How Do I Read The Medicare Summary Notice
Its really two notices. Youll receive a separate MSN for your claims for Part A which helps pay for inpatient hospital care, inpatient care in a skilled nursing facility, certain home health care services and end-of-life hospice care and your claims for Part B .
The Part A Medicare summary notice shows the dates of the claims, how much of the deductible you have met, whether Medicare approved all of the claims, and the total amount you may be billed from the facility. It also lists the facilities where you have had claims this period and the dates you received services there.
Centers for Medicare & Medicaid Services
Page 2 includes tips for reviewing the notice and how many days of coverage you have used in your benefit period for inpatient hospitalization and skilled nursing facilities.
Page 3 provides detailed information about your claim, including the number of benefit days used, whether the claim was approved, any charges that werent covered, the amount Medicare paid and the maximum you may be billed. Keep in mind that the bill may be covered by Medigap or other supplemental coverage.
It shows the numbers for the three-month period covered in the summary notice and the total for the claim. It also shows the dates you went to the hospital or facility and when your current benefit period began.
Centers for Medicare & Medicaid Services
Centers for Medicare & Medicaid Services
Centers for Medicare & Medicaid Services
What Is The Difference Between Medicaid And Medicare
Medicare and Medicaid are different programs. Medicaid is not part of Medicare.
Heres how Medicaid works for people who are age 65 and older:
Its a federal and state program that helps pay for health care for people with limited income and assets. A basic difference is that Medicaid covers some benefits or services that Medicare doesnt like nursing home care or transportation to medical appointments .
Visit your states Medicaid/Medical Assistance website or medicare.gov for more information. Learn more in the article, Can I get help paying my Medicare costs?
When Do I Need To File Medicare Claim
Original Medicare has both participating and non-participating providers. Participating providers accept Medicares reimbursement plus your coinsurance as full payment, and have agreed to always bill Medicare for your care. Non-participating providers can charge you up to 115 percent of Medicares rate and dont have to file claims with Medicare, although some choose to do so. This means you may have to submit your own healthcare claim if you see a non-participating provider.
Read Also: How To Get Help Paying Your Medicare Premium
You May Like: Do I Need To Sign Up For Medicare Part B
How To Use Your Explanation Of Benefits
Your EOB shows you the costs for any medical services you received from the previous month, but its not a bill. You dont need to send any payments or take any action. It helps you track your medical costs and shows you how expenses are divided between your doctor, your health plan, and your copay.
Are Claim Filing Requirements Different If I Have Medicare Advantage Or Medigap
If you have Medicare Advantage, providers in the plans network have to bill your insurer for your care. As mentioned above, you may have to submit your own claims if you go out-of-network.
If you decide to file a claim yourself, first contact your insurer for its claims mailing address and any forms to include with your claim. Because Advantage plans have different time limits for filing claims than Original Medicare, be sure to follow your insurers rules to avoid a denial.
Original Medicare will automatically send your claims to most Medigap insurers for secondary payment, but some Medigap insurers require plan holders to manually file claims. If you have to submit your own Medigap claim, youll need to at least send the insurer a Medicare summary notice showing the payment Medicare made, and you may need to provide other documentation, such as an invoice or receipt. You dont have to submit an MSN when filing claims for Medigap services that arent covered by Original Medicare . Contact your Medigap insurer if you have questions about Medigap claims.
Recommended Reading: How Many Medicare Credits Do I Have
User License Agreement And Consent To Monitoring
End User Agreements for Providers
Some of the Provider information contained on the Noridian Medicare web site is copyrighted by the American Medical Association, the American Dental Association, and/or the American Hospital Association. This includes items such as CPT codes, CDT codes, ICD-10 and other UB-04 codes.
Before you can enter the Noridian Medicare site, please read and accept an agreement to abide by the copyright rules regarding the information you find within this site. If you choose not to accept the agreement, you will return to the Noridian Medicare home page.
THE LICENSES GRANTED HEREIN ARE EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THESE AGREEMENTS. BY CLICKING ABOVE ON THE LINK LABELED “I Accept”, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THESE AGREEMENTS.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK ABOVE ON THE LINK LABELED “I Do Not Accept” AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THESE AGREEMENTS CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, “YOU” AND “YOUR” REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
LICENSE FOR USE OF “PHYSICIANS’ CURRENT PROCEDURAL TERMINOLOGY”, FOURTH EDITION
Consent to Monitoring
Using Your Medicare Number To File A Claim
Medicare beneficiaries do not typically have to file claims on their own. A health care provider has one year from the day of service to file a claim on behalf of a patient. But if your claim is not filed in a timely manner, you may contact the provider to request that they file the claim.
If they still dont file the claim soon after your request, you may file the claim yourself by gathering and completing the Patient Request for Medical Payment form along with an itemized bill from the health care provider and a letter explaining your reason for filing the claim.
In order to submit the claim, you will need to look up the appropriate Medicare Administrative Contractor . MACs are private health care insurers that have been awarded a geographic jurisdiction to process Original Medicare claims.
Don’t Miss: What Does Medicare Part E Cover
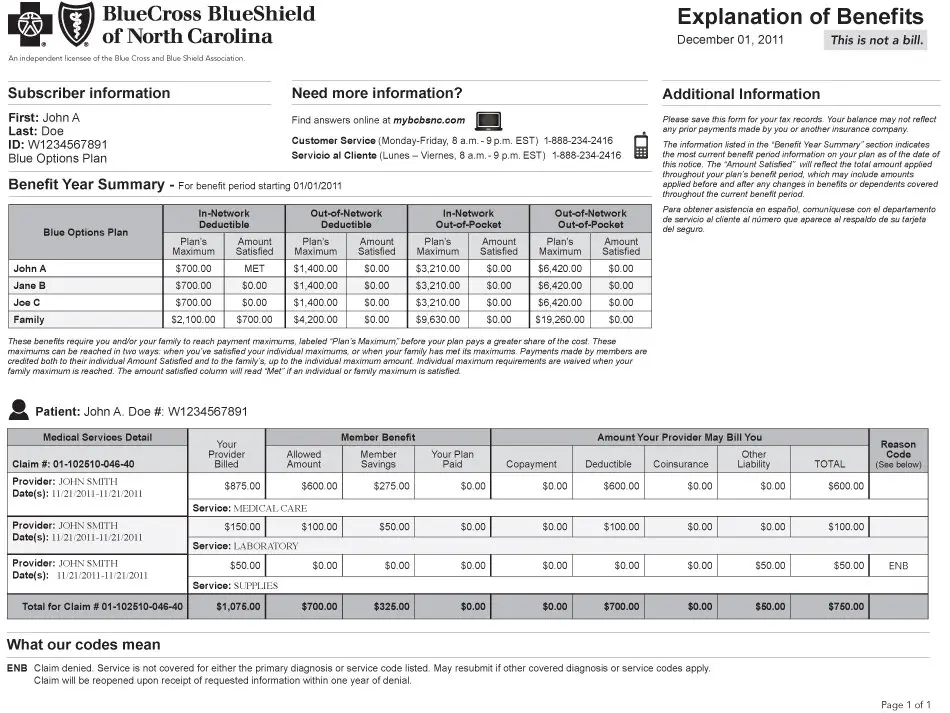
How Do I Read My Explanation Of Benefits Statement
Who is this for?
If you have a Blue Cross Blue Shield of Michigan or Blue Care Network Medicare plan, this information can help you understand the pieces and parts of your Medicare EOBs.
About once a month, youll receive an explanation of benefits, also called an EOB. Its a list of every time you visited the doctor, went to the hospital or filled a prescription, plus how much it all costs. Its important to remember that this statement isnt a bill. Its a tool to help you keep track of your plan usage. Well only send you statements when you use your coverage.
Coba Trading Partner Contact Information
The Coordination of Benefits Agreement Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the trading partners. The COBA Trading Partners document in the Download section below provides a list of automatic crossover trading partners in production, their identification number, and customer contact name and number. For additional information, click the COBA Trading Partners link.
Recommended Reading: What To Do Before You Turn 65 Medicare
Ama Disclaimer Of Warranties And Liabilities
CPT is provided âas isâ without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. The AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. The AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with Palmetto GBA or CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled âI Accept.â
Does Medicare Send An Eob
Each month that you fill a prescription with your Medicare drug plan, you will get an EOB in the mail. This letter provides you with an overview of your prescription medicine claims and associated costs. Learn more about the EOB by visiting their website. By login into your protected Medicare account, you may download and save your Part D claims information by pressing the Blue Button on the Medicare website.
Recommended Reading: Can You Have Two Medicare Advantage Plans
What Is In A Medicare Explanation Of Benefits
There are many different parts of your EOB. Regardless of where you get your plan, they will all include the same information.
First, it will list any prescriptions or medical services you received in the past month. Not only will it list your claims over the last month, but it will also show you the total cost of the services and how much you paid out of pocket.
If there are any updates to the medications covered by your plan, these updates will also be listed on your EOB.
It will also include a summary of the payments. As was mentioned before, it will show what costs you had to pay out of pocket. It will also show what your plan covered and what other organizations paid for.
What Should You Expect To See In The Msn
If youre enrolled in Original Medicare, you will receive an MSN instead of an EOB. An MSN shows similar information to an EOB.
Your MSN has a summary page containing:
- Starting date of the benefit period
- Status of claims, whether approved or denied
- How much you owe
Whether your MSN is for Part A or Part B, they usually follow the same format.
How is the Medicare EOB similar to the MSN? Just like the explanation of benefits, the MSN shows:
- Dates when you accessed healthcare services
- Claim status, whether approved or not
- Charges that Medicare does not cover
- Amount paid by Medicare
- The maximum amount to be billed
- Instructions for how to handle denied claims or file an appeal
Health insurance providers usually file claims on your behalf. However, it is still advisable to check for denied claims yourself. If you believe that your health plan should cover the claim, you can appeal. The appeals process for an MSN is similar to the process for Medicares explanation of benefits.
MSNs are released quarterly, but you can request monthly electronic MSNs for faster tracking.
Read Also: What Are The Guidelines For Medicare
Additional Information On Your Eob
These items arent on the example EOB here, but may be included in your EOB:
- Amount that may have been paid from spending accounts, such as a health reimbursement account , if applicable.
- A glossary of the terms and definitions included on your EOB, as well as instructions for how you can appeal a claim, if necessary.
- More specific details about filing an appeal in your state of residence.
- A summary of deductible and out of pocket maximums.
Video Result For Where To Get Champva Eobs
04C-Ad18 TRICARE Supplement Claims
Independent Practice Associations | V BILLINGS |…
J HELPS THE VA CHAMPVA Part V
MODIFIER IS INCONSISTENT WITH CPT CODE Scenario |…
AR CALLER 48 SCENARIOS PART 2 | DENIAL MANAGEMENT |…
AR CALLER E-book | medical billing materials | AR…
E-BOOK FOR AR CALLER | MEDICAL BILLING NOTES | DENIAL…
greatwww.cep.fsc.va.gov
totototototo
toto
toto
towhereto
Useful News
Op-Ed: Following L.A.’s freeways to the roots my immigrant grandparents planted for me, a mixed-race childYour browser indicates if you’ve visited this link
PizzaSacramento
California NewsYour browser indicates if you’ve visited this link
EXPLAINER: Why Court’s EPA-climate change ruling mattersYour browser indicates if you’ve visited this link
10 things you need to know about riding Amtrak overnightYour browser indicates if you’ve visited this link
California adds laws targeting ghost guns, sales to minorsYour browser indicates if you’ve visited this link
Also Check: How Old To Get Medicare And Medicaid
The Basics Of A Medicare Explanation Of Benefits
A Medicare Explanation of Benefits summarizes the items or services you received during a given time that were paid for by your Medicare Advantage or Part D plan. Typically, these are sent out by plans monthly and available online.
An EoB summarizes the items or services you received and how they were paid for by your Medicare Advantage or Part D plan.
Generally speaking, an EoB shows you what your plan billed Medicare, along with Medicareâs approved payment amount. Youâll also see what your Medicare paid and whatâs left that youâre expected to pay to your provider. Note, an EoB isnât a bill. In essence, itâs like a receipt for the Medicare services and items you recently used. Itâs also important to recognize that an EoB is different from a Medicare Summary Notice, which is a summary of coverage usage for a three-month period in Original Medicare.
Who Receives An Eob
Anyone enrolled in Medicare Advantage and Medicare Prescription Drug Plan will receive an EOB when they use their policy. You dont need to request an EOB you automatically receive an EOB the month after a claim, whether its from an office visit or a prescription.
Each plan has its own EOB form private insurance companies provide Medicare Advantage and Part D, and your EOB will come directly from them. If your MA plan and Part D plan are from different companies, youll receive an EOB for each.
Are you eligible for cost-saving Medicare subsidies?
Don’t Miss: What Is Original Medicare Mean
How To Read An Eob
EOBs may look different depending on your provider, but they generally include similar information. An EOB summarizes the items and services you accessed, the amount charged to Medicare, how much was covered by Medicare and how much you owe.
Below is a sample EOB with different sections labeled and explained.
After reviewing your EOB, if you have any questions or complaints, call your health insurance provider.
What To Do With The Notice
- If you have other insurance, check to see if it covers anything that Medicare didnt.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
- If an item or service is denied, call your medical providers office to make sure they submitted the correct information. If not, the office may resubmit.
- If you disagree with any decision made, you can file an appeal. On the last page of the MSN there are step-by-step directions on when and how to file an appeal.
Recommended Reading: When Can You Start Collecting Medicare
You May Like: Is Medicare Plan F Still Available
How Long To Keep An Eob
An article from the New York Times recommended keeping your EOB on file for at least one year to track payments, detect discrepancies and verify that bills have been paid in full.
If you plan to file for medical expense deductions, its recommended that you keep your EOB along with other tax documentation for six to seven years.
If youre not filing for medical tax deductions, youve fully paid your bills, and youre no longer seeking the services on your EOB, the National Association of Productivity & Organizing recommends shredding last years collection of EOBs.
For those with a serious medical condition that has improved, NAPO recommends keeping your EOBs for five years if you dont qualify for medical expense deductions.
Also Check: Is Stem Cell Treatment Covered By Medicare
How To Get Medicare Summary Notice Online
Make a login for your Medicare account. Select Get your Medicare Summary Notices electronically from the My messages area at the top of your account site, which is located under the My messages section. Youll be sent to the My communication options page, where you may check the box next to Change eMSN preference and then click Submit.
Contents
Read Also: Is Genetic Counseling Covered By Medicare
Coordination Of Benefits Overview
The Benefits Coordination & Recovery Center consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, , intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
All Medicare Secondary Payer claims investigations are initiated from and researched by the BCRC, and is not a function of the local Medicare claims paying office. This single-source development approach greatly reduces the number of duplicate MSP investigations. This also offers a centralized, one-stop customer service approach for all MSP-related inquiries, including those seeking general MSP information. The BCRC provides customer service to all callers from any source, including, but not limited to, beneficiaries, attorneys/other beneficiary representatives, employers, insurers, providers, and suppliers.