What Does Prolia Do
Throughout your life, your body breaks down existing bone and builds new bone in its place to keep your skeleton strong. Osteoclasts are the cells that drive the process. As you age, the bone-building process slows down while the work of osteoclasts continues at the same pace. This leads to a loss of bone density. Prolia is an injectable medication that works by disrupting the activation of osteoclasts to slow down bone loss.
Medicare Prior Authorization Explained
Home / FAQs / General Medicare / Medicare Prior Authorization Explained
Before your doctor can provide specific services, prior authorization from Medicare may be necessary. Depending on your plan type, you might need prior approval to see a specialist.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
So, which services and types of plans require prior authorization? Below, well explain what you need to know.
Millions Of Americans Have Osteoporosis With Even More Suffering From Decreased Bone Density Leaving Them At Greater Risk Of Developing Osteoporosis In The Future
While osteoporosis is more prevalent in women and adults older than 65 compared to those aged 50-64, men and women of any age can also develop it.
Prolia is a prescription drug approved by the U.S. Food and Drug Administration used to treat osteoporosis in women after menopause who at higher risk for fracture. Because osteoporosis and decreased bone density increase your risk for fractures or other injuries due to a fall, Prolia works with your body to help stop the development of bone-removing cells, protecting your bones longer.
Read on to learn more about Medicares coverage for Prolia, as well as other information about osteoporosis and helpful benefits you may have.
Also Check: How To Sign Up For Medicare At Age 65 Online
Medicare Part C Inpatient Coverage
The inpatient coverage youll receive with Medicare Part C will at least match those of Medicare Part A. These services include:
- inpatient hospital care
- vaccinations for flu, hepatitis B, and pneumococcal disease
Any additional coverage for these services will be outlined by the specific plan you choose. For example, some plans offer basic vision exams, while others include allowances for prescription eyeglasses or contact lenses.
The cost of a Medicare Part C plan will depend on a variety of factors. The most common costs within your plan will be:
- your Part B monthly premium, which may be covered by your Part C plan
- your Medicare Part C costs, which include a deductible and monthly premiums
- your out-of-pocket costs, which include copayments and coinsurance
Below are some cost comparisons for Medicare Part C plans in some major cities around the United States. All the plans listed below cover prescription drugs, vision, dental, hearing, and fitness benefits. However, they all differ in cost.
How Much Does Prolia Cost With Medicare
If you qualify for coverage for Prolia under Medicare Part B, your plan will typically pay 80% of the injection while you pay the remaining 20%. Based on the list price of the drug, the 20% coinsurance would amount to roughly $250. You’ll usually need to satisfy your Medicare Part B deductible before your plan will cover the drug.
Under Medicare Part D, the amount you’ll have to pay out of pocket depends on the terms of your plan, what tier your plan classifies the drug as and what stage of coverage you’re in.
- Deductible stage. Until you satisfy your plan’s deductible, you will usually need to pay the full price for Prolia.
- Post-deductible stage. After you have met your deductible, your plan will typically pay for some or most of the cost of the drug, leaving you responsible for a copay.
- Donut hole. Once your total drug spending reaches the threshold for your plan’s coverage gap or donut hole, you’ll generally be responsible for 25% of the cost of Prolia.
- Post-donut hole. After you and your plan have spent more than the upper limit for the donut hole, you’ll enter catastrophic coverage, with your plan likely paying most of the cost of the drug while you are responsible for only a copay or coinsurance.
Don’t Miss: Is Xiidra Covered By Medicare Part D
Us Food And Drug Administration
- Treatment of postmenopausal women with osteoporosis at high risk for fracture
- Treatment to increase bone mass in men with osteoporosis at high risk for fracture
- Treatment of men and women with glucocorticoid-induced osteoporosis at high risk for fracture
- Treatment to increase bone mass in men at high risk for fracture receiving androgen deprivation therapy for non-metastatic prostate cancer
- Treatment to increase bone mass in women at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer
Giant Cell Tumor Of The Bone
Anderson et al reviewed investigational approaches and control paradigms for recurrent or metastatic primary bone tumors . These researchers analyzed temozolomide plus irinotecan data and reviewed in the context of other newer approaches including anti-angiogenesis, anti-IGF-1R antibodies and bisphosphonates for ES. Some current state-of-the-art approaches for OS include L-MTP-PE, anti-IGF-1R inhibition, aerosol therapies and bone specific agents. The authors stated that bone-specific agents including denosumab and bisphosphonates may have benefit against ES, OS, and giant-cell tumor .
Read Also: How Old Do You Need To Be Eligible For Medicare
Medicare Part B Drugs: Cost Implications For Beneficiaries In Traditional Medicare And Medicare Advantage
In the face of rising prescription drug costs, a large majority of the public supports federal efforts to lower drug spending. In his 2022 State of the Union address, President Biden urged Congress to pass legislation to rein in drug costs. In November 2021, the House of Representatives passed the Build Back Better Act , which includes several provisions that would lower prescription drug costs, but the Senate has yet to take action on this legislation. Proposals included in the BBBA would allow the federal government to negotiate the price of some drugs covered under Medicare Part B and Part D require drug companies to pay rebates to the federal government when annual increases in drug prices for Medicare and private insurance exceed the rate of inflation cap monthly insulin costs for people with Medicare and private insurance and cap Medicare beneficiaries out-of-pocket drug spending under Part D .
In the first part of this analysis, we examine Medicare claims data for 2019 to assess cost-sharing liability for Part B drugs for beneficiaries in traditional Medicare . In the second part of our analysis, we use Medicare Advantage benefit design data for 2022 to examine the range in cost-sharing amounts at or below 20% coinsurance charged by Medicare Advantage plans for in-network Part B drugs. We also analyze variation in cost-sharing amounts for out-of-network Part B drugs charged by plans that provide out-of-network coverage.
License For Use Of Dental Procedure Codes Fourth Edition
End User Point and Click Agreement
These materials contain Current Dental Terminology, is copyright by the American Dental Association. © 2012 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED âI ACCEPTâ, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED âI DO NOT ACCEPTâ AND EXIT FROM THIS COMPUTER SCREEN. IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, âYOUâ AND âYOURâ REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
Read Also: Does The Mayo Clinic Take Medicare
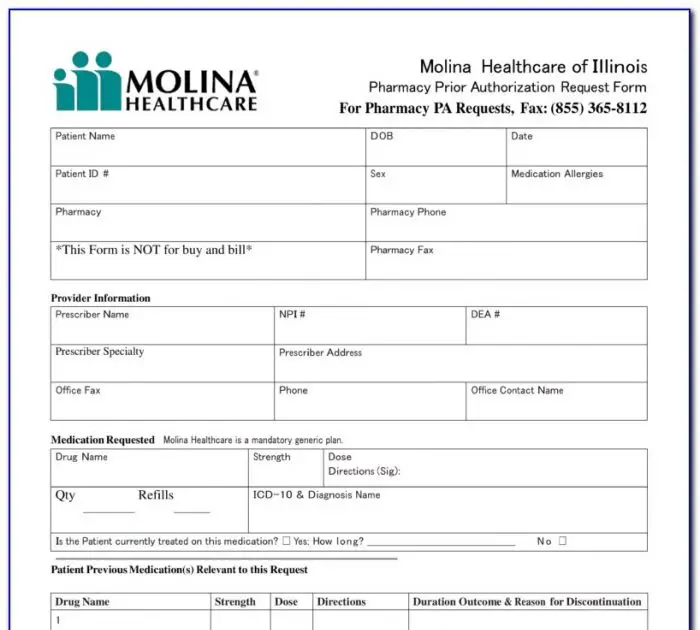
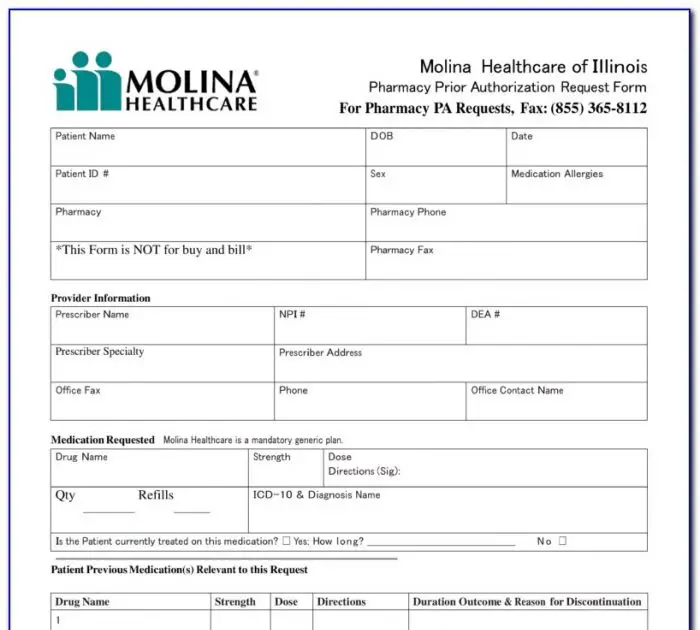
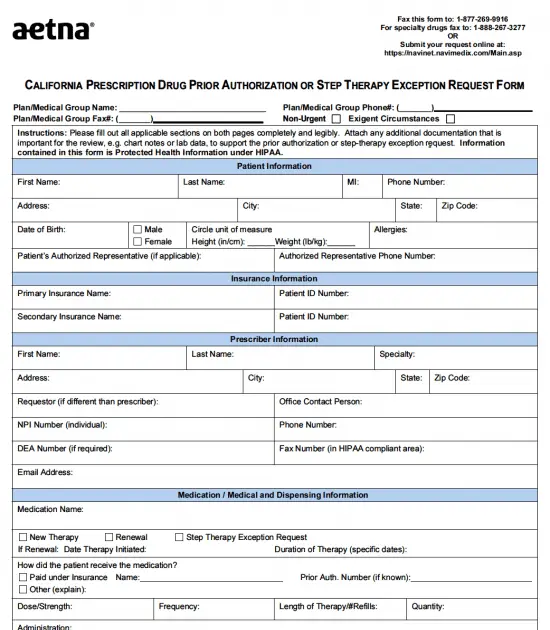
Medicare Part D Prior Authorization
Often, even top Part D prescription drug plans need prior authorization for coverage on specific drugs. Different policies have varying rules, so youll need to contact the carrier directly to confirm coverage.
Most Part D plans have forms you can download online. The online option is a useful way to print the documents and take them to your doctor. Your doctor can help you correctly complete the form.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
Also, recipients may directly contact their Part D plan and ask for a mail-in form. You can find the number for Member Services on your plans member ID card.
Compendial Uses For Xgeva
- Second line therapy for osteopenia or osteoporosis in patients with systemic mastocytosis
- Thyroid cancer as palliative care for bone metastases
Denosumab is available as Prolia and Xgeva . Denosumab is a fully human monoclonal antibody that inhibits osteoclastic bone resorption by binding to osteoblast-produced RANK ligand , a cytokine member of the tumor necrosis factor family. By reducing RANKL binding to the osteoclast receptor RANK, bone resorption and turnover decrease.
Denosumab is a novel, fully human, highly specific, monoclonal antibody to receptor activator of nuclear factor kappabeta ligand . The antibody is produced in genetically engineered mammalian cells. Use blocks osteoclast activation, thereby resulting in a decreased bone resorption . Three molecules, RANKL, receptor activator of nuclear factorkappabeta , and osteoprotegerin have been identified as essential factors in osteoclast generation and function the RANKLRANKosteoprotegerin pathway is responsible for osteoclast differentiation, activation, and survival. Denosumab, a monoclonal antibody to RANKL, mimics the actions of osteoprotegerin, and therefore, reduces bone resorption.
An increased risk of hypocalcemia has been observed in clinical trials of patients with increasing renal dysfunction, most commonly with severe dysfunction , and with inadequate/no calcium supplementation. Monitor calcium levels and calcium and vitamin D intake.
Don’t Miss: How To Get Free Medicare
American Hospital Association Disclaimer
The American Hospital Association has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
Lower Medicare Advantage Premiums
Medicare Advantage plans are administered by private insurers. Premiums vary, but the average rate is dropping to $18 a month. The premium for Medicare Advantage plans is in addition to the Part B premium, which everyone pays . Some insurers advertise zero-premium plans, but this refers to the additional Medicare Advantage premium these plans are allowed to charge. People who enroll in a zero-premium Medicare Advantage plan will still need to pay the Part B premium.
Read Also: What Do The Different Parts Of Medicare Cover
Read Also: How To Get A Wheelchair From Medicare
Is Prolia Covered By Medicare
- Is Prolia covered by Medicare?’ Learn about the cost of this osteoporosis drug and how much you can expect to pay for it if your doctor prescribes it for you.
The National Osteoporosis Foundation reports that roughly 10 million Americans have osteoporosis and that an additional 44 million people suffer from decreased bone density and may develop the disease in the future. Osteoporosis puts you at an increased risk for debilitating fractures, but there are treatments available to lower the likelihood of injury due to a fall or other accident.
Prolia is approved by the U.S. Food and Drug Administration to treat bone loss and minimize fracture risk. In many cases, Medicare covers Prolia to make treatment more affordable.
Puerto Rico Prior Authorization Requests
Prescribers should submit these requests to the Puerto Rico Medication Intake Team by fax at 1-800-594-5309 or 1-800-658-9457 .
Prescribers with questions about the prior authorization process for professionally administered drugs should call 1-866-488-5995 for Medicare requests and 1-800-314-3121 for commercial requests. Assistance is available Monday through Friday, 8:30 a.m. to 5:30 p.m. local time.
Read Also: What Is The Cost Of Medicare B
What Is Medicare Prior Authorization
There are many confusing terms that are used when discussing Medicare health insurance, among them is the term prior authorization. This term refers to the requirement which states that a healthcare provider must obtain approval from the Medicare program itself in order to provide a given medical service or treatment. In other words, it ensures that benefits cover treatment that is expressly pre-approved by Medicare.
Of course, this begs the question: Does Medicare require prior authorization? Well, like many things in the world of insurance, the answer is a bit more complicated than a simple yes or no. In actuality, whether prior authorization is specifically required for you, the Medicare beneficiary, to receive certain treatment is entirely dependent on the treatment or service itself and the level of Medicare coverage you have.
Lets take a look at this question in more detail by breaking down the specifics of prior authorization requirements by the different parts of Medicare.
Other Hcpcs Codes Related To The Cpb : :
J1740 Injection, ibandronate sodium , 1 mg J3489 Injection, zoledronic acid, 1 mg J9000 Injection, doxorubicin HCl, 10 mg J9022 Injection, doxorubicin HCl, liposomal, imported Lipodox, 10 mg Q2050 Injection, doxorubicin HCl, liposomal, not otherwise specified, 10 mg S0156 Tamoxifen citrate, oral, 10 mg
Recommended Reading: Does Medicare Cover Prrt Treatment
Is There A Generic Version Of Prolia
Denosumab is a generic alternative to Prolia. Denosumab also serves as the generic form of Xgeva, which is a drug identical to Prolia that is used to treat skeletal-related events in patients with multiple myeloma and bone metastases.
Denosumab costs may be slightly less than that of Prolia due to its generic nature.
What Part Of Medicare Pays For Prolia
For those who meet the criteria prescribed above, Medicare Part B covers Prolia. If you don’t meet the above criteria, your Medicare Part D plan may cover the drug. GoodRx reports that 98% of surveyed Medicare prescription plans cover Prolia. With Medicare Part D coverage, youâre likely to pay coinsurance or a copay.
Recommended Reading: Which Drugs Are Covered By Medicare Part D
Is Prolia Covered By Medicare 2019
by Sharon Groves | Mar 19, 2019 | The American Retirement Advisor Blog
There is an antibody in Prolia that slows down the weakening of bones. It signals the cells that break bone down, preventing these cells from forming. The FDA has approved twice-a-year Prolia injections to treat osteoporosis in people with a high risk of fractures. It is usually administered to the patient in a doctors office.
Possible side effects include serious allergic reactions, low blood calcium, severe jaw bone problems, unusual thigh bone fractures, and increased risk of broken bones. After stopping Prolia, serious infections, skin problems, and bone, joint, or muscle pain, can occur.
Foods that increase bone density are milk, cheese, dairy foods, green leafy vegetables, broccoli .
Prolia is administered in your doctors office or a medical clinic. The drug could be considered a covered item under Medicare Part B if Medicare determines the drug is medically necessary. Pre-authorization is required before Medicare will pay for your treatment.
Medicare Part A and Medicare Part B help pay for an injectable drug for osteoporosis and visits by a home health nurse to inject the drug, if you meet these conditions:
1)Youre a woman.
2) Youre eligible for Part B and meet the criteria for Medicare home health services.
See Medicare.gov.
Dont Miss: How Much Is Medicare And Medicaid
End User Point And Click Agreement
CPT codes, descriptions and other data only are copyright 2012 American Medical Association . All Rights Reserved. Applicable FARS/DFARS Clauses Apply.
You, your employees, and agents are authorized to use CPT only as contained in the following authorized materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services . You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, 515 N. State Street, Chicago, IL 60610. Applications are available at the AMA Web site, .
Applicable FARS/DFARS restrictions apply to government use.
U.S. Government Rights
Don’t Miss: Do Medicare Advantage Plans Cover Home Health Care
Is The Cost Of Prolia Covered By Medicare
Whether Prolia is covered by Medicare depends on the type of Medicare coverage you have. Many different Medicare plans are available. And Prolia may be covered under some Medicare plans but not others.
If you have a Medicare plan, contact your doctor or your Medicare plan provider. Either can let you know what youll pay for Prolia.
You May Like: Does Medicare Pay For Portable Oxygen Tanks
Compendial Uses For Prolia
- Prevention or treatment of osteoporosis during androgen deprivation therapy for prostate cancer in patients with high fracture risk
- Consider in postmenopausal patients receiving adjuvant aromatase inhibition therapy along with calcium and vitamin D supplementation to maintain or improve bone mineral density and reduce risk of fractures
Recommended Reading: How Do I Register For Medicare Part A
Recommended Reading: What Month Does Medicare Coverage Begin