Q: What If I Need A Drug My Medicare Part D Plan Doesnt Cover
A: According to medicare.gov, if you have a Medicare drug plan, you can ask for a coverage exception.
Basically, this means you can ask your plan to provide or pay for a drug you think should be covered.
You also can appeal your plan’s decision about whether or not to provide or pay for a drug.
Before you take either of these steps, though, talk with your doctor or the health care provider who wrote the prescription. He or she should be able to tell you if your plan has special coverage rules. They also can tell you if any generic or over-the-counter drugs could work as well as the ones they prescribed.
If that doesn’t help, go to cms.gov for more on how to request a coverage determination or exception.
How Much Does Medicare Pay For A Therapy Session
Remember, Medicare covers as much of the cost as is approved by Medicare. If it is not determined that your outpatient therapy service is medically necessary for you at Original Medicare, your provider will need to confirm that you will receive payment for 80% of the service in order to apply for reimbursement.
Medicare Reimbursement Rates For Psychotherapy
Please see our updated Medicare Rates:
| CPT Code |
|---|
| $42.17 | $25.30 |
The reduced rate here isnt the exact amount Medicare pays out but represents a rough estimate of the suggested reduction to expect from Medicare. In our experience, Medicare over-estimates the contracted rate for most private insurance companies so their total reduction, while large, still leaves providers with a modest but much higher earning than Medicaid.
Part of the reason why is Medicare is more selective with their network.
Also Check: Does Medicare Pay For A Registered Dietitian
Does Medicare Cover Therapy For Depression
Medicare Part B helps pay for one depression screening per year, and it must be done in a primary care doctors office or primary care clinic that can give follow-up treatment and referrals. In addition, Medicare beneficiaries are eligible to receive a one-time Welcome to Medicare preventive visit that includes a review of potential risk factors for depression.
Coverage: A yearly depression screening and preventive visit does not cost anything if your doctor or health care provider accepts assignment.
Comparing your Medicare options? Medicare.orgs information and resources can help make it easy to find the quality and affordable Medicare plan thats right for you. We offer free comparisons for Medicare Advantage Plans , Medicare Supplement Plans , and Medicare Prescription Drug Plans .
Get an online quote for Medicare plans that fit your health care needs today! Or call TTY 711 to get answers and guidance over the phone from an experienced licensed sales agent.
Other Mental Health Disability Benefit Programs
If you have a mental health disorder or illness which is disrupting your life and causing you financial stress, you should look into disability benefit programs. Many federal, state, and local initiatives provide assistance and financial support to individuals with mental health disabilities.
Some of these programs include:
- The SSAs Old-Age, Survivors, and Disability Insurance program, which provides monthly benefits to qualified retired and disabled workers, as well as their dependents and families of insured workers
- State-specific programs, such as Michigans Disability Assistance Program , which provide cash assistance to eligible adults who are 65 years old or older and have a disability
- Medicaid Section 1115 Demonstration programs, which provide qualified Medicaid beneficiaries with substance use or mental health services
- Private disability programs, which assist commercial insurers. These are often included in an employers benefits package and are ideal for individuals with partial disabilities.
There are also many programs available that can help you through the disability benefits application process. Children or adults who are at risk of homelessness and have a severe mental illness, medical impairment, or co-occurring substance use disorder, for instance, may qualify for the SSI/SSDI Outreach, Access, and Recovery . Under this program, case managers work closely with eligible individuals to help them secure SSI and SSDI benefits.
You May Like: Do Medicare Advantage Plans Cover Dentures
Which Outpatient Mental Health Care Services Does Medicare Cover
Medicare covers the following outpatient mental health care services:1
- Family counseling, when the goal is to help with treatment
- Psychiatric evaluation and diagnostic tests
- Outpatient treatment programs
- Medication management and certain medications that are not self-administered, like some injections
- For treatment of drug or alcohol abuse
- Partial hospitalization
What Mental Health Services Does Medicaid Cover
If you have Medicaid health coverage, can you get access to mental health services? Are you ineligible for the mental health services you need?
You can scour the web, and the truth is, its hard to find a solid answer one way or another if your Medicaid provider absolutely covers the treatment you are seeking.
Fear not.
You can get access to the services you need. You can take the first steps towards mental and emotional wellness with your Medicaid plan. Getting mental health services through Medicaid can actually be quite easy. While it seems daunting at first, in actuality, among nonelderly adults with mental illness or serious mental illness, those who have Medicaid are more likely than those without insurance or those with private insurance to receive both inpatient and outpatient treatment.
Here at Simple Intervention, we want you to rest easy there are solutions out there for you or your child to get the guidance and the treatment you need.
So what services are covered by your Medicaid plan? Well walk you through it.
Recommended Reading: How Does United Medicare Advisors Make Money
Youre Our First Priorityevery Time
We believe everyone should be able to make financial decisions with confidence. And while our site doesnt feature every company or financial product available on the market, were proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about , but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services.Here is a list of our partners.
Medicare Coverage Of Therapy And Mental Health Benefits
Contributing expert: Kelly Blackwell, Certified Senior Advisor®Medicare beneficiaries can access mental health care benefits through Original Medicare Part A for inpatient care and Part B for outpatient services or through a Medicare Advantage plan. Mental health coverage through Medicare supports optimal emotional, psychological, and social well-being.Updated: December 07, 2021
Kelly Blackwell
Kelly Blackwell is a Certified Senior Advisor ®. She has been a healthcare professional for over 30 years, with experience working as a bedside nurse and as a Clinical Manager. She has a passion for educating, assisting and advising seniors throughout the healthcare process.
You May Like: How To Enroll In Medicare Part B Online
How Does Medicares Mental Health Coverage Vary Across Different Plans
This table shows mental health coverage for different parts of Medicare:
| Type of plan | Medicare coverage |
|---|---|
| Medicare Part A | A stay at a general hospital or psychiatric facility. Part A will only cover inpatient psychiatric hospital costs for mental health disorders up to 190 days. This is the lifetime limit. |
| Medicare Part B | Outpatient services for therapy and other psychiatric treatments. Mental health visits with a clinical psychologist, clinical nurse specialist, psychiatrist, and other professionals are covered, as long as the provider accepts the assignment. |
| Medicare Advantage | These plans are an alternative to original Medicare and are sold by private insurers. They typically offer the same mental health benefits as Medicare Part A, Part B, and Part D. Some plans may come with additional benefits, such as dental and vision. Unlike original Medicare, there is an annual out-of-pocket limit. |
| Medicare Part D | Prescription drugs for mental illness. Medicare plans donât cover all drugs, but they typically cover anticonvulsant, antidepressant, and antipsychotic medications. |
| Medicare Supplement plans | A policy sold by private insurance companies to help pay for out-of-pocket mental healthcare costs â such as deductibles, copays, and coinsurance costs â after Medicare Part A and Part B pay their part. |
What are Medicareâs requirements for receiving mental health services?
-
Certified nurse-midwife
-
Transportation
How Does Medicare Cover Mental Health Services
Dear Marci,
I am new to Medicare. I have been receiving treatment for depression and anxiety for several years, and have gotten treatment in both inpatient and outpatient settings. Will these services be covered under Medicare? How much will they cost?
Dear Beau,
Medicare covers medically necessary mental health careservices and programs that are intended to help diagnose and treat mental health conditions.
If you have Original Medicare, Part A covers inpatient mental health services that you receive in either a psychiatric hospital or a general hospital. Your provider should determine which hospital setting you need. If you receive care in a psychiatric hospital, Medicare covers up to 190 days of inpatient care in your lifetime. If you have used your lifetime days but need additional mental health care, Medicare may cover your additional inpatient care at a general hospital.
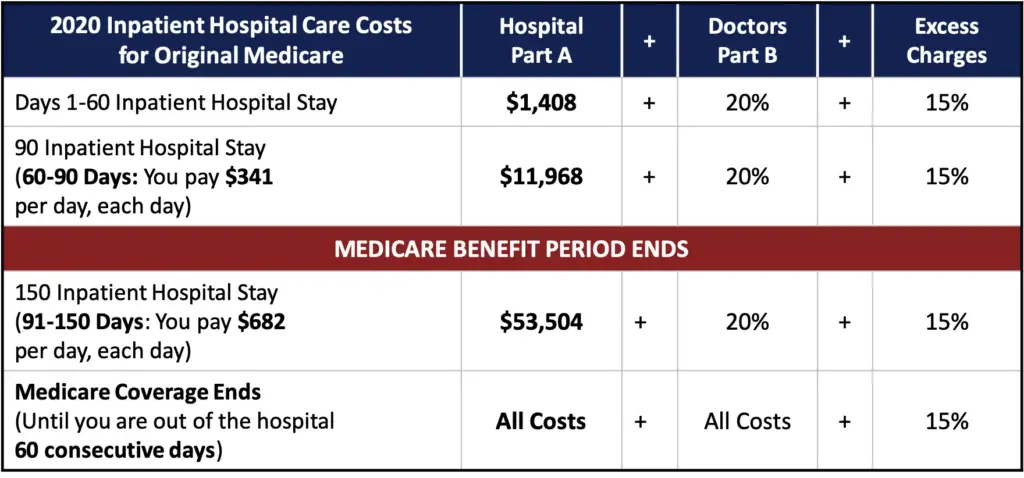
Be aware that you will have the same out-of-pocket costs with Original Medicare whether you receive care in a general or psychiatric hospital:
Recommended Reading: Is Medicare A Federal Program
How Your Location Impacts Your Mental Health Reimbursement Rate
Your location has an enormous impact on your contracted rate.
If you live in San Francisco, Los Angeles, Seattle, or many cities with high levels of education, there tend to be an abundance of mental health providers serving those locales.
On the other hand, if you are only one of a small handful of providers in a town, city, or state, you may see a significantly higher insurance reimbursement rate for psychotherapy.
Want to make the most money per session? You could move to Alaska.
Your location is one of the least flexible aspects that decides your contracted rate with insurance companies but it has a serious impact on your reimbursement rates for psychotherapy.
Consider this a business strategy question youll need to answer before settling on an office location.
The closer you are in proximity to under-served locales, the higher you can expect your rates to be priced.
If you are struggling to pick the right companies to increase your caseload, consider working with our mental health billing service to get these sorts of questions answered, along with all your billing, with way less headache along the way.
Will Your Mental Health Services Be Covered Through Medicaid
Every state Medicaid program provides some kinds of medical health services. Is your therapy covered by Medicaid? Are your Medicare mental health services covered?
Some states, like Virginia, offer substance use disorder services as part of their Medicaid plans. In Virginia, those who use Medicaid, FAMIS, and FAMIS MOMS are covered for Addiction and Recovery Treatment Services, known as ARTS. Through ARTS, our team at Simple Intervention can help you navigate a substance crisis and make the changes you need to reclaim your life from addiction or a substance abuse disorder.
While adults receive a fair amount of coverage for mental health services, children who are covered under FAMIS have a wider array of covered treatments. Because of this widespread coverage, if you are concerned about finding outpatient therapy for your child through FAMIS, we can get you the exact treatment your child needs.
Also Check: Is Social Security The Same As Medicare
The Basics Of Medicare And Mental Health Care Coverage
With that out of the way, here’s what you need to know about how Medicare does and doesn’t cover mental health care.
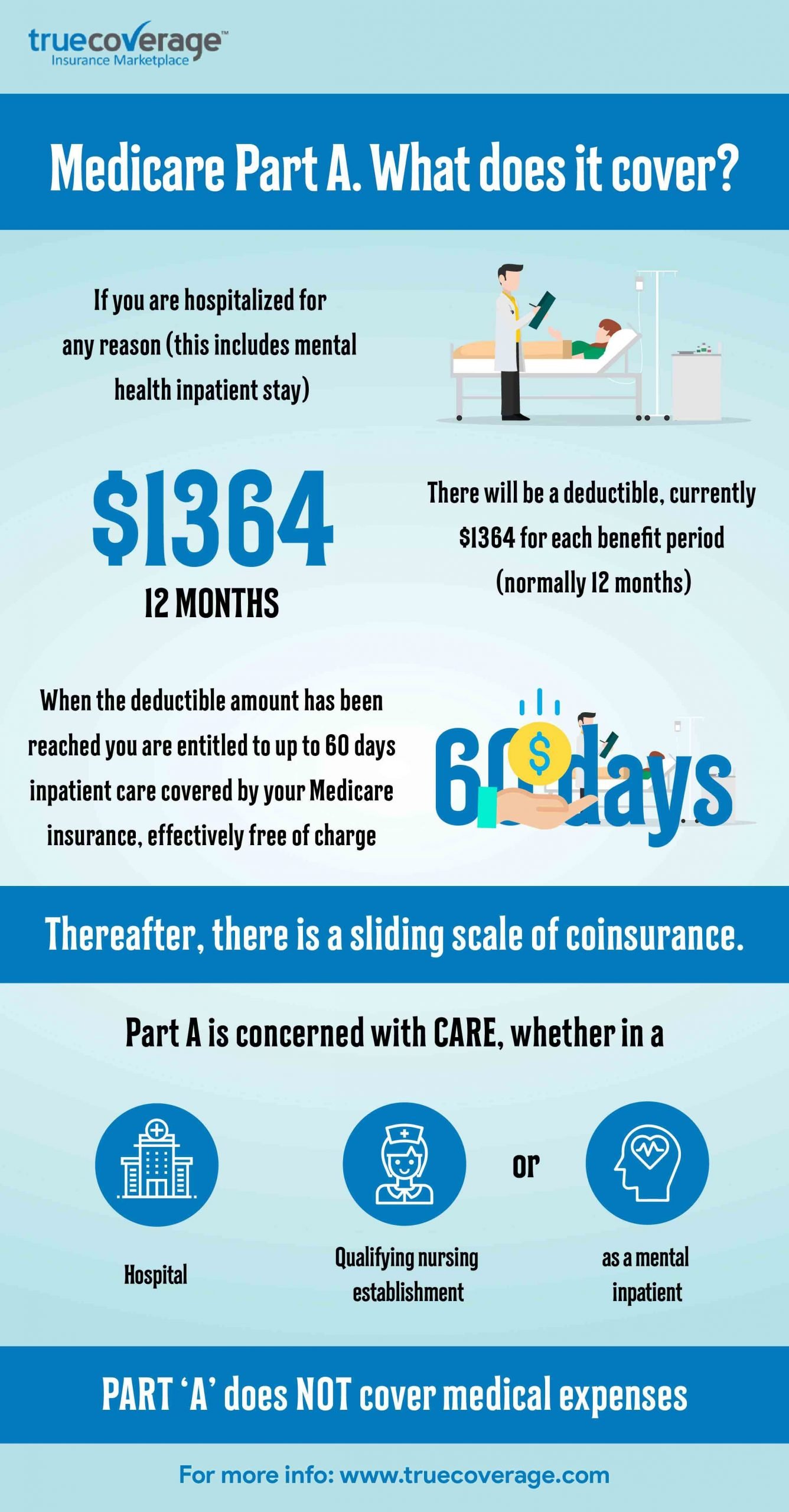
According to medicare.gov, Medicare Part A helps pay for the following during inpatient hospital stays:
- You room
- Nursing care
- Other related services and supplies
Medicare Part B, on the other hand, helps pay for mental health services provided outside of a hospital. A few examples:
- Psychiatrist or other physician appointments
- Clinical psychologist or clinical social worker visits
- Doctor-ordered lab tests
Something else Part B covers: partial hospitalization for people who require coordinated outpatient care.
Finally, Medicare Part D covers prescription drugs needed to treat a mental illness or mental health condition.
Does Medicare Cover Counseling
- Activity therapies like art, dance, and music therapy
- Family counseling to address a mental health condition
- Drugs that usually arent self-administered
- An annual depression screening with a primary care physician
- An annual alcohol misuse screening with a primary care physician
Medicare Part B has an annual deductible that changes over time. It was $183 in 2018 and is $233 in 2022. After the deductible, Medicare covers 80% of outpatient services and you have to pay 20% coinsurance on the Medicare-approved amount for the service you are receiving.
The standard monthly premium for Medicare Part B in 2022 is $170.10. This amount is usually deducted from your Social Security check.
You May Like: What Is The Requirement For Medicare
Mental Health Provider Demand Effecting Reimbursement Rates For Therapy
The sad truth is some of the best panels are totally full and their network map of mental health providers is saturated. Theres nothing you can do when a company like Florida Blue hasnt accepted mental health providers in years.
The amount of contracted providers per insurance company will have a larger influence on your ability to get in that network or not than it will on what youll be paid.
But on the other hand, if a company is easy to get accepted into their network, odds are higher they do not reimburse as much. Again, this is a case by case situation youll need to research and address.
Inpatient Mental Health Care
Hospital Insurance offers coverage for mental health care services that you receive in a hospital that requires you to be admitted as an inpatient. You can get inpatient mental health care services either in a psychiatric hospital or a general hospital that only takes care of people who have mental health conditions. Keep in mind that if you are in a psychiatric hospital instead of a general hospital, Medicare Part A only pays for up to 190 days of inpatient psychiatric hospital services during your lifetime.
For inpatient mental healthcare, Medicare doesnt cover a phone or television in your room, private duty nursing, a private room , and personal items .
Recommended Reading: How Much Money Can I Make On Medicare
Does Medicare Cover Therapy
Yes, Medicare covers therapy services. While the rate of coverage depends which Medicare plan you have many people receive their Medicare benefits through a health insurance company instead of directly from the government Medicare will typically help you pay for your therapy sessions.
With the federal Medicare plan, members who are enrolled in Part B receive coverage for outpatient mental health services. Medicare Part B is the medical coverage that helps pay for mental health screenings, diagnosis, and treatment including psychiatrist visits and medication management.
Does Medicare Advantage Cover Mental Health Care
Medicare Advantage does cover mental health care. While Medicare Advantage plans replace Original Medicare with a smaller, local network, they must cover what Medicare covers however, the costs for each service may vary. You will want to check with each plan to see how much Medicare Advantage will cost you for mental health services.
To learn more call a Senior65 agent at 800-930-7956.
Related Articles:
- New to Medicare: Everything you need to know. Medicare is the United States federal health insurance program for Americans 65 and older, as well as people with certain disabilities or End Stage Renal Disease .
- Pros and Cons of Medicare Advantage Finding the right Medicare insurance can be rather confusing for seniors – especially when parsing through the 150-page “Medicare and You” booklet that the government sends out as you approach age 65. We have made a list of the advantages and disadvantages of choosing a MA plan that should help
- Medicare Insurance Switching: Ultimate Guide With so many different plans, carriers, deductibles and what not, picking the wrong plan happens. A lot. Check out your options.
Recommended Reading: How To Find Out If I Have Medicare
Caring For Someone With A Mental Health Disorder
Caring for someone with a mental health issue can be challenging emotionally and financially.
Centrelink offers support through:
- Carer Payment – an income support payment if you give constant care to someone
- Carer Supplement – an extra yearly payment for some carers
- Carer Adjustment Payment – a one-off payment for carers of children under 7 with severe illness or major disability.
You can use the Carer Gateway website to find other kinds of support. This includes practical, social, and emotional help.
How Much Does Medicare Pay For Mental Health Care Services
An annual depression screening is free if the doctor accepts Medicare assignment. Otherwise, Medicare Part B pays 80 percent of the Medicare-approved amount for most covered mental health care services. You are responsible for the remaining 20 percent, and the Part B deductible applies.
Medicare Advantage plans also help pay for mental health care services and may cover additional mental health services or items. Check with your plan provider to get coverage and cost details.
Recommended Reading: Does Medicare Plan F Cover Acupuncture
Medicare Coverage Of Mental Health Services
A persons mental health refers to their state of psychological, emotional, and social well-being and its important to take care of it at every stage of life, from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered for mental health services through Medicare. Mental health services are a system of care that aim to assess, diagnose, treat, and counsel in an individual or group setting anyone who needs help alleviating mental or emotional illness, symptoms, conditions, and disorders. Find out what is included in your Medicare coverage for mental health services and get the help you or a loved one need.
