How Much Does Medicare Pay For An Emergency Air Ambulance Transportation
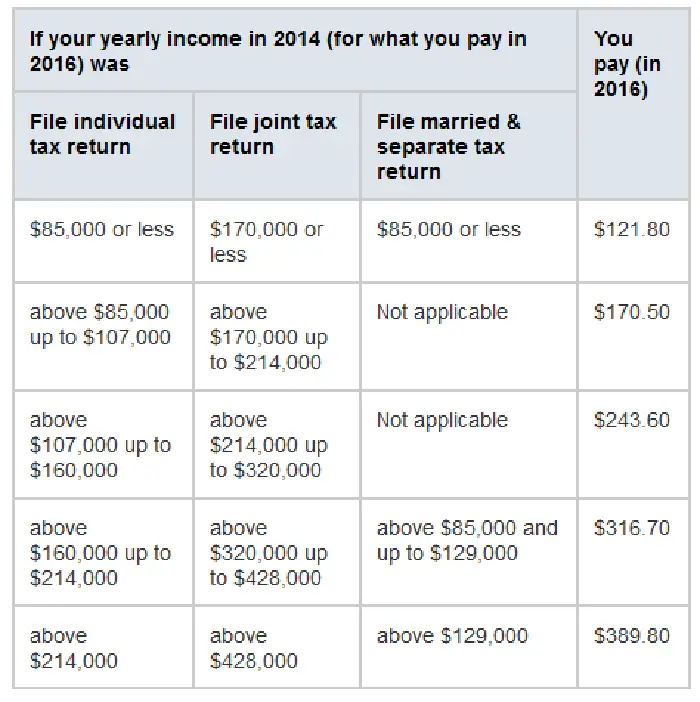
Depending on the terms and conditions of your Medicare Advantage plan, the rules and options available to you will differ. If you have Original Medicare, Medicare Part B will typically cover 80% of the cost of your air ambulance ride. After you have met your Part B deductible, which in 2022 is $233 per year, you will typically pay the 20% co-payment.
What Are The Out
Medicare Part B pays 80 percent of the cost of a wheelchair after you have met your annual deductible. You will pay 20 percent of the cost in addition to your annual Medicare premiums. You may also have copay costs associated with any doctor visits necessary to get your wheelchair.
In some parts of the country, DME suppliers are required to participate in a competitive bidding program, which helps to keep costs manageable. However, that competitive bidding program has been temporarily paused until January 1, 2021.
During this temporary gap, it is especially important to be aware of aggressive marketing techniques practiced by some DME suppliers. If you have any questions or concerns about a DME supplier, or about someone who has come to your home to try to sell you DME, you can call the Fraud Hotline of the HHS Office of Inspector General at 1-800-HHS-TIPS or report it online.
Read Also: When Is Medicare Supplement Open Enrollment
Original Medicare And Emergency Ambulance Transportation
Medicare covers emergency ambulance transportation if youve had a sudden medical emergency and your health is in danger.
Medicare may pay for emergency ambulance transportation by helicopter or airplane if your condition requires rapid transportation that cannot be provided on the ground.
Coverage for emergency ambulance transportation depends on the seriousness of your condition.
In some cases, Medicare may cover transportation in an ambulance if you have End-Stage Renal Disease and need ambulance transportation to and from the facility where you receive dialysis treatment.
Also Check: What Is The F Plan For Medicare
What Qualifies As An Ambulance
An ambulance is a medically equipped vehicle which transports patients to treatment facilities, such as hospitals. They can rapidly transport paramedics and other first responders to the scene, carry equipment for administering emergency care and transport patients to hospital or other definitive care.
Does Medicare Cover International Air Ambulance Services
Medicare does not typically cover care received outside of the United States, including air ambulance services. It will cover international medical care in only a few scenarios. These include emergencies near the U.S. border, where the nearest hospital is in another country. This can also include medical emergencies on cruise ships or while traveling between the continental United States and Alaska.
Advice: If you intend to travel outside the United States, you should consider purchasing travel insurance.
Recommended Reading: How Do Medicare Insurance Brokers Get Paid
Original Medicare Transportation Example
If Original Medicare is your sole coverage, your total out-of-pocket costs will include your monthly monthly Medicare Part B premium, your calendar year deductible and 20% coinsurance for approved services.
When calculating a claim payment, Medicare uses the Medicare approved amount what Medicare will pay a doctor or supplier that accepts assignment which may be less than the actual amount a provider charges. Assignment means a provider agrees to accept the Medicare-approved amount as payment in full. Most providers accept assignment, but its a good idea to check to be sure. If the provider does not accept assignment, you may be billed for the difference.
Below we have provided an example of how Original Medicare would pay for an ambulance bill:
| Cost type |
|---|
| The remaining 20%, or $200 |
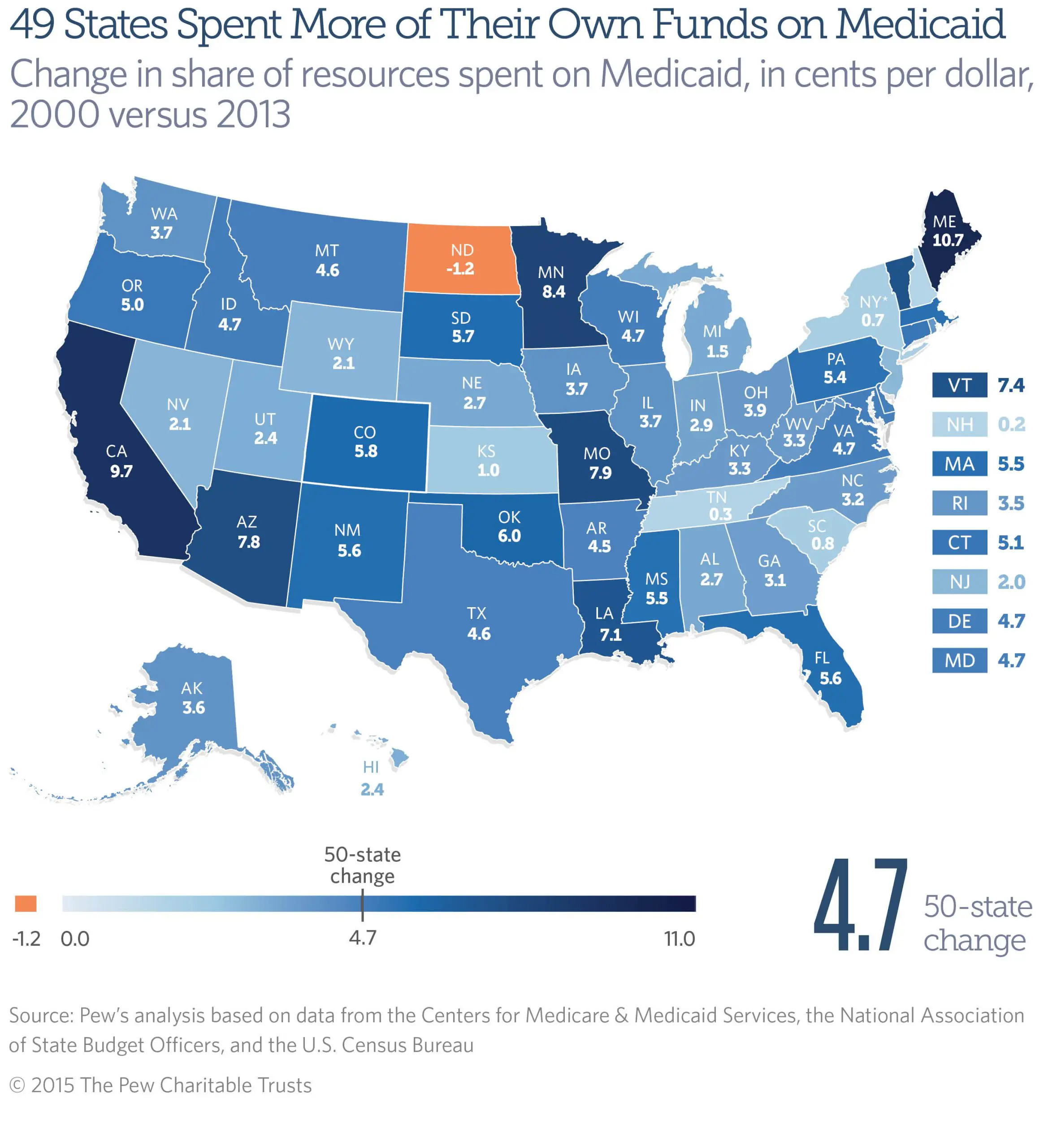
State And Local Programs
Your state or city may have additional programs that can help you find transportation. The programs and the types of services they provide may differ from one area to another.
One option is to look for Area Agencies on Aging near you. AAA helps address the needs of people who are ages 60 and over, with a large focus on access to transportation.
To find state or local programs, including AAA, use the Eldercare Locator. This is a tool developed by the U.S. Administration on Aging that can help you find many different services in your area.
Don’t Miss: How To Appeal Medicare Part B Late Enrollment Penalty
When Will Medicare Cover Air Transportation
An alternative to ambulance transportation is transport by air. Medicare medical transportation in a helicopter or airplane may be covered if a patients health condition requires such travel. Travel by air must be deemed faster than an ambulance to be considered for coverage.
Additionally, Medicare-covered air transportation demands that any delay in treatment could result in loss of life or serious complications. Example scenarios that may qualify a patient for air travel rather than a traditional ambulance include:
- A pickup location difficult to reach by ground transportation
- Long distances to nearest facility
- Heavy traffic that could prolong sensitive transportation times
When Does Medicare Cover Emergency Medical Transport Services
Medicare covers medically necessary medical transportation to the closest hospital in the event of an emergency. Medicare Part B generally pays all but 20% of the Medicare-approved amount for most doctor services plus any Part B deductible. Ambulance companies must accept the Medicare-approved amount as payment in full. This also applies to emergency air medical transport services. If Medicare determines your condition did not warrant emergency medical transportation, it may not cover any of the costs.
In some very limited cases, Medicare will also cover non-emergency medical transport services by ambulance, but you must have a written order from your health-care provider stating that your medical condition requires transportation by ambulance.
Keep in mind that Medicare is testing a new program in a few states for beneficiaries who need scheduled, non-emergency medical transportation three or more times in a short period. In these states, the ambulance company is required to get prior authorization before a fourth ride is arranged if Medicare denies authorization, and you still use the ambulance, the company may bill you in full for all charges. States and districts currently affected by the program include:
New To Medicare?
Becoming eligible for Medicare can be daunting. But don’t worry, we’re here to help you understand Medicare in 15 minutes or less.
Don’t Miss: Does Medicare Pay For Calquence
What Is Emergency Medical Transportation
You need emergency medical transportation if youve had a sudden health crisis or accident and your health is in serious danger, so much so that it may be harmful for you to ride in a car or taxi. Here are some situations in which emergency medical transportation is necessary:
- You are unconscious, in shock, or bleeding uncontrollably from an accident or injury.
- Your condition requires skilled medical care while you are en route to the hospital.
Emergency medical transportation also applies to emergency air transport if you are in a location that cant be reached by a ground ambulance, or if traffic conditions are such that waiting for ground transportation could have life-threatening consequences.
What Happens If Medicare Doesnt Pay For An Ambulance
Youll receive a Medicare Summary Notice for the Medicare ambulance billing denial. Review that document carefully. While it might demonstrate that the trip wasnt covered, it may also demonstrate that the ambulance company failed to fully document the reasons for your transportation or that the proper paperwork wasnt filed. If either of those is the case, youll want to speak to the ambulance company or your provider.
Medicare may also determine that there wasnt a Medicare-defined medical necessity for ambulance transport. Namely, 1) that some other method of transport could have worked or 2) you didnt need as many ambulance trips as ordered.
If Medicare doesnt cover your ambulance ride, you have the ability to appeal the decision. The MSN will have instructions for how to file an appeal. Follow those to the letter. Also, speak with your provider and the ambulance company to gather supporting documentation for your appeal.
Also Check: Does Medicare Pay For Entyvio
Medical Transportation With Medicare Advantage
Medicare Advantage covers the same benefits as original Medicare, but through private insurance companies. These plans must offer at least the same coverage as original Medicare.
This means that a person would receive the same emergency and nonemergency transportation under Medicare Advantage as they would under original Medicare.
However, Medicare Advantage companies may require a person to choose in-network ambulance services to receive full reimbursement.
How Many Wheelchairs Will Medicare Pay For
If you have a wheelchair, your life will be drastically changed.
However, youll have to consider the cost of wheelchairs.
Many new wheelchair users worry about this: what wheelchairs does Medicare cover? We are here now to help you answer this question.
In order to qualify for wheelchair coverage, you must not have mobility issues that negatively impact your daily activities when you are away from home.
Find out if you are eligible for medical insurance, and if so, which of the plan options is right for you. Lets get into it.
Read Also: Are Doctors Required To Accept Medicare
Read Also: What Is Medicare Open Enrollment
Whats The Medicare Beneficiaries Cost Associated With Transportation
So, does Medicare offer transportation? Well, now you know that Medicare has a set amount they will approve for patient transport. Transportation services that are part of Medicares network are required to accept Medicares agreed amount.
Patients with Medicare Part B will be responsible for 20% of the Medicare-approved charge. Meanwhile, Medicare pays the other 80%.
If the ambulance company accepts assignment from Medicare, then it must instead accept an agreed-upon payment when transporting Medicare beneficiaries. Often, the Medicare-approved amount paid to the provider is less than the amount normally charged.
For example, if ambulance transportation took place due to a serious medical emergency, an ambulance company might normally charge $800. Hypothetically, lets say the Medicare-approved amount is $400. Instead of paying 20% of $800, a Medicare beneficiary pays 20% of only the $400 Medicare-approved fee, amounting to $80.
The difference in charges is because patients are only responsible for 20% of the Medicare-approved amount.
However, a few situations demand different charges for transportation:
The balance remaining after Medicare paid is eligible for secondary insurance, which may come in the form of a Medicare Advantage Plan or a Medigap supplemental plan.
Enter your zip below to find affordable rates for your transportation needs with our free plan comparison tool.
How Much Does Medicare Cover
If Medicare approves your ambulance transport claim, it covers 80% of the Medicare-approved amount, leaving you responsible for the other 20%. The Medicare-approved amount is a fee schedule that varies based on your location.
However, ambulance transport counts toward your annual Part B deductible. So, if you havent yet met your deductible, youre responsible for paying the remaining amount plus the standard 20% coinsurance.
Don’t Miss: How Do I Choose Medicare Part D Plan
How Much Does Dialysis Cost
Health insurance policies are covering the costs of dialysis treatment. So, if you have health insurance, you will have to pay only for coinsurance and deductibles. For instance, a patient with Medicover health insurance would have to pay $160 for deductibles and 20% of the total amount for coinsurance. Though, there are Medicare patients with secondary health insurance that covers the whole cost or part of it. According to a Health Affairs article, the monthly costs for an average U.S. patient are $120 for the dialysis-related drugs and around $12 for dialysis.
If you dont have health insurance, expect to pay more than $550 for a single hemodialysis treatment and more than $73,000 per year for the typical three treatments per week. Depending on the medical prescription, vitamins and injectable drugs can add hundreds of dollars to the final price. For example, patients going to one of the many DaVita dialysis centers from the U.S. would have to pay around $500 for the dialysis treatment, without medications. On the other hand, a dialysis center from Ohio charges more than $1,450 but is open to negotiations with self-pay patients.
You might also like our articles about the cost of a kidney, pelvic ultrasound, or wound VAC.
In case of an emergency, the cost for un unscheduled dialysis treatment at a hospital would be much higher. For instance, the price of a single treatment at the Baptist Memorial Health Care from Memphis is around $10,000.
How Can I Get Free Transportation
Local organizations may have volunteer driver programs.
Also Check: Is Mutual Of Omaha A Good Medicare Supplement Company
Your Costs For Ambulance Services
Regardless of whether your ambulance trip is considered emergency or non-emergency, youre responsible for a portion of its cost, unless you have supplemental coverage that will pay your share. Your Part B deductible will apply , and then Medicare will cover 80% of its approved amount for the ambulance transportation. Youll be responsible for the other 20% of the cost.
Does Medicare Cover Air Ambulances
Depending on your case and coverage plan, Medicare might cover your air ambulance trip. However, there are certain conditions that must be met.
As a general rule, Medicare strongly favours land ambulances, this services costs being substantially lower. However, in some cases, Medicare Part B as well as Medicare Advantage will pay for air ambulance transportation by airplane or helicopter.
For this purpose, the service must be medically necessary, which means that you require immediate and rapid ambulance transportation that a ground ambulance cannot provide. An example of medical necessity might be if you need a specialized, complex, and time-critical surgery.
If your current hospital lacks the necessary equipment or surgical staff, Medicare would most likely cover the air ambulance fees to transport you to a hospital that could perform the surgery. On the other hand, in most cases where there is no imminent danger of death, Medicare will most likely deny coverage for an air ambulance.
More specifically, for Medicare to cover your air ambulance, the medical flight must be required for one of the following reasons:
- A ground ambulance cannot reach your pick-up location or
- There is a significant distance to travel by ground or obstacles, like heavy traffic, could prevent you from reaching the nearest health care facility.
Be cautious: Medical necessity can look very different to a doctor than it does to Medicare.
Don’t Miss: Is Medicare Part D Worth It
Is Transportation To My Doctor Included In My Medicare Plan
Contributing expert: Kelly Blackwell, Certified Senior Advisor®Updated: March 30, 2022Understand your Medicare coverage for emergent and non-emergent transportation and learn about transportation resources in your community.
Kelly Blackwell
Kelly Blackwell is a Certified Senior Advisor ®. She has been a healthcare professional for over 30 years, with experience working as a bedside nurse and as a Clinical Manager. She has a passion for educating, assisting and advising seniors throughout the healthcare process.
You may need transportation to and from a hospital or other care facility, including your doctors office. Original Medicare only covers ambulance transportation deemed medically necessary and when your medical condition is such that traveling any other way would endanger your health.
Medicare Advantage Plans also cover medically necessary ambulance transportation as a Medicare-covered service. MA plans may help pay for transportation that Medicare does not cover.
According to the Kaiser Family Foundation , in 2022, 38% of the Medicare Advantage plans available across the country include transportation as an additional benefit. Chances are high that you will have access to at least one of these plans in your area.
Most areas of the country have resources and federal or state programs to help you find options for non-emergency medical transportation. Depending on your income and health condition, you may qualify for financial assistance.
Some Medicare Advantage Plans Also Cover Non
Some Medicare Advantage plans may cover non-emergency medical transportation to doctors office appointments, physical therapy sessions and even the pharmacy. Some plans may partner with ride-sharing companies such as Lyft to provide this covered benefit.
43% of Medicare Advantage plans cover transportation as an additional benefit in 2023.1
This benefit came as a result of a 2018 ruling by the Centers for Medicare & Medicaid Services to allow Medicare Advantage plans to begin including non-emergency medical transportation as a covered benefit.
Private Medicare Advantage plans are required by law to include all of the same benefits covered by Medicare Part A and Part B , which are provided by the federal government. This means Medicare Advantage plan beneficiaries also have the same emergency transportation coverage detailed above by Original Medicare, in addition to any additional non-emergency transportation that their plan covers that isnt covered by Original Medicare.
Don’t Miss: What Age Do You File For Medicare
What About Medicare Advantage Plans With Transportation Coverage
If you are familiar with your Medicare options, you may have heard that the dream of getting your medical transportation covered by Medicare may be a reality under certain Medicare Advantage plans. Believe it or not, it may be possible to get transportation services insurance through certain Medicare Advantage plans, including non-emergency Medicare appointment transportation.
Keep in mind, however, that Medicare Advantage plans are offered by private insurance providers. This means that exact pricing, availability, and benefits will vary from plan to plan. Remember that Medicare Advantage plans with transportation coverage may not be available everywhere.
Does Medicare Pay For Transport From Rehab To Home
If a patient meets specific conditions, non-emergency ambulance transportation may be paid under Part B Medicare. These criteria include: After being discharged from the hospital, patients are transported to their homes. Patients live in a nursing home on a full-time basis who require transportation to non-emergency doctor appointments.
You May Like: What Are The Qualifications To Get Medicare
