More Resources For Medicare Beneficiaries
When approaching the age to qualify for Medicare benefits, visit the official Social Security Administration Medicare website to determine your eligibility and calculate your premium. In the meantime, read more about when and how to apply for Medicare and visit medicare.gov to prepare for when that time comes.
Medicare Eligibility At Age 65
- You are at least 65 years old
- You are a U.S. citizen or a legal resident for at least five years
In order to receive premium-free Part A of Medicare, you must meet both of the above requirements and qualify for full Social Security or Railroad Retirement Board benefits, which requires working and paying Social Security taxes for at least 10 full years .
Learn more about Medicare eligibility at and before age 65 by referring to this helpful chart and reading more information below.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
Another type of Medicaid program is Early and Periodic Screening, Diagnostic, and Treatment . This program is available to individuals under the age of 21 who live in households that meet certain financial criteria. This type of Medicaid also has an age restriction and could therefore also be considered age-based.
ABD and EPSDT are required by federal law to be included in all state Medicaid programs. But as long as certain federal requirements are met, state Medicaid programs are free to offer their own Medicaid benefits and eligibility guidelines to people who might not otherwise be eligible for these two programs. Age may or may not play a role, depending on where you live.
For example, Medicaid in North Carolina is only available to those age 65 and over or 21 and under unless you are pregnant, are responsible for a child age 18 and under, disabled or require long-term care.
But in North Dakota, Medicaid is available to all low-income adults, regardless of age.
It could be said that Medicaid is age-based in some states and for some programs, but it is not universally age-based.
Also Check: Do You Have To Get Medicare At 65
What Medicaid Covers For Medicare Enrollees
Medicare has four basic forms of coverage:
- Part A: Pays for hospitalization costs
- Part B: Pays for physician services, lab and x-ray services, durable medical equipment, and outpatient and other services
- Part C: Medicare Advantage Plan offered by private companies approved by Medicare
- Part D: Assists with the cost of prescription drugs
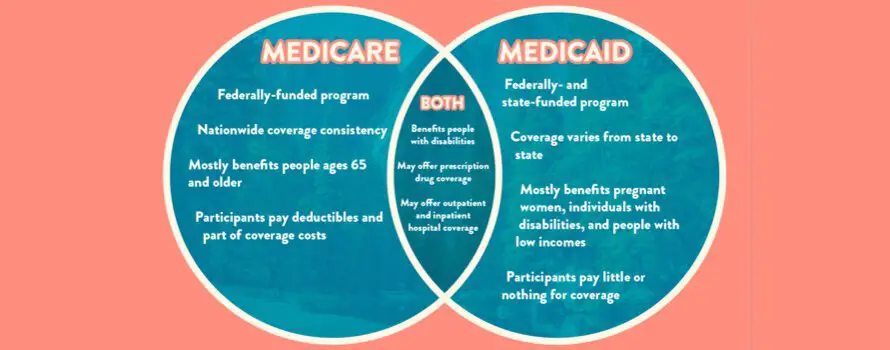
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid . Medicaid also covers additional services beyond those provided under Medicare, including nursing facility care beyond the 100-day limit or skilled nursing facility care that Medicare covers, prescription drugs, eyeglasses, and hearing aids. Services covered by both programs are first paid by Medicare with Medicaid filling in the difference up to the state’s payment limit.
Get Important News & Updates
Sign up for email and/or text notices of Medicaid and other FSSA news, reminders, and other important information. When registering your email, check the category on the drop-down list to receive notices of Medicaid updates check other areas of interest on the drop-down list to receive notices for other types of FSSA updates.
Also Check: Does Medicare Cover Dexcom G6
How Could Lowering The Medicare Age Affect People Eligible For Full Medicaid Benefits
What is current policy? Today, some people are eligible for both Medicare and full Medicaid benefits, while others may lose Medicaid eligibility once they become eligible for Medicare. A persons status as a Medicare beneficiary does not qualify them for full Medicaid benefits. Instead, a person must independently qualify for Medicaid through an eligibility pathway based on low income or disability. Individuals in the 60-64 age range may qualify for Medicaid through various pathways that may have different eligibility criteria and benefit packages. For example:
What are the key policy choices and implications? Lowering the age for Medicare would require policy choices about whether to allow individuals in the new age range to continue to receive full Medicaid benefits, if eligible under the ACA expansion or other poverty- or disability-related pathways, or whether these individuals would move from Medicaid to Medicare as their sole or primary source of coverage. How these eligibility issues are resolved has important implications for enrollee benefits and cost-sharing as well as state and federal costs . Additionally, Medicare enrollment is limited to specific periods, while Medicaid enrollment is open year-round. However, Medicaid eligibility must be periodically renewed, while Medicare eligibility currently continues without the need to renew eligibility once a person turns 65.
How Could Lowering The Medicare Age Affect Benefits For Current Medicaid Enrollees
What is current policy? Medicare and Medicaids benefit packages differ. Both cover inpatient and outpatient care and prescription drugs. Medicare generally includes wider participation of providers, though Medicaid drug coverage is broader. Medicaid also covers long-term care services in nursing homes and the community and specialty behavioral health services, which Medicare generally does not. Medicaid covers dental, vision, and hearing benefits for adults at state option. Traditional Medicare currently does not generally cover these benefits, although most Medicare Advantage plans do offer some dental, vision and hearing benefits. President Bidens budget calls for adding these benefits to Medicare. Medicaid rules also require states to recover the cost of long-term care benefits provided to people age 55 and older from the estates of deceased enrollees, and other costs may be subject to estate recovery at state option. Medicare does not require estate recovery, though it also does not cover long-term care services. The appeals process also differs between the two programs, with Medicaid allowing services to continue while an appeal is pending.
Don’t Miss: Are All Medicare Supplement Plan G The Same
What If Im Not Automatically Enrolled At 65
If your Medicare enrollment at 65 is not automatic, but you want to enroll, here are some more magic numbers.
3 and 7.
To start taking advantage of Medicare at 65, you need to sign up during the three months before the birthday month you turn 65. Those are the first three months of your seven-month Initial Enrollment Period.
Unless your birthday is on the first day of the month, your Initial Enrollment Period includes the three full months before turning 65, the month you turn 65, and the three months after you turn 65. If you were born on the first day of the month, IEP is the four months before your birth month, along with your birthday month and the two months after.
If you sign up during one of the months before your 65th birthday, your coverage will begin on the first day of the month you turn 65 .
Are you eligible for cost-saving Medicare subsidies?
How Could Lowering The Medicare Age Affect Out
What is current policy? The Medicare Savings Program is a Medicaid pathway that helps to cover Medicares premiums and/or cost-sharing requirements for current Medicare enrollees with low income and limited assets. This is an important consideration because Medicares premiums and cost-sharing are higher than those under Medicaid, which limits the populations who can be subject to premiums and has nominal cost-sharing. Box 1 summarizes current Medicare out-of-pocket costs and the assistance available through MSP.
Box 1: Medicare Out-of-Pocket Costs and the Medicare Savings Program
Medicare Part A, which covers inpatient hospital services, has an annual deductible of $1,484 in 2021. Medicare Part A also requires co-insurance for hospital stays over 60 days. Most Medicare beneficiaries qualify for Part A without a premium, based on their work history. Medicare Part B, which covers outpatient services, requires a monthly premium of $148.50 for most beneficiaries in 2021. Part B also requires an annual deductible of $203 in 2021 and co-insurance of 20% of the Medicare-approved cost of services after the deductible is met.
To help low-income enrollees afford Medicares out-of-pocket costs, state Medicaid programs must offer three MSP pathways:
Don’t Miss: What Medicare Supplement Plans Cover Hearing Aids
Adding Medicare Part C And Part D Plans
Medicare health plans are offered by private companies and provide additional benefits to those with Medicare Part A and Medicare Part B.Part C is the Medicare Advantage plan. To qualify for this plan, the individual must first qualify for Part A and Part B and must pay premiums, if applicable. In most cases, those with end-stage renal disease will not qualify.
Medicare Part D is prescription drug coverage. To qualify for this prescription drug plan, a person must first qualify for Part A and Part B and must pay premiums, if applicable.
How To Qualify For Medicaid
Almost every state has multiple Medicaid programs. But, as a good rule of thumb, if you make less than 100% to 200% of the federal poverty level and are pregnant, elderly, disabled, a parent/caretaker or a child, thereâs likely a program for you. And if you make less than 133% of the FPL**, thereâs possibly a program for you, depending on whether your state expanded Medicaid under Obamacare. In 2021, the federal poverty levels range from $12,880 to $44,660 .
In 2021, the federal poverty level in Alaska ranges from $ $16,090 to $55,850 . The federal poverty level in Hawaii ranges from $14,820 to $51,360 .
You May Like: Does Princeton House Accept Medicaid
You May Like: What Age Can I Qualify For Medicare
How Mepd Services Are Provided
If youre an adult with a disability and qualify for MEPD, these services are typically provided by STAR+PLUS. You will choose a STAR+PLUS health plan from the ones available in your service area.
If you have a child with a disability who qualifies for MEPD, these services are typically provided by STAR Kids. You will choose a STAR Kids health plan from the ones available in your service area.
You might also be enrolled into traditional Medicaid. Traditional Medicaid just means the state pays your doctors, nurses and other caregivers directly.
Full Retirement Age By Year
Full retirement age is the age you begin to receive full Social Security benefits. If you start to draw your Social Security benefits before reaching your full retirement age, the payment you receive will be less.
An easy way to think about full benefits and retirement age is this,
- Social Security will reduce your payments if you choose to receive your benefit before full retirement age. The percentage of reduced amount is highest at age 62 and decreases until you reach full retirement age.
- If you choose to receive Social Security payments when you reach full retirement, you will get the total amount.
- Suppose you choose not to receive Social Security payments when you reach full retirement and delay your benefit. In that case, you can increase the amount of your payment by earning delayed retirement credits.
If youre not sure when you reach full retirement age, our table provides the years and months you need to know for full retirement.
You May Like: How To Get Medicare To Pay For Hearing Aids
How To Apply For Medicaid
If youâre eligible for Medicaid, you can apply all year round through your states Medicaid website or HealthCare.gov, the federal health insurance marketplace. If you apply for Medicaid through Healthcare.gov and it looks like you qualify, the federal government will notify your state agency, which will contact you about enrollment. States also generally let you print out paper applications you can mail, fax or return directly to your local government office.
To complete your Medicaid application, you will likely need to provide documentation that you meet your states requirements. This documentation may include:
-
Your birth certificate or drivers license to serve as proof of age and citizenship
-
Recent pay stubs or tax returns to serve as proof of income
-
Copies of bank statements
-
Proof of address, which could include a lease, utility bill statements or a copy of your mortgage
-
Medical records to serve as proof of disability
States have 45 days to process your Medicaid application. They have 90 days if eligibility is tied to a disability . Processing can take longer if applicants do not supply all of the required documentation. If you dont qualify for Medicaid, you might be able to get subsidized health insurance through Healthcare.gov. However, only certain life events allow you to apply for a marketplace health care plan outside of open enrollment, which takes place from Nov. 1 to Jan. 15.
Free in your inbox each Friday.
Sign up now
Medicaid Eligibility And Costs
The federal and state partnership results in different Medicaid programs for each state. Through the Affordable Care Act , signed into law in 2010, President Barack Obama attempted to expand healthcare coverage to more Americans. As a result, all legal residents and citizens of the United States with incomes 138% below the poverty line qualify for coverage in Medicaid participating states.
While the ACA has worked to expand both federal funding and eligibility for Medicaid, the U.S. Supreme Court ruled that states are not required to participate in the expansion to continue receiving already established levels of Medicaid funding. As a result, many states have chosen not to expand funding levels and eligibility requirements.
Those covered by Medicaid pay nothing for covered services. Unlike Medicare, which is available to nearly every American of 65 years and over, Medicaid has strict eligibility requirements that vary by state.
However, because the program is designed to help the poor, many states have stringent requirements, including income restrictions. For a state-by-state breakdown of eligibility requirements, visit Medicaid.gov and BenefitsCheckUp.org.
Also Check: Does Medicare Advantage Cover Shingles Vaccine
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
Who Runs Medicare And Medicaid
The federal government runs the Medicare program. Each state runs its own Medicaid program. Thats why Medicare is basically the same all over the country, but Medicaid programs differ from state to state.
The Centers for Medicare and Medicaid Services, part of the federal government, runs the Medicare program. It also oversees each states Medicaid program to make sure it meets minimum federal standards.
Although each state designs and runs its own Medicaid program, all Medicaid programs must meet standards set by the federal government in order to get federal funds .
In order to make significant adjustments to their Medicaid programs, states must seek permission from the federal government via a waiver process.
Read Also: Is Medicare Available For Green Card Holders
Your First Chance To Sign Up
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Avoid the penaltyIf you miss your 7-month Initial Enrollment Period, you may have to wait to sign up and pay a monthly late enrollment penalty for as long as you have Part B coverage. The penalty goes up the longer you wait. You may also have to pay a penalty if you have to pay a Part A premium, also called Premium-Part A.
How Might Lowering The Medicare Age Affect Medicaid Enrollees
President Bidens FY 2022 budget proposes lowering the Medicare enrollment age from 65 to 60, and a group of over 150 House Democrats recently a provision lowering the Medicare age to 60 or 55 to be included in the Presidents American Families Plan. President Bidens budget proposes giving people age 60 and older the option to enroll in the Medicare program with the same premiums and benefits as current beneficiaries, but with financing separate from the Medicare Trust Fund. The Presidents budget proposal does not detail how lowering the Medicare age would work or be financed, or how it would affect current Medicaid spending and enrollees. While lowering the Medicare eligibility age based solely on work history to 60 could provide coverage to older adults who are currently uninsured or provide a more affordable option for people with private health insurance coverage, it also could affect Medicaid enrollees in this age range. Some Medicaid enrollees might lose Medicaid coverage when they gain Medicare, and others might become dually eligible for both programs, depending on the details of how it would work.
Also Check: How To Get A Wheelchair From Medicare
Medicare Enrollment Can Be Impacted By Social Security Benefits
Depending on your situation, you with either need to enroll in Medicare at age 65 or you may be able to delay. If you continue to work past age 65 and have creditable employer coverage , you can likely delay enrolling in Medicare until you lose that employer coverage. In most cases, people turning 65 will need to get Medicare during their 7-month Initial Enrollment Period to avoid financial penalties for enrolling late. Your IEP begins 3 months before the month of your 65th birthday and ends 3 months after.
Social Security benefits fit in the Medicare enrollment journey in one special way. If you are receiving either Social Security benefits for retirement or for disability, or Railroad Retirement Board benefits, you will be automatically enrolled in Medicare Part A and Part B when you first become eligible.