How Does Medicare Cover Counseling
Medicare Part BMedicare Part B is medical coverage for people with Original Medicare benefits. It covers doctor visits, preventative care, tests, durable medical equipment, and supplies. Medicare Part B pays 80 percent of most medically necessary healthcare… covers many different outpatient mental health services:Medicare.gov, Mental health care , Accessed November 3, 2021
Medicare Part AMedicare Part A is hospital coverage for Medicare beneficiaries. It covers inpatient care in hospitals and skilled nursing facilities. It also covers limited home healthcare services and hospice care…. provides coverage for counseling services as part of treatment in an inpatient facility, such as a general hospital or psychiatric hospital.Medicare.gov, Mental health care , Accessed November 3, 2021
How Can I Get Help Paying For A Caregiver
If you or your loved one have exhausted your financial resources paying for in-home caregivers, you may be eligible for both Medicare and Medicaid.
Every state has at least one home- and community-based health services waiver program. If you meet the eligibility guidelines, this type of waiver program could help you pay for things like:
- adult day care
- help with daily personal care
- modifications to your home
- help with housekeeping
If you think you or someone in your family might need custodial care, you may want to consider a long-term care insurance policy to help you cover the cost.
A Medicare supplement plan may also help you pay some of the costs that Medicare wont cover.
Differences Between The Medicare Hospice Benefit And Regular Medicare
- Medicare hospice coverage is limited to beneficiaries who are terminally ill.
- Hospice coverage is for pain and symptom management and comfort, not for curative treatment of the underlying terminal illness.
- Hospice coverage is holistic. Not only is medical care covered, but so are social work services, chaplain services, bereavement services and homemaker services.
A Comparison of Medicare Home Health Benefits and Hospice Benefits
| Service | |
| Not Covered | Covered, during periods of medical crisis |
¹ There are additional services that can be provided in the home, but are not included in the home health benefit. Medicare will pay for reasonable and necessary home health visits if all the following requirements are met: 1. Patient needs skilled care 2. Patient is homebound 3. Care is authorized by physician and 4. Home Health agency is Medicare-certified. .² Medicare will pay for hospice care if all the following requirements are met: 1. Prognosis that life expectancy is 6 months or less. 2. Terminal illness is certified by physician 3. Patient elects hospice benefit 4. Care is specified in the hospice plan of care and 5. Hospice program is Medicare-certified. .
You May Like: When Can I Enroll For Medicare Part B
Does Medicare Cover Hospice At Home
Admittedly, hospice may not be a pleasant topic to discuss, but it behooves all of us to understand what this benefit offers and the coverage available to Medicare recipients.
What is Hospice?As explained by the Hospice Foundation of America, hospice offers medical care of another kind not to restore good health but rather to maintain or enhance quality of life for those with a terminal condition. With this program, an individualized care plan is developed and kept current for each patient. The plan extends beyond physical pain to address the spiritual and emotional anguish that is inevitably an outcome of terminal illness. Additionally, hospice care supports the caregiver throughout the caring period and later serves as a pillar for grief support.
Eligibility for Hospice Care Medicare BenefitsRecipients of Medicare Part A, which is the hospital insurance component of Medicare benefits, are eligible for hospice care if they submit the appropriate documentation. This includes a physician certification that states the Medicare recipient is terminally ill with a life expectancy of six months or less acceptance of palliative care, which is care to comfort versus cure and a signed statement to confirm that hospice care has been chosen over other Medicare-covered benefits to treat the illness or related conditions.
Related articles:
How Long Can You Get Hospice Care
If youve been in hospice for six months, you can continue to receive hospice care, provided the hospice medical director or hospice doctor reconfirms your terminal illness at a face-to-face meeting.
If you have other health issues that arent related to your terminal illness, Medicare will continue to pay for covered benefits, but generally, hospice focuses on comfort care.
Under your hospice benefit, youre covered for hospice care for two 90-day benefit periods followed by an unlimited number of 60-day benefit periods. At the start of every benefit period after the first, you must be recertified as terminally ill.
Read Also: Can You Get Medicare If You Live Outside The Us
What Are The Medicare Requirements For Inpatient Hospice Coverage
Medicare requirements for inpatient hospice coverage include:
- Your doctor or specialist certifies that you have a life expectancy of six months or less.
- You choose comfort care instead of curative treatments.
- You are experiencing severe pain and symptoms that would best be treated in an inpatient center rather than at home or in a nursing home or assisted living facility.
Does Medicare Pay For Skilled Nursing Care During Hospice
Does Medicare pay for hospice care in a skilled nursing facility? Strictly speaking, Medicare does not pay for skilled nursing care because someone is in hospice, but many times there are other triggering events that cause Medicare to cover skilled nursing care. For example, someone who is in hospice falls and breaks a hip. That situation would justify skilled nursing care. A person develops an infection or pneumonia that results in hospitalization. The patient is transferred to a skilled nursing facility to continue the care. In those ways, skilled nursing and the custodial care that accompanies it are available.
Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mothers Medicare plan took excellent care of her and us. I am grateful for such a wonderful program and the insurance that worked with Medicare.
You May Like: Do Medicare Advantage Plans Have Dental Coverage
How Do You Pay For Hospice Care
For those not eligible for Medicare or Medicaid, payment for hospice can come from private insurance or an HMO, since these also include a hospice benefit.
Hospices employ financial specialists to help families who do not qualify for federal assistance and do not have insurance find available resources. The payment options for these families include self-pay and charitable organizations.
Facing a terminal illness brings with it many concerns. Paying for end-of-life care shouldnt be one of them.
Coverage For Hospice Care
- Nurse visits
- Bereavement support
- * Arts services
* Connecticut Hospice covers all costs of Arts services, which are not reimbursed to us by Medicare.
You must still pay your regular Medicare Part A and B premiums, and any other care that is unrelated to the terminal illness will continue to be covered.
Also Check: What Is Blue Cross Blue Shield Medicare Advantage
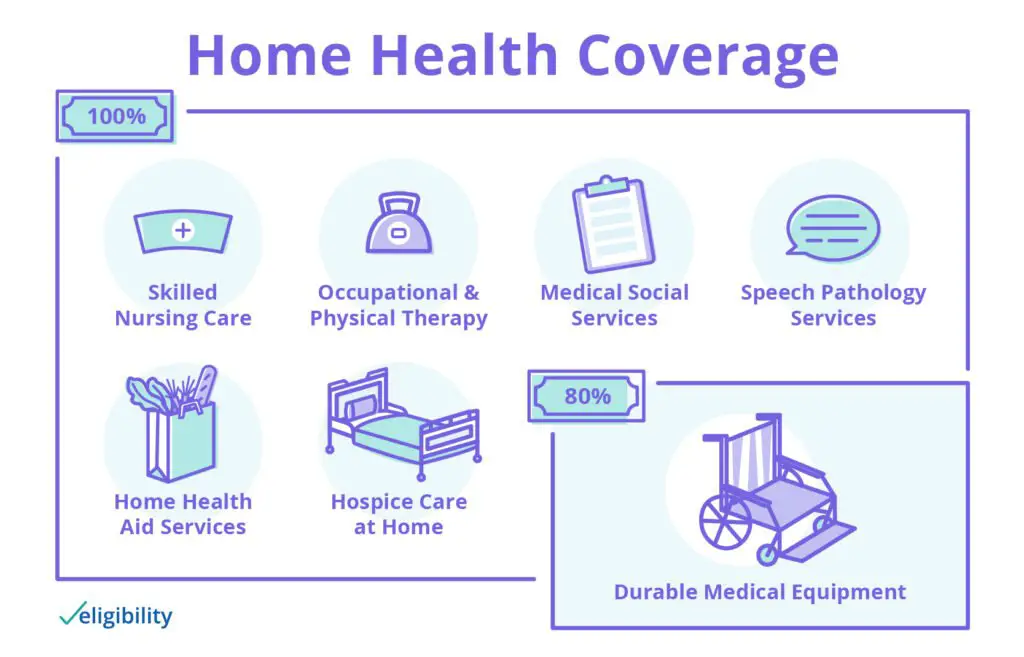
How To Pay For In
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that wont be covered by Medicare. This is where supplemental insurance comes in.
You may have already heard of Medigap insurance, which you purchase to help pay for all the medical costs that Medicare doesnt, like copayments, deductibles, and premiums. Its also a useful source to have when it comes to in-home care. Supplemental insurance could help cover the costs that you may accrue, like personal care, meals delivered to your home, and the remaining costs of your DME.
If you have any questions regarding your in-home care and what is covered by Medicare, contact your local Social Security office.
Level : Continuous Home Care
Continuous home care is for times of crisis when you need a higher level of nursing care. These services may make it easier for you to stay in your home even when your symptoms get more severe.
Continuous home care means you need a nurse for at least eight hours in a 24-hour period. You may also be receiving help from other hospice team members at the same time, but at least half the care must be supplied by a nurse.
Also Check: Do You Have Dental With Medicare
Who Pays For Hospice Care At Home
The Medicare Hospice Benefit covers end-of-life services related to a patients terminal diagnosis in whatever setting the patient calls home, whether thats a traditional residence, an assisted living facility, or nursing home. Wherever hospice occurs, all services related to the terminal diagnosis are covered up to 100% by Medicare Part A.
If the patients symptoms cannot be managed by the routine level of hospice care, additional levels of service, such as 24/7 continuous care or inpatient hospice care, will also be financed through Medicare Part A at no additional expense to the patient or family.
Covered Medicare Hospice Services

- Youre eligible for Original Medicare Part A .
- Your doctor and the hospice medical director certify that youre terminally ill and have six months or less to live if your illness runs its normal course.
- You sign a statement choosing Medicare hospice care instead of other Medicare-covered benefits to treat your terminal illness.
- You get Medicare hospice care from a Medicare-approved hospice program.
Medicare hospice services that are typically covered when theyre needed to care for your terminal illness and related condition include:
- Physician services
- Nursing care
- Medical supplies and equipment
- Prescription drugs for symptom control and pain relief
- Nutritional counseling social worker services and grief counseling for you and your family
- Medicare hospice aide and homemaker services
- Short-term inpatient care
- Short-term respite care
- Other Medicare-covered services needed to manage your pain and other symptoms related to your terminal illness, as recommended by your Medicare hospice team
If you would like to learn more about your Medicare hospice coverage and options, I would be pleased to help you.
- You can use one of the links below to set up a phone call with me or request personalized information from me by email.
- You can also do some research on your own to get familiar with Medicare plan options in your area by clicking on the Compare Plans button on this page.
New To Medicare?
Don’t Miss: How To Reorder Medicare Card
Does Medicare Ever Cover Respite Care In The Home
Medicare defines respite care as temporary care in a facility such as a nursing home to give the caregiver some time off. Generally, respite care for a dementia patient isnt covered early on.
Medicare typically does cover respite care as part of the hospice care benefit under Part A. According to the National Institute on Aging , Alzheimers is a terminal illness with recognizable end-of-life symptoms. You are generally eligible for hospice and respite care if your health-care provider certifies you are approaching the end of life and you agree to comfort care instead of medical treatment, and sign a statement with Medicare confirming that decision.
If you qualify for the hospice benefit, you pay nothing for your eligible home health-care services, including short-term respite care provided in a nursing home or hospice inpatient facility. Although the hospice benefit doesnt cover adult day care services, it does cover inpatient respite care you may be asked to pay 5% of the allowable charges.
Medicare Transportation For Hospice Patients
When a loved one has been diagnosed with a terminal illness, an extremely challenging road often lies ahead. Along with coping with grief and making appropriate arrangements, many difficult decisions need to be made.
Navigating the healthcare landscape and determining what services are and are not covered for a person on hospice care can certainly feel overwhelming.
All individuals with Medicare Part A coverage are entitled to receive hospice care at no cost once they select a provider. This includes transportation services related to the hospice diagnosis.
According to the Medicare Benefit Policy Manual, Ambulance transports of a hospice patient, which are related to the terminal illness and which occur after the effective date of election, are the responsibility of the hospice.
While transportation benefits normally fall under Medicare Part B, when a patient is put on hospice, Part A takes precedent. Importantly, along with ambulance services, this coverage also provides for wheelchair van transportation, while Part B does not.
For a patient on hospice at home or in a facility, comfort and minimization of pain are the primary concerns. The goal is to give the patient the highest possible quality of life during the time they have left. The hospice care team, which includes the physician, the patients family, and the supporting medical staff, will collaboratively make decisions on the best course of palliative care.
You May Like: Does Medicare Pay For Mobility Scooters
Does Medicare Require People To Give Up Dialysis For Hospice
Dialysis is a life-sustaining treatment for people with end-stage renal disease . Treatments usually last four hours and are done three times per week. People who have lost 85% or more of their kidney function and who quit dialysis usually have about one week to live. Then why would Medicare require people to give up dialysis to receive hospice, and, if that is the case, is there a way around this rule?
Do Medicare Advantage Plans Or Medicare Supplement Plans Cover Adult Day Care
Medicare Advantage and Medicare Supplement plans are provided by private insurance companies approved by Medicare, which means they are able to determine what coverage they will offer plan enrollees. Medicare Advantage plans must cover everything included in Original Medicare , but they may offer additional benefits for adult day care. Consult the plan information documents of the plans you are interested in for more information.
Keep in mind that all plan types and benefits may not be available in all locations and you must continue to pay your Part B premium if you enroll in Medicare Advantage, plus any additional premiums required by your plan.
Long-term care insurance and Veterans Administration policies may also help cover costs associated with adult day care.
Would you like more information about Medicare and adult day care or respite care services for dementia? I am happy to answer your questions. If you prefer, you can schedule a phone call or request an email by clicking on the buttons below. You can also find out about plan options in your area by clicking the Compare Plans button.
The product and service descriptions, if any, provided on these Medicare.com Web pages are not intended to constitute offers to sell or solicitations in connection with any product or service. All products are not available in all areas and are subject to applicable laws, rules, and regulations.
New To Medicare?
Also Check: What Weight Loss Programs Are Covered By Medicare
Are There Other Programs Available To Help With Adult Day Care Expenses
Programs of All-Inclusive Aid for the Elderly is a joint program between Medicare and Medicaid. It is designed to help older adults stay in their homes instead of entering nursing home care. PACE programs might pay for all services covered by Medicare and Medicaid that your doctor believes are medically necessary for your care, including but not limited to:
- Adult day care
- Other specialty medical care and therapies
To qualify for PACE, you must:
- Be age 55 or over
- Be enrolled in Medicare, Medicaid, or both
- Live in a PACE service area
- Need a nursing-home level of care, according to your doctor
- Be able to safely stay in your home with the appropriate support services
You can find out if theres a PACE program in your state and if youre eligible for services on the PACE program page on Medicares website.
Does Medicare Cover Hospice
The term hospice refers to treatment, services, and care for people who have an illness and are not expected to live longer than 6 months.
Making decisions about hospice care, whether for yourself or someone you love, is not easy. Getting direct answers about what hospice costs and how you can pay for it may make a difficult decision a little clearer.
Original Medicare does pay for hospice care, as long as your hospice provider is enrolled in the program and accepts Medicare coverage. A Medicare Advantage plan will also cover hospice care.
If youre looking for specific answers about which hospice facilities, providers, and services are covered under Medicare, this article will help you answer those questions.
Medicare covers hospice once a medical doctor certifies that you have an illness that makes it unlikely you will live longer than 6 months.
To get this coverage, you must sign a statement that confirms:
- you want palliative care
- you dont intend to continue seeking treatments to cure the illness
- you choose hospice care instead of other Medicare-approved services to treat your illness
If you are receiving hospice care, that means your doctor has certified that your life expectancy is 6 months or less. However, some people defy expectations.
Recommended Reading: What Does Medicare Part B
Finding A Hospice Program
Consider these questions when choosing your hospice care providers:
- Is the hospice provider certified and licensed by the state or federal government?
- Does the hospice provider train caregivers to care for you at home?
- How will your doctor work with the doctor from the hospice provider?
- How many other patients are assigned to each member of the hospice care staff?
- Will the hospice staff meet regularly with you and your family to discuss care?
- How does the hospice staff respond to after-hour emergencies?
- What measures are in place to ensure hospice care quality?
- What services do hospice volunteers offer? Are they trained?
A hospice doctor is part of your medical team. You can also choose to include your regular doctor or a nurse practitioner on your medical team as the attending medical professional who supervises your care.
In addition, a hospice nurse and doctor are on-call 24 hours a day, 7 days a week, to give you and your family support and care when you need it.