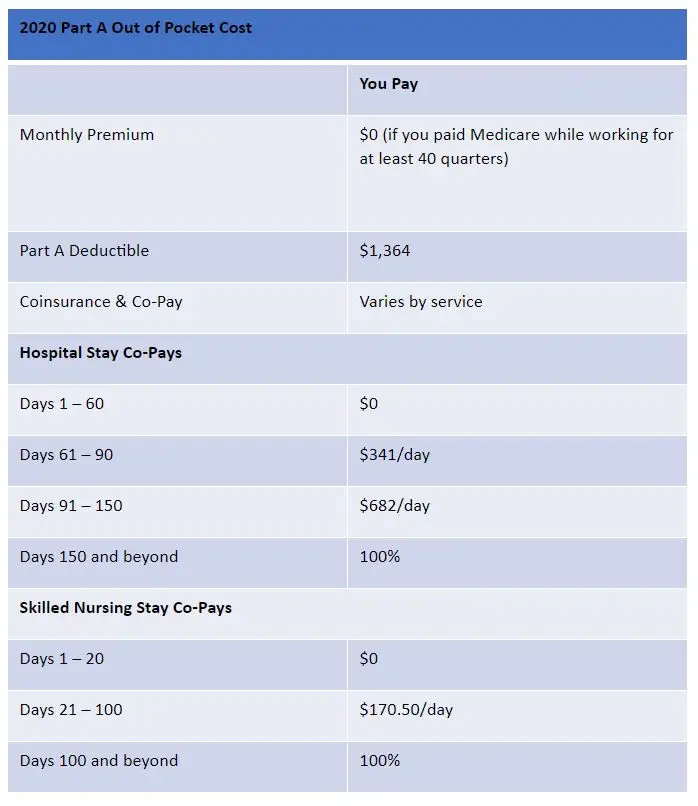
Medicare Part A Covered Home Care ServicesUnder Part A , you can be covered for home care services if you had to spend a minimum of 3 consecutive days at the hospital as an inpatient, or had to have a skilled nursing facility stay of the same duration. In this case, you may still require skilled nursing care and therapy at home. Medicare Part A covers the first 100 days of home health care services provided that you meet the eligibility requirements of being essentially homebound and needing skilled care to recover from the injury, illness or condition that precipitated the hospital stay. Its also important that you start receiving these home care services within a 14-day time frame from your stay at the hospital or SNF.
Medicare Part B Covered Home Care ServicesIf you require home health services beyond 100 days, Medicare Part B can cover these services.
Your doctor should then sign a home health certification that designates which specific home health care services you need, why you need them, for how long, and what the desired outcome should be. Your home healthcare agency can then create a plan of care that meets those requirements outlined by your doctor.
See What Our Customers Say..
They are always here for me…
A. Khatib K. Manassas, VA
Original Medicare Vs Medicare Advantage When It Comes To Home Care
To properly understand the differences between Original Medicare and Medicare Advantage plans when it comes to home care, it is important to first understand the difference between the two coverage options themselves:
People may receive their Medicare in two different forms, Original Medicare or via a Medicare Advantage plan.
Read Also: Can A 60 Year Old Get Medicare
You May Like: Does Usaa Have Medicare Supplement Insurance
Finding A Home Health Care Agency
If you are interested in home health care after a stay in the hospital, or as an alternative to a stay in a hospital or nursing facility, contact a home health care agency recommended by your doctor or the hospital discharge planner. The discharge planner can even contact an agency for you. You may also get help in locating home health care agencies from a community health organization, visiting nurses association, United Way, Red Cross, or neighborhood senior center. Medicare.gov lists home health care agencies in your area and allows you to compare the quality of their service depending on past performance.
Medicare Has Special Rules Defining How Long And How Often You Receive Home Care Services
One of the defining features of home care services as they relate to Medicare is that they must be received fewer than 8 hours a day, over less than 7 days per week. Those hours of care cannot exceed 28 hours per week, or over a period longer than 21 days.
With that being said, if your doctor declares that you still need home health care after 21 days, then you can continue to receive it for as long as you need it.
Don’t Miss: Which Medicare Advantage Plans Cover Massage Therapy
Does Medicare Cover Home Health Aides
Medicare covers home health aides as part of a physician-ordered plan of care for you in your home if the following requirements are met:
- You also have other skilled services in the home, such as nursing, physical therapy, occupational therapy, or speech-language pathology.
- You are receiving home health services from a Medicare-approved home health agency that complies with federal and state regulations governing home health aides.
- Home health aides providing services meet all federal and state requirements and are supervised by a skilled professional.
- Home health aide services are part-time or intermittent and match the amount, frequency, and duration established by the physicians plan of care.
- Home health aide services are reasonable and necessary to the treatment of your illness or injury.
- Home health aides providing services are certified or licensed, in good standing with your states regulatory agency, and operate within their scope of practice and level of training and competency.
- Compared to skilled nursing services, home health aide services do not exceed eight hours per day and 35 hours per week.
What If Medicare Wont Cover All My Physical Therapy
Medicare no longer caps how much medically necessary physical therapy it will cover throughout the year. But in some cases, doctors might recommend physical therapy beyond what Medicare considers medically necessary. In this case, you may be stuck paying for additional treatment sessions out of your own pocket.
To help pay these costs, you could turn to Medicaid, which helps some low-income people, pregnant women, and families cover their health care costs.
Otherwise, consider switching from Original Medicare to Medicare Advantage. Many Medicare Advantage plans cover more services than Original Medicare, so you could find a plan that pays for more physical therapy.
You May Like: What Is The Annual Deductible For Medicare
You May Like: How Do I Stop Medicare Junk Mail
Home Health Change Of Care Notice
The home health agency must also give you an ABN or a HHCCN when they reduce or stop providing home health services or supplies because of one of these:
- The home health agency makes a business decision to reduce or stop giving you some or all of your home health services or supplies.
- Your doctor changed your orders, which may reduce or stop giving you certain home health services or supplies that Medicare covers.
The HHCCN lists the services or supplies that will be changed, and it gives you instructions on what you can do if you dont agree with the change.
The home health agency isnt required to give you a HHCCN when it issues the Notice of Medicare Non-coverage .
How Else Can I Get Or Pay For Home Health Care
Unfortunately, Medicare does not entirely cover home health care because Medicare only covers part-time or intermittent skilled nursing care that your doctor deems medically necessary.
If you need long-term help at home, you can enroll in private long-term care insurance. However, since they are not under Medicare, you will have to pay on your own.
However, if you have limited income or assets, you may qualify for Medicaid, depending on your states rules. With Medicaid, you can access certain health care services Medicare does not cover. There are also home and community-based service waiver programs that offer skilled nursing care.
You May Like: How Is Medicare Part B Penalty Calculated
Will Medicare Cover Skilled Nursing Care
Medicare will pay for whats considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
Skilled nursing services are generally required to treat an illness or assist in the recovery of an injury. As the name implies, those who provide this care are licensed to administer medical treatment such as injections, catheter changes, wound dressings, and tube feedings.
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it wont cover 24-hour-a-day care.
How To Enroll In Medicare
Enrolling in Medicare is easy once you understand how to do so. Its important to know that how you enroll in Medicare Part A and Part B is different from how you enroll in Medicare Advantage , Part D or Medicare supplement insurance.
See the table below for a quick overview of how to enroll in a Medicare or Medigap plan and read on for how-to steps for both Original Medicare and the three kinds of Medicare and Medigap plans.
Original Medicare Medicare Advantage plan Medicare Prescription Drug plan Medicare Supplement Insurance plan How to Enroll
Enroll in Original Medicare online at the Social Security website or by calling or visiting your local Social Security office.
Enroll directly in the plan e.g., on the plans website or Medicare.gov .
Enroll directly in the plan e.g., on the plans website or Medicare.gov .
Enroll directly in the plan e.g., on the plans website
Original Medicare
How to Enroll
Enroll in Original Medicare online at the Social Security website or by calling or visiting your local Social Security office.
Medicare Advantage plan
Enroll directly in the plan e.g., on the plans website or Medicare.gov .
Medicare Prescription Drug plan
Enroll directly in the plan e.g., on the plans website or Medicare.gov .
Medicare Supplement Insurance plan
Enroll directly in the plan e.g., on the plans website
You May Like: Does Medicare Cover Portable Nebulizers
Qualifying For Home Health Coverage
To be eligible for Medicare home health benefits, you must meet all of these conditions:
- You are homebound. That means you are unable to leave home without considerable effort or without the aid of another person or a device such as a wheelchair or a walker.
- You have been certified by a doctor, or by a medical professional who works directly with a doctor , as being in need of intermittent occupational therapy, physical therapy, skilled nursing care and/or speech-language therapy.
- That certificationarises from a documented, face-to-face encounter with the medical professional no more than 90 days before or 30 days after the start of home health care.
- You are under a plan of care that a doctor established and reviews regularly. The plan should include what services you need and how often, who will provide them, what supplies are required and what results the doctor expects.
- Medicare has approved the home health agency caring for you.
Are You Automatically Enrolled In Medicare When You Turn 65
Yes. If you are receiving Social Security, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. Social Security will send you sign-up instructions at the beginning of your initial enrollment period, three months before the month of your 65th birthday.
You May Like: Do You Have To Get Medicare At 65
Recommended Reading: Is It Mandatory To Sign Up For Medicare At 65
Improve Medicare For All Beneficiaries
Medicare is extremely popular, but it needs attention to ensure all beneficiaries receive comprehensive coverage and equitable treatment. The Medicare program that Americans know and cherish has been allowed to wither. Traditional Medicare, preferred by most beneficiaries, has not been improved in years, yet private Medicare Advantage plans have been repeatedly bolstered. Its time to build a better Medicare for all those who rely on it now, and will in the future.
Does Medicare Cover Home Health Aides In Florida
If youre struggling to understand Medicare in Florida, Connie can help. Ask Connie your question, and a local, licensed agent will help you navigate your Medicare journey. Complete this form to have your question answered. It could be featured on Dear Connie.
Dear Connie,
My husband has multiple chronic conditions. While we have specialists coming to the house to support him, I hope to get help with his daily personal care needs. Its become overwhelming for me to manage. Im wondering, does Medicare cover home health aides in Florida?
Seeking help,Shirley from Spring Hill, Florida
Find the right Medicare plan for you
Im so happy youre reaching out and seeking the support you need.
Yes, Medicare covers home health aides under certain conditions.
For example, if you were only seeking a home health aide and there werent other services being provided in the home, your husband would not be eligible. Home health aides are not offered as a stand-alone service through Medicare.
Agent tip:
Home health aides are not offered as a stand-alone service through Medicare. To qualify, the Medicare beneficiary must also be receiving in-home skilled care.
However, since it sounds like your husband is receiving either skilled nursing care, physical therapy, occupational therapy, speech-language pathology, or other home health services, hed likely qualify.
Don’t Miss: Does Medicare Part B Cover Eye Exams And Glasses
Who Can Receive Home Care Covered By Medicare
Individuals must have coverage through Medicare Part A and/or Medicare Part B and meet the following four criteria as set forth by Medicare.gov:
You May Like: Who Does Not Have To Pay For Medicare Part B
What You Pay For Home Health Services
All eligible Medicare recipients pay the following for home health services:6
- $0 for home health services
- 20% of the Medicare-approved amount for like a walker, wheelchair or hospital bed
Before home health care begins, your home health agency should explain your bill. This includes what Medicare will help cover, what Medicare wont cover and how much youll owe . The details of what isnt covered by Medicare must be given to you in an before you receive any uncovered items or services.7
Recommended Reading: How To Qualify For Medicare In Ga
What Types Of In
If your situation meets Medicare criteria, Medicare may cover in-home health care such as:
- Skilled nursing care
- Part-time home health aides
- Medical social services
Medicare benefits might also cover:
- Durable medical equipment
- Medical supplies
- Injectable osteoporosis drugs
If you qualify for home health care under Medicare, you generally dont have to pay any coinsurance or copayment. If you need durable medical equipment, youll typically pay 20% of the Medicare-approved amount as coinsurance. Read more about Medicare and durable medical equipment.
How To Get Approved For In
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care, and they include the following:
You must be under the care of a doctor:
The primary step in getting approved for in-home care is that you and the nursing plan must be under the care of a Medicare-approved doctor. This doesnt mean that the doctor will be at every visit. A home health nurse specialist will administer your plan, which your will create and regularly review.
Youre homebound:
This is when youre unable to leave your house for treatment. Homebound patients require assistance from a person or piece of durable medical equipment such as a walker or wheelchair to get around the home or to get to services outside the home. Immobile people are considered homebound as well. A doctor can deem that youre homebound if he or she believes that your illness or condition could get worse if you left the home.
You doctor certifies that you need home care:
You dont need round-the-clock care:
Your in-home care comes from an approved home health agency:
MORE ADVICE
You May Like: How To Register For Social Security And Medicare
What Durable Medical Equipment Is Covered By Medicare
The cost of durable medical equipment is covered by Medicare if it is deemed medically necessary, and has been prescribed by a doctor for use at home. The list of covered durable medical equipment includes:
- Blood sugar monitors.
You will pay 20% of the Medicare-approved amount for the equipment, and you will be liable for any remaining deductible under Medicare Part B.
Medicare Coverage Of In
In-home health care may be covered if its medically necessary. It must also be part-time or intermittent, which rules out full-time and long-term care in the home. Home health services such as skilled nursing care, home health aide services, physical and occupational therapies and medical social services are covered by Part A and/or Part B.
Medicare doesnt cover non-medical care and services provided in the home, including meal deliveries. Homemaker services and personal care, such as help with chores and assistance with the activities of daily living, may be covered only when provided alongside other medically necessary care.
Donât Miss: How Do I Know What Medicare Coverage I Have
Don’t Miss: Does Medicare Part B Cost The Same For Everyone