What Are The Medicare Annual Limits For Mental Health Provider Services
The law limits Medicare payments for outpatient mental health to 62.5% of expenses in the calendar year. Services include the treatment of mental, psychoneurotic, and personality disorders for people not inpatient in a hospital. These limitations DO NOT apply to diagnosis, but rather, they apply to treatment.
Which Mental Health Services Does Medicare Cover
Medicare covers a wide variety of mental health treatments. This includes psychotherapy and counseling services provided by a clinical psychologist or psychiatrist, clinical social worker, nurse practitioner, clinical nurse specialist, or physician assistant. Group psychotherapy and family counseling are often covered in most cases as well.
Medicare also covers a variety of diagnostic tests and psychiatric evaluations. This includes an annual depression screening, alcohol misuse screening, and testing for other mental health conditions. These tests may be performed by a psychologist or your normal physician — they should be covered either way.
What Youll Pay For Outpatient Mental Health Care
For outpatient mental health care, after you meet the Medicare Part B deductible, which is $233 in 2022 , Part B covers 80% and you’re responsible for 20% of covered services. Its important to note that the mental health professionals you use must accept Medicare assignment that means they agree to Medicares price schedule and will not charge you more.
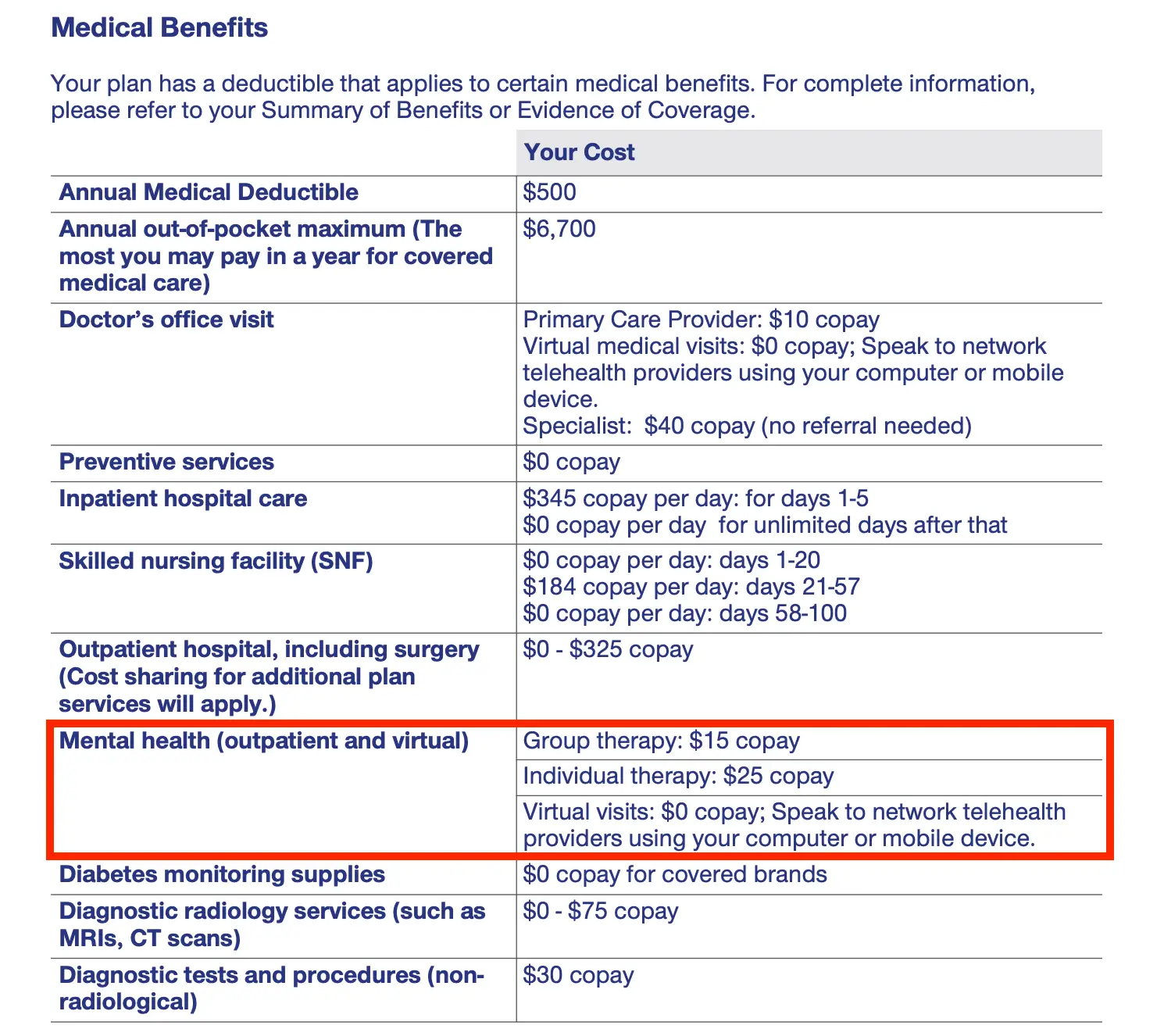
If you have Medicare Supplement Insurance, or Medigap, your 20% share may be covered by your plan. If you have a Medicare Advantage plan, youll need to check your specific plan to see how much youll pay.
If you receive additional mental health services in hospital outpatient facilities, you may owe additional fees to the hospital.
To get information on your out-of-pocket costs, talk to your health care provider. Your bottom line will depend upon providers charges, the facility type, whether your doctor accepts Medicare assignment and any other insurance you may have.
You May Like: Which Type Of Care Is Not Covered By Medicare
Does Medicare Cover Counseling If You Have Medicare Advantage
Medicare Advantage is private insurance, which means that your coverage may be different depending on the specific plan you choose. At a minimum, Medicare Advantage must provide the same level of counseling and therapy coverage as Original Medicare.
Your Medicare Advantage plan may charge a flat copayment for counseling and therapy services instead of a percentage-based coinsurance. You may also need to get counseling from providers in the plans approved network of providers.
Also noteworthy, some Medicare Advantage plans require referrals and prior authorization for therapy and counseling services.
If you have a Medicare Advantage plan, check your plan brochure for specific information about mental health coverage. You can also call your plans Member Services department for further help.
What If My Mental Health Medication Is Not On My Plan Formulary
Medicare covers all therapeutic classes of prescriptions, which doesnt mean there is coverage for all prescription drugs. If youre on an uncovered medication, you have a few options.
- Ask your provider to prescribe another medication that can help provide the same results
- Ask for a Formulary Exception
Also Check: Are Hearing Aid Batteries Covered By Medicare
Faqs On Mental Health And Substance Use Disorder Coverage In Medicare
The COVID-19 pandemic has taken a heavy physical and mental health toll on all ages, including older adults, heightening interest in strategies to improve access to mental health and substance use disorder services generally, and in Medicare. In April 2022 more than two years into the pandemic one in six adults 65 and older reported anxiety and depression, according to KFF analysis of the Household Pulse Survey, somewhat lower than the quarter of older adults who reported anxiety and depression in August 2020, when the country was in still the midst of widespread lockdowns in the early stage of the pandemic. Additionally, nearly a third of adults 65 and older say that worry or stress related to coronavirus has had a negative impact on their mental health, according to KFF polling,a somewhat lower rate than reported among younger adults.
These FAQs review mental health and substance use disorder coverage and out-of-pocket costs in Medicare and discuss policy proposals related to coverage of mental health and substance use disorder treatments.
Get Your Billing Handled
It’s our goal to ensure you simply don’t have to spend unncessary time on your billing.
You want to get paid quickly, in full, and not have to do more than spend 10 or 15 minutes to input your weekly calendar.
You want to know you can call your billing admin, a real person you’ve already spoken with, and get immediate answers about your claims.
You want to not have to deal with it!
Learn how to offload your mental health insurance billing to professionals, so you can do what you do best.
As private practitioners, our clinical work alone is full-time. Add in the unnecessarily difficult insurance billing system and we run the risk of working way over full-time. TheraThink provides an affordable and incredibly easy solution. My daily insurance billing time now is less than five minutes for a full day of appointments. My cost is a percentage of what is insurance-approved and its my favorite bill to pay each month! Denny and his team are responsive, incredibly easy to work with, and know their stuff. I cannot capture in words the value to me of TheraThink. Thank you. You free me to focus on the work I love!
Recommended Reading: How Much Is Medicare Going Up
Reviews For Our Therapists
| Gabrielle Hollis |
“I love how Gabrielle makes me feel comfortable and seen. Her voice is extremely soothing. She is kind and works according to your needs. I am really grateful for her time and counselling. I feel more confident and validated. “
| Ann Iroz |
“Ann is a wonderful and insightful counselor, she had a way of working with me and my spouse that was effective in de-escalating a very difficult and emotional situation, and bringing the two of us back to a healthy place. “
| Glenny Trejos |
“She listens and also speaks. She gives good ideas when I feel like there is no other option to resolve things. She never makes me feel judged, even when I am the person in the wrong about things. She truly cares about my mental well being.”
| Carol HounslowCounsellor |
“I started therapy back in September and I’m so grateful that I was matched with Carol. She’s the most wonderful listener, I always feel heard and understood without ever being judged.Carol has really helped me see what the root causes are and has given me the confidence to implement changes in my daily life and how I approach my own thoughts. Through this process I’ve also discovered meditation and mindfulness, which has been game changing for my overall happiness and wellbeing particularly when coupled with our weekly sessions.I cannot thank you enough Carol – To anyone reading, if you’re ever paired with this therapist you are in very safe hands! “
| Zachari GeorgeLCSW |
“Zach is professional, caring and a terrific therapist! “
Why Is Medicare Hard To Bill For Mental Health Providers
Medicare subcontracts out to many different subcontractors like Noridian or Palmetto or Novitas or NGS or WPS or FCSO.
Each contractor has their own electronic claims submission enrollment requirements, forms, and process. Each system is clunky and the enrollments take quite some time. Most clients also have a secondary insurance company to bill alongside their Medicare coverage.
We take care of this enrollment process and secondary claims submission and follow-up for our providers at TheraThink.
Dont Miss: What Is The Best Medicare Supplement Insurance Plan
Also Check: Why Is My First Medicare Bill So High
Lindsay Malzone Medicare Expert
Medicare beneficiaries might be aware that they have some sort of mental health coverage, but may not understand what it entails regarding services, co-payments, and prescriptions
When it comes to mental health benefits, Kayrish says keep the following in mind:
- Original Medicare includes a 20% co-insurance and if you have a supplement, it will most likely cover it.
- Medicare Advantage includes the same type of coverage and a co-payment.
- Medicare Advantage may require a gatekeeper system, which means your primary carephysician has to refer you to mental health care.
Medicare Part D Prescription Drug Coverage And Mental Health Care
Medicare Part D prescription drug plans are not required to cover all drugs, but with limited exceptions, they are required to cover all antidepressant, anticonvulsant and antipsychotic medicines.
Part D plans are sold by private insurers and other companies that Medicare approves. Almost all plans have a formulary a list of drugs the plan covers. This list can change each year, but the company has to notify you at least 30 days before the change takes effect.
Its important to review your plans formulary changes when you receive this information.
Recommended Reading: How To Get Medicare And Medicaid Together
Where Can I Find Medicare Mental Health Providers
With traditional Medicare, you can see any eligible mental health provider who participates in the program and who accepts assignment, when required. But finding a psychiatrist who accepts Medicare patients can be a challenge. A recent Kaiser Family Foundation analysis found that 60 percent of psychiatrists are accepting new Medicare patients, compared with almost 90 percent of physicians who arent pediatricians, while other psychiatrists and mental health professionals refuse patients paying with Medicare or private insurance.
If you go to a provider who has opted out of Medicare, youll be responsible for the total bill Medicare wont reimburse you. A doctor who has opted out should ask you to sign a contract noting this, but its wise to ask mental health providers if they accept Medicare before youre treated.
To find a psychiatrist or other physician in your area who accepts Medicare, go to Medicares physician compare website. It helps that Medicare relaxed some of its restrictions on using telehealth services during COVID, which has improved access to mental health providers.
Why Is Medicaid Hard To Bill For Mental Health Providers
For the same reason that Medicare is hard to bill, except that each state has their own contract instead of each region . As such, your states Medicaid policy is up to them.
Each state may have their own system that they have built that might be slow and require many enrollments as well, or they might contract out the insurance coverage to existing commercial insurance companies.
Example: What you think is UHC is actually Medicaid via UHC and while youre in-network with UHC, youre out of network with their Medicaid network your claims get denied.
Make sure you understand exactly which Medicaid panels you are enrolling with, including if youre in-network with their commercial or Medicaid or HMO or PPO or EPO plans.
You May Like: How Do You Qualify For Medicare Part A And B
Read Also: How Old To Be Eligible For Medicare
Does Medicare Cover Mental Health Therapy
Yes, Medicare covers mental health care, which includes counseling or therapy. Depending on your needs, mental health care can be provided in a variety of settings. The goal is to get the right kind of support when you need it.
Mental health pertains to our emotional, psychological, and social well-being. Our mental health can impact how we think, feel, and act. From a holistic, whole-person perspective, mental health plays a big part in our general overall health. Just as Medicare helps cover physical ailments, it also offers various benefits to support emotional, psychological, and social health.
Mental health concerns include anxiety and depression, substance abuse, eating and stress disorders, schizophrenia, and attention-deficit/hyperactivity disorders. These concerns can range from mild to severe and can be addressed on an outpatient or inpatient basis.
You can access mental health benefits through Original Medicare or Medicare Advantage plans, an alternative to Original Medicare. MA plans offer the same services, follow the same Medicare rules as Original Medicare, and generally require in-network providers, referrals, and prior authorization to receive benefits.
Compare Medicare Advantage Plans That Cover Counseling
For California residents, CA-Do Not Sell My Personal Info, .
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
You May Like: Does Medicare Cover Assisted Living In Illinois
Who Is Eligible For Medicare
People who work pay into Medicare during their working years through a payroll tax, then are eligible to enroll when they turn 65 years old. Youre eligible for premium-free Medicare Part A if you worked and paid into Medicare for at least ten years.
Its possible to get Medicare Part A at age 65 even if you havent worked, but youll probably have to pay out of pocket to cover your premium. The exception is if you are married to someone who paid into Medicare for ten years or more. In that case, you should still be able to get Part A without paying a premium.
How Long Have We Had Medicare?
Medicare was passed in 1965 to increase access to healthcare for Americas senior citizens. Most people in America enroll in Medicare when it becomes available to them at retirement age. Before Medicare was passed, 54 percent of elders aged 65 and over had health insurance. Now, 98.4 percent of elders in America have health insurance through Medicare.
Medicare also covers people who are younger than 65 when they have disabilities. People with end-stage renal disease or Lou Gehrigs disease can enroll in Medicare before they turn 65 years old.
People who qualify for Social Security Disability Income for any reason are eligible for Medicare 24 months after they start receiving SSDI.
You can inquire about your Medicare eligibility at your local Social Security office.
Need Help Getting Coverage For Mental Health
Your mental health is just as important as your physical health, so ensure you have the coverage to face anything. Our licensed insurance agents can help you find Medicare Supplement coverage to patch the holes in your regular Medicare plan.
Our agents are extremely knowledgeable, friendly, and patient to guide you to the health insurance plan that best suits your needs. Best of all, their time is free for you.
So give us a call today. Or fill out our quick and easy online rate form to be connected with the best rates in your area.
Don’t Miss: What Is The Best Medicare Advantage Plan In Texas
Coverage Doesnt Guarantee Access
While Medicare covers mental health care, finding providers who accept Medicare as a form of payment for these services may be a struggle. Theres been an ongoing issue that folks cant seem to get a professional who accepts Medicare as payment for the mental health counseling and services they do deliver, says Kayrish.
How Much Do Medicare Beneficiaries Pay For Mental Health Benefits And Substance Use Disorder Benefits
Inpatient Services
Beneficiaries who are admitted to a hospital for inpatient mental health treatment would be subject to the Medicare Part A deductible of $1,556 per benefit period in 2022. Part A also requires daily copayments for extended inpatient hospital stays. For extended hospital stays, beneficiaries would pay a $389 copayment per day and $778 per day for lifetime reserve days. For inpatient stays in a psychiatric hospital, Medicare coverage is limited to up to 190 days of hospital services in a lifetime. Most beneficiaries in traditional Medicare have supplemental insurance that may pay some or all of the cost sharing for covered Part A and B services.
Outpatient Services
For most outpatient services covered under Part B, there is a $233 deductible and 20 percent coinsurance that applies to most services, including physician visits. However, some specific Part B services have different cost-sharing amounts :
Prescription Drugs
Those with Part D coverage face cost-sharing amounts for covered drugs and may pay an annual deductible and a monthly premium. For example, most Part D enrollees pay less than $10 for generic drugs, but many pay $40-$100 for brand-name drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing.
Recommended Reading: What Is Medicare Catastrophic Coverage
Does Medicare Cover Outpatient Mental Health
Medicare Part B covers mental health services you receive when youre not a hospital inpatient, such as in a doctors or therapists office, hospital outpatient department or community health center. Medicare generally covers mental health services and visits with psychiatrists, other doctors, clinical psychologists, clinical nurse specialists, clinical social workers, nurse practitioners and physician assistants.
Health care providers who aren’t medical doctors must consent to the amount Medicare approves as payment in full, called accepting assignment. But not all mental health professionals accept Medicare.
What you pay for outpatient mental health services. Once youve met the standard Part B deductible, $233 in 2022, youll pay 20 percent of the Medicare-approved amount for the services.
You can receive one depression screening each year thats not subject to the deductible or coinsurance if you go to a primary care provider physician, physician assistant or nurse practitioner who accepts the Medicare-approved amount. This provider must either treat you or refer you elsewhere for treatment, but those services are not free.
Coverage for partial hospitalization. Medicare will cover partial hospitalization if you need more intense treatment than you can get in a doctors or therapists office. Oftentimes, this treatment is provided in a hospital outpatient department or mental health center where you dont stay overnight.