Does Medicare Cover Other Sleep Disorders
Currently, Medicare covers sleep studies if you exhibit symptoms of OSA, but those can also overlap with symptoms of other sleep disorders. If youre diagnosed with narcolepsy or insomnia, your doctor can prescribe you medication. For medication, you will need to be enrolled in a Medicare Part D Drug Plan, which you can be enrolled in on its own or as an additional Plan with your other Medicare Coverage . Under Part D, youll need to meet the current monthly deductible of $415.
Your copay will depend on the drug youre being prescribed. Prescription drugs as listed in a drug formulary categorizing drugs into different tiers. Drugs in Tier 1 are for generics and have lower copayments. Tiers 2 to 5 are brand-name and specialty drugs requiring higher out-of-pocket payments.
The Working Parts Of An Insurance Plan
DeductiblesThe deductible is the amount you pay out of pocket for medical expenses before your insurance companys coverage kicks in.
If you have a deductible of $1000 and you havent had any other services performed prior to your sleep study, you will usually need to pay down that $1000 deductible. After that, your insurance company begins to reimburse, with those amounts depending on your policy, whether youve stayed in network and whether you have coinsurance.
CoinsuranceThis is the percentage you will still pay on medical services after the deductible has been satisfied. Usually this is an 80/20 split: the insurance company pays 80 percent of the final bill, and you pay the rest up to a predetermined maximum. Check your policy to figure out what your coinsurance percentages are.
CopaymentCopayment usually applies to prescriptions and office visits, but some insurance companies may ask you to pay a small fee before having a sleep study. Again, you will need to consult your insurance carrier to see if they have any front-end fees youll need to pay first.
Out-of-pocket limitsThis term refers to the total amount you will actually pay for covered expenses in any given year. First you pay your deductible, then you pay your coinsurance percentage up to a predetermined amount. After you reach that limit, you have maxed out your out-of-pocket limit, and then your insurance company usually covers all expenses at 100 percent.
Where Can I Get An Oral Appliance For Sleep Apnea
Contact Dr. Jeffrey W. Cross, D.D.S., F.A.G.D., for more information about obstructive sleep apnea treatment that goes beyond a CPAP machine. Since 2005, Dr. Cross has utilized oral appliance therapy and mouthpieces to treat sleep apnea patients. He is a member of the American Academy of Dental Sleep Medicine as well as the Academy of Clinical Sleep Disorders Disciplines. Dr. Cross has completed hundreds of hours of continuing education and is highly experienced in his field.
Contact Dr. Crosstoday at for a better nights sleep to learn more about treating your sleep apnea with a mouthpiece.
You May Like: Who Gets Medicare Part D
Your Cost For A Sleep Study Under Medicare
Sleep studies are considered a diagnostic test and must be ordered by your doctor to qualify for Medicare coverage.
Sleep studies are covered by Medicare Part B. You will owe 20 percent of the Medicare-approved cost of the study, and the Part B deductible applies.
You may owe less if you have supplement insurance, such as Medicaid or a Medigap policy.
If youre enrolled in a Medicare Advantage plan, you may be restricted to sleep centers and clinics within your plans provider network.
Does Medicaid Cover Cpap Treatment
The most effective treatment for sleep apnea is the use of a continuous positive airway pressure, or CPAP, machine. These machines deliver constant and steady air pressure to your airway as you sleep through a hose connected to a mask. In general, Medicaid does cover this sleep apnea treatment.
If youre diagnosed with sleep apnea according to Medicaids criteria, the program will cover an initial 12-week period of CPAP treatment. Medicaids criteria determines how severe your sleep apnea is based on your apnea-hypopnea index . This index measures how often your breathing is interrupted each hour.
If your condition improves during the 12-week period and youve shown compliance with your usage of the CPAP machine, your treatment will continue to be covered in the future. The improvement of symptoms must be confirmed by your doctor or sleep specialist. The compliance requirement basically ensures that youre using the machine enough to gain benefits. Currently, Medicaid requires that you use the machine for at least 4 hours a night, 70% of nights within the trial period.
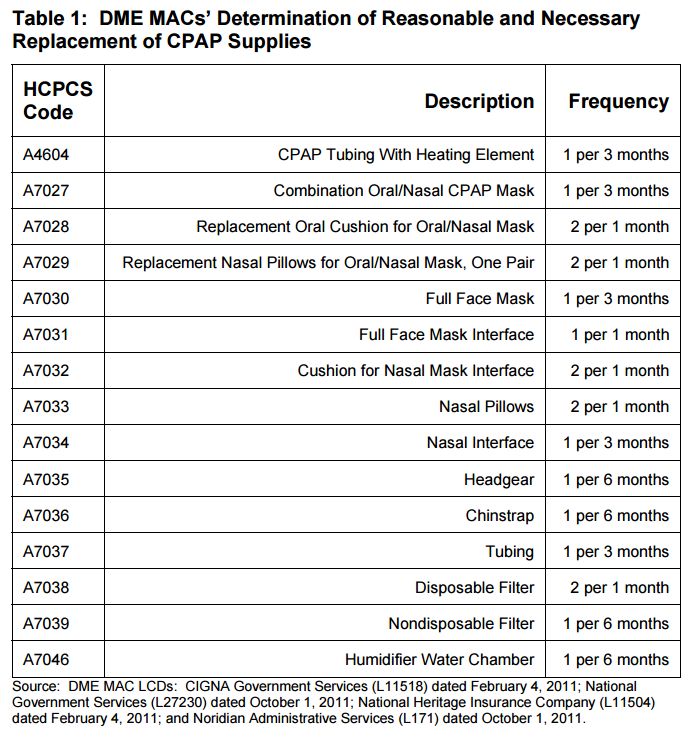
Keep in mind that Medicaids benefits may not cover all costs, and you may need to pay for accessories such as filters and masks.
Don’t Miss: Does Medicare Cover Hospital Bed For Home Use
How Much Will I Have To Pay Out Of Pocket For This Procedure
Every insurance plan is different. Generally, the co-pay costs for Inspire therapy should be similar to co-pays for other out-patient surgical procedures. Some patients may have secondary benefits or supplemental coverage that will offset their co-pay. Your Inspire therapy team will help you through this process.
Patients receiving Inspire experience significant reductions in sleep apnea events and significant improvements in quality of life and daytime functioning. Contact the team of experts at Comprehensive Sleep Care Center to find out if Inspire Sleep Apnea Therapy is right for you.
Repeat Sleep Study Indications
It may be necessary to perform repeat sleep studies up to twice a year for any of the following indications. performed in a healthcare facility is considered medically necessary for persons who meet criteria for attended NPSG in section I above in all other cases, unattended sleep studies are considered medically necessary):
Note: A home sleep study is performed over multiple nights with a single interpretation is considered a single sleep study for purposes of reimbursement.
Also Check: Is Eliquis Covered Under Medicare
Recommended Reading: When Is The Medicare Advantage Open Enrollment Period
How It Is Done
Sleep studies are usually scheduled for evening and night hours in a special sleep lab. But if you usually sleep during the day, your test will be done during the hours you normally sleep. Youll be in a private room, much like a hotel room. For portable sleep monitoring, youll use equipment at home that records information about you while you sleep.
Youll need to be at the sleep lab before the test so the technician can prepare you for the study. You may fill out a form about your sleep the night before. You may also be asked to fill out another form after the study about your sleep during the study.
After the test, you can shower and shampoo your hair to remove the glue from your body. Hair conditioner may help get the glue out of your hair.
Dont Miss: Does Medicare Cover Gastric Bypass Revision
What Are The Criteria For Medicare To Cover An In
Recommended Reading: What Is The Average Premium For Medicare Advantage Plans
Why It Is Done
Sleep studies may be done if your sleep is not restful or if you are tired all day. These studies can help find sleep problems, such as:
- Problems staying awake, such as narcolepsy.
- Problems with nighttime behaviors. These include sleepwalking, night terrors, bed-wetting, and REM behavior disorders .
- Conditions such as periodic limb movement disorder. This is repeated muscle twitching of the feet, arms, or legs during sleep.
- Seizures that occur at night .
- Ongoing problems that have not responded to treatment.
Home Sleep Studies Vs In
Home sleep tests are only used to diagnose sleep-disordered breathing issues, like sleep apnea. By contrast, in-lab sleep studies can help diagnose other sleep disorders, like narcolepsy and periodic limb movement disorders. The difference lies in what the tests measure. Although both tests usually measure factors like airflow, blood oxygen levels, and heart rate, only in-lab sleep studies actually measure sleep by monitoring brain activity.
People often prefer a home sleep study to an in-lab study, since it is less expensive and does not require traveling to the sleep lab. A home sleep apnea test also involves fewer attached devices, so it may feel less invasive. However, since an in-lab sleep study gathers more data, it is more likely to pick up on symptoms of obstructive sleep apnea or other conditions.
If you have a straightforward case of moderate or severe sleep apnea and no other health conditions, then a home sleep apnea test might be right for you. If you have any reason to believe you need a more comprehensive test, then it might be worthwhile to skip the home test and go directly to the sleep lab.
Also Check: How Do You Get Credentialed With Medicare
What Other Sleep Apnea Devices Does Medicare Cover
People who have mild to moderate sleep apnea or cannot tolerate a CPAP machine are good candidates for oral appliances. Like a sports mouth guard, the oral appliance holds the jaw forward in a way that keeps the airway open. Oral appliances are comfortable to wear and are quieter and more portable than CPAP machines.
If a CPAP machine isnt effective in treating your sleep apnea, its possible that a bi-level positive airway pressure, or BiPAP, machine could work for you. BiPAP machines provide more air pressure for inhalation and less for exhalation than a CPAP machine. Medicare will pay for a BiPAP machine if the beneficiary has obstructive sleep apnea and has tried a CPAP machine but hasnt found relief.
Donât Miss: How Do I Cancel Medicare Part A
Does Medicaid Cover Sleep Studies

- If you might have a sleep disorder, your doctor could order a clinical sleep study to learn more. Find out whether Medicaid will cover any costs for a sleep study.
If your doctor believes youâre exhibiting signs of sleep disorders, he may refer you to a polysomnography more widely known as a clinical sleep study. These studies require overnight evaluation to diagnose the severity of your symptoms and how theyâre affecting your sleep continuity, cardiac functions and other factors. This may be in the form of a sleep lab study or a home test. Find out more about whether Medicaid covers sleep studies below.
Read Also: What Is The Requirement For Medicare
Also Check: How To Cancel Medicare Online
When Will Medicare Cover Cpap Machines
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study. Medicare will cover the sleep apnea machine after the initial three-month trial period if your doctorafter meeting youdocuments in your medical record that you meet certain conditions about using the device and that you benefited from CPAP during the initial trial period.
Upon completion of the trial period, you must be re-evaluated to determine whether there is a medical necessity to warrant Medicare coverage of the CPAP machine beyond those initial three months. Medicare wont continue coverage for subsequent months without this re-evaluation.
Is Sleep Apnea Covered By Medicare
If youve been diagnosed with sleep apnea, Medicare Part B may provide coverage for a three-month trial of Continuous Positive Airway Pressure therapy. Coverage may be extended longer if your doctor determines the therapy is helping.
A CPAP machine is a form of positive airway pressure ventilation that provides a constant level of pressure to the upper airway and is used to help treat sleep apnea. Medicare Part B and Medicare Advantage plans will cover the rental of the machine and the purchase of necessary supplies.
Medicare Part D plans and Medicare Advantage plans with prescription drug coverage may cover medications used to treat sleep apnea and other sleep disorders.
You can compare Medicare Advantage and Part D plans online for free, with no obligation to enroll.
You May Like: Does Medicare Part A Cover Urgent Care Visits
Supplemental Medicare Coverage For Sleeping Problems
Although Original Medicare helps cover seniors with certain sleeping disorders, it does not cover everything. If you have been diagnosed with sleep apnea and need additional coverage, you may want to consider a Medicare Supplement Plan .
Get a quote from Medicare.org. We offer free comparisons for Medicare Advantage Plans , Medicare Supplement , and Medicare Prescription Drug Plans. Contact a licensed sales agent at TTY 711 to help you find the right Medicare coverage for your needs.
Home / FAQs / Medicare Coverage / Does Medicare Cover Sleep Apnea
Sleep apnea is a common condition with which many people struggle. Medicare Part B provides coverage for sleep apnea including doctor visits, sleep studies, and equipment to treat the disorder. Depending on the Medicare plan you have, you may be responsible for a portion of the cost.
Medicare And Sleep Studies
Whether youve been told that youre snoring, you find it hard to fall asleep or youre too tired when you wake up in the morning, youre probably worried that you have a sleep disorder. As such, sleep studies are required to discover your problem and work to treat it, so you can go back to sleeping like a baby.
However, you may worry about the costs of such procedures. If you have Medicare or youre planning to enroll in it, you might have asked yourself if it provides any coverage for sleep studies. Read on to learn more about what Medicare covers when it comes to sleep studies.
What Is a Sleep Study?
Its quite difficult to discover a sleeping disorder during a normal doctor visit so, sleep studies are required. Basically, what a sleep study involves is having a doctor monitor you over the course of the night. Through this procedure, the doctor can find out what its causing your sleeping problems, and diagnose things such as insomnia, narcolepsy and more.
It works by having an EEG analyze of your sleeping cycle. If there are any disruptions in your REM and nonREM cycles, the EEG will notice it and help set the diagnosis.
Does Medicare Offer Coverage for Sleep Studies?
Medicare can indeed cover the costs of a sleep study, but it has specific requirements that you need to take into consideration. This is why talking to a healthcare provider is essential before you sign up for it. Basically, you need to find out if Medicare is accepted by your sleep study lab.
Recommended Reading: What’s The Eligibility For Medicare
What Is The Cost Of A Sleep Study With Insurance
Its nearly impossible to capture all of the variations in reimbursement schedules from one insurance payer to the next, especially with so many different avenues for applying insurance benefits .
However, here are some highlights and generalized guidelines for determining if, how, and when your insurer will cover your sleep study.For the purposes of this post, the discussion centers only on private insurance carriers and not CMS/Medicare/Medicaid.
License For Use Of Current Dental Terminology
End User License Agreement:These materials contain Current Dental Terminology , copyright © 2021 American Dental Association . All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled “I accept”, you hereby acknowledge that you have read, understood and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled “I do not accept” and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Recommended Reading: Does Medicare Pay For Laser Cataract Surgery
How Much Do Sleep Apnea Mouthpieces Cost
The expense of a mouthpiece varies depending on the kind of mouthpiece required. The typical cost is between $1,800 and $2,000. These devices may be covered by certain insurance companies or portions of the cost may be reimbursed. Its critical to discuss this with your insurance company to discover whether youre eligible for any discounts on oral devices.
Is Medicare Willing To Pay For Sleep Apnea Mouthpieces

Oral appliances are a fantastic treatment option for obstructive sleep apnea, but does Medicare Cover Oral Devices for Sleep Apnea?
Oral appliances for obstructive sleep apnea are covered under Medicare if they fulfill specific criteria and are determined to be Medicare-approved. To qualify for coverage:
- The patient must see a doctor prior to seeking coverage and a dentist must order the device.
- To establish a sleep apnea diagnosis, the patient must have a Medicare-approved sleep test.
- The dentist must be a Medicare DME Supplier in order to receive payment.
- All requirements of the durable medical equipment definition must be fulfilled by the oral device.
- For the treatment of obstructive sleep apnea, oral appliance therapy must be both necessary and appropriate.
- The patient is not able to tolerate a positive airway pressure device, or the doctor determines that using the CPAP machine would be ineffective in that situation.
- All other billing, coding, and documentation necessities must also be completed.
Its critical that all important criteria are fulfilled in order for Medicare to reimburse your oral device. In certain situations, coverage is given at a specific proportion, with the patient on the hook for the difference.
Also Check: Does Medicare Supplement Cover Medicare Deductible