Does Medicare Cover Psychiatric Hospitalization
In severe cases of mental illness, a psychiatrist may determine a patient needs to be admitted to a psychiatric hospital or a general hospital for treatment and Medicare Part A may help pay for inpatient mental health services during a hospital or mental health facility stay. During the hospital stay, Medicare Part B may cover physician services provided.
Coverage: Medicare helps pay for mental health care in a psychiatric hospital up to 190 days. After this time, Medicare may pay for care in a general hospital. Out-of-pocket costs for a psychiatric hospital are the same as any other hospital for inpatient care that accepts Medicare assignment.
Caring For Someone With A Mental Health Disorder
Caring for someone with a mental health issue can be challenging emotionally and financially.
Centrelink offers support through:
- Carer Payment – an income support payment if you give constant care to someone
- Carer Supplement – an extra yearly payment for some carers
- Carer Adjustment Payment – a one-off payment for carers of children under 7 with severe illness or major disability.
You can use the Carer Gateway website to find other kinds of support. This includes practical, social, and emotional help.
Medigap Medsup And Mental Health Care
For starters, both Medigap and MedSup are terms for a product normally called Medicare supplement insurance.
As implied, this policy supplements the costs related to Original Medicare. To put it another way, it helps people pay for some of the expenses Medicare doesn’t cover.
Learn more about this type of plan in our “Medicare Supplement Insurance Policy FAQ.”
That’s true whether you’re talking about general health care or mental health care. For example, most Medigap plans cover the costs Medicare Parts A and B won’t pay for if you’re hospitalized for mental illness.
A few examples:
- All Medigap policies cover your Part A hospitalization copays and coinsurance
- They also cover all or part of your psychiatrists copays and coinsurance
- Most of these plans cover your Part A hospitalization deductible, too
MedSup and Medigap plans help if you’re ever get outpatient treatment for mental illness as well. Specifically, they usually cover some or all of your Part B out-of-pocket costs.
You May Like: How To Get A Power Wheelchair Through Medicare
Coverage Doesnt Guarantee Access
While Medicare covers mental health care, finding providers who accept Medicare as a form of payment for these services may be a struggle. Theres been an ongoing issue that folks cant seem to get a professional who accepts Medicare as payment for the mental health counseling and services they do deliver, says Kayrish.
How Much Does Medicare Reimburse For Psychiatrist
Medicare rebates of about $125 per standard consultation are available for up to 10 sessions, if a Medical Practitioner or Psychiatrist refers you through completing a Mental Health Care Plan. Alternatively, Private Health Fund rebates can be claimed if your policy covers you to see a Clinical Psychologist.
Read Also: What Does Medicare Part E Cover
Does Medicare Cover Mental Health Services In Tennessee
Yes, Medicare insurance covers mental health services, inpatient and outpatient, depending on your specific plans benefits.
Parts A and B of Medicare assist in paying for mental health services. Medicare Part A covers inpatient services and treatments administered in a psychiatric or general hospital, while Medicare Part B covers doctor visits and services that are considered outpatient.
Does Medicare Cover Marriage Counseling
Medicare generally only covers marriage or couples counseling in a very limited number of cases.
First, Medicare has only been reimbursing marriage and family therapists since 2019, and it currently only reimburses them for services provided to people with a primary substance use disorder diagnosis.
Second, Medicare only covers services linked to a primary psychiatric diagnosis listed in the Diagnostic and Statistical Manual of Mental Disorders . So, it wont cover any kind of marriage or family therapy from any kind of provider if it isnt required to treat a mental health condition.
This means that if you want to see a social worker or psychologist to address communication or other relationship issues that arent directly related to a mental health diagnosis, Medicare wont cover it.
Also Check: What Type Of Insurance Is Medicare Part D
Kathleen Cameron Senior Director At Ncoa
adults have been impacted pretty significantly, particularly by the social isolation and loneliness that they experience that could have exacerbated existing conditions that they had or in some cases, new diagnosis of depression, anxiety, sleep problems happened during the pandemic
For those on Medicare, knowing what mental health services are covered can make seeking help more daunting. Medicare beneficiaries might be aware that they have some sort of mental health coverage, but may not understand what it entails regarding services, co-payments, and prescriptions, says Lindsay Malzone, Medicare expert at Medigap.com.
To help navigate the ins and outs of Medicare, experts share insight.
Medicare Part D And Prescription Drug Coverage
Medicare Part D are plans run by private companies approved by Medicare. Since each plan can vary by coverage and cost, its important to know the details of your plan and how it applies to medication for mental health care.
Most plans have a list of drugs the plan covers. Although these plans are not required to cover all medications, most are required to cover medications which may be used for mental health care, such as:
- anticonvulsants
- antipsychotics
If your doctor prescribes a drug that yourplan doesnt cover, you canask for coverage determination and/or an exception.
Mental health care services typically not included under Medicare parts A and B are:
- private room
Recommended Reading: Where Do I Get A Medicare Card
How To Find Mental Health Providers That Accept Medicare Near Me In Tennessee
With Athena Care, gaining access to mental health testing services and treatments has never been easier. A care coordinator can assist you at one of our three mental health clinics in Tennessee: Nashville, Murfreesboro, or Hendersonville, open Monday through Friday, 8:00 a.m. to 5:30 p.m.
When choosing mental and behavioral health doctors in Tennessee, keep the following in mind:
- Education, training, license, and years of experience
- Specialties and services offered
- Insurance companies they work with
- Office hours
- Session length
Also, dont be afraid to ask questions.
Here youll find a list of practitioners organized by city, along with information about their backgrounds and specialties.
How Does Medicares Mental Health Coverage Vary Across Different Plans
This table shows mental health coverage for different parts of Medicare:
| Type of plan | Medicare coverage |
|---|---|
| Medicare Part A | A stay at a general hospital or psychiatric facility. Part A will only cover inpatient psychiatric hospital costs for mental health disorders up to 190 days. This is the lifetime limit. |
| Medicare Part B | Outpatient services for therapy and other psychiatric treatments. Mental health visits with a clinical psychologist, clinical nurse specialist, psychiatrist, and other professionals are covered, as long as the provider accepts the assignment. |
| Medicare Advantage | These plans are an alternative to original Medicare and are sold by private insurers. They typically offer the same mental health benefits as Medicare Part A, Part B, and Part D. Some plans may come with additional benefits, such as dental and vision. Unlike original Medicare, there is an annual out-of-pocket limit. |
| Medicare Part D | Prescription drugs for mental illness. Medicare plans donât cover all drugs, but they typically cover anticonvulsant, antidepressant, and antipsychotic medications. |
| Medicare Supplement plans | A policy sold by private insurance companies to help pay for out-of-pocket mental healthcare costs â such as deductibles, copays, and coinsurance costs â after Medicare Part A and Part B pay their part. |
What are Medicareâs requirements for receiving mental health services?
-
Certified nurse-midwife
-
Transportation
Recommended Reading: How Can A Provider Check Medicare Eligibility
Does Medicare Pay For Inpatient Mental Health Care
Inpatient mental health care administered at a general hospital or psychiatric hospital is covered by Medicare Part A.
There is no lifetime limit to the number of days a Medicare beneficiary can receive covered mental health treatment during inpatient hospital stays at a general health hospital.
When treated at a psychiatric hospital, Medicare coverage of mental health care is limited to 190 days over the course of your lifetime.
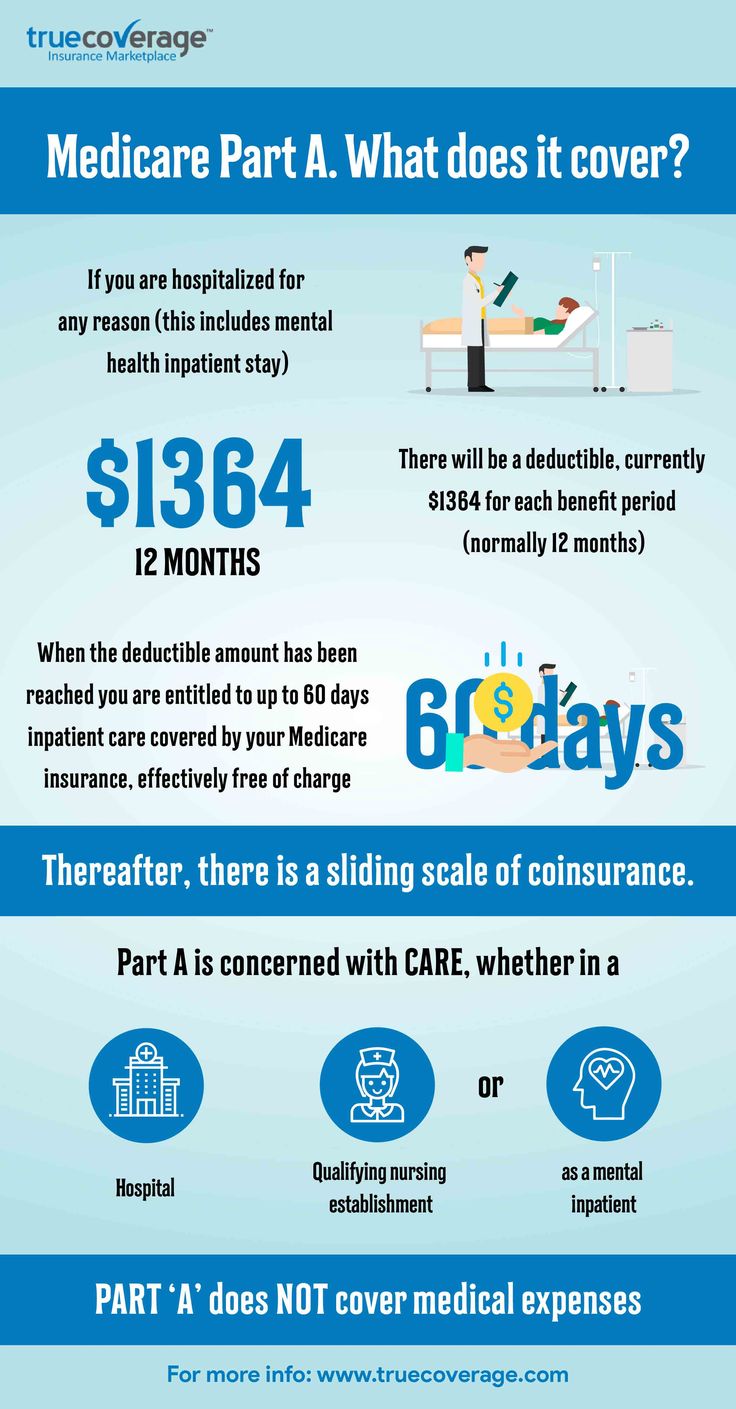
If you receive inpatient care that is covered by Medicare, you will be responsible for the Medicare Part A deductible, which is $1,408 per benefit period in 2020. If your inpatient hospital stay lasts longer than 60 days, youll then be required to pay additional Part A coinsurance costs.
If You Have Medicare And Need Mental Health Services What Can You Expect To Pay Out Of Pocket

Medicare doesnât cover 100% of the costs for mental health services. You will typically have to pay a monthly premium, annual deductible, and coinsurance. Your payment will all depend on the services you need. Medicare Part A covers hospital insurance, and Medicare Part B provides medical insurance for mental health services.
There are usually no monthly premiums for Medicare Part A. The reason is that most people work enough hours during their lifetime to qualify for premium-free Part A. This is 40 quarters â or 10 years â for either you or your spouse.
Medicare Part A has a deductible of $1,556 for 2022. This is for the admission to a hospital or psychiatric facility for each benefit period. A supplemental Medicare plan will cover part or all of the deductible.
| Over 90 days | $778 per day for up to 60 days.This is called the lifetime reserve. Medicare gives you a total of 60 reserve days during your lifetime. You are responsible for paying 100% of your costs after youâve used your lifetime reserve days. |
For example, suppose you spend 63 days in a psychiatric facility. You will pay the $1,556 deductible and $1,167 for 3 days of coinsurance. The total will be $2,723.
If you need psychotherapy and other mental health services, youâll need to review the costs of Medicare Part B.
You May Like: Does Medicare Pay For Vitamins
Using The Medicare Helpline
Medicare gives you special rights and resources for protecting them. These include:
- The Medicare Beneficiary Ombudsman
- The Competitive Acquisition Ombudsman
- The Beneficiary and Family Centered Care-Quality Improvement Organization
These resources provide information and advice to make informed healthcare decisions that best meet your needs and situation. They can also help you address and work through grievances with Medicare providers.
Does Medicare Cover Mental Health Care
Medicare Part B covers mental health services, such as screenings, counseling, reviews with your provider, telehealth, and more.
Plus, mental health visits you get from a doctor, psychiatrist, psychologist, social worker, nurse specialist, nurse practitioner, or physician assistant are covered under Medicare Part B.
Under Medicare Part B, youâll need to meet the deductible before Medicare starts paying for approved services. Additionally, Part B has a 20% coinsurance, meaning youâd be responsible for paying 20% of any approved services.
If you have a Medicare Supplement, the 20% coinsurance is likely covered .
In 2022, those with the popular Medicare Supplement Plan G would only be responsible for paying the $233 Part B deductible. All other out-of-pocket costs are covered by their Medigap plan.
You May Like: Why Sign Up For Medicare At 65
What Part Of Medicare Covers Mental Health Care
Medicare Part A covers mental health care in an inpatient setting. Part A mental health care is in a general hospital or a psychiatric hospital only for people with mental health concerns. If you get inpatient care in a psychiatric hospital, Part A will cover up to 190 days in a lifetime. There is no limit to the number of benefit periods you can have for mental health care in a general hospital.
Part A covers your room , meals, nursing care , therapy and treatment, lab tests, medications, and other services and supplies you need. Part A does not cover personal items or a phone or TV in your room.
Medicare Part B covers mental health care on an outpatient basis in these types of settings:
- A doctors or other health care providers office
- A hospital outpatient department
- A community mental health center
And from these types of providers :
- Psychiatrist or another doctor
- Clinical psychologist, social worker, or nurse specialist
- Nurse practitioner
- Physician assistant
Part B helps pay for these outpatient mental health services:
Part D helps cover self-administered prescribed drugs.
Medicare Advantage plans cover all services offered through Original Medicare Part A, Part B, and usually Part D. Copays and coinsurance amounts vary, depending on your plan. Providers and services must be in-network and typically require referrals and prior authorizations before you can receive services.
Medicare Part A: What Mental Healthcare Is Covered
Part A, often referred to as hospital insurance, covers your healthcare costs in an inpatient setting. This could be a general hospital or a psychiatric hospital. In either case, Original Medicare will cover you in the same way.
Medicare Part A will cover your room, meals, nursing care and therapy, lab tests, medications, and other forms of care that are necessary for your condition.
There is one central difference between being admitted to a psychiatric hospital and a general hospital: Medicare will only cover 190 days of psychiatric hospital stays over your lifetime. This is distinct from general hospital stays, which will renew in each benefit period.
You May Like: How To Calculate Medicare Tax
Medicare Inpatient Mental Health Services
If you do need inpatient care as part of your treatment, Medicare Part A covers services during an inpatient hospital or psychiatric hospital stay. Theres a limit to Medicare coverage if you stay at a psychiatric hospital thats dedicated to treating mental health patients, as opposed to a general hospital. Medicare Part A pays for up to 190 days of psychiatric hospital care in your lifetime.
Even during inpatient stays, Medicare Part B still covers certain mental health benefits, such as physician services.
Does Medicare Cover Behavioral Health And Substance Abuse Treatment
Medicare may cover the management of a behavioral health condition if the health care provider offers the Psychiatric Collaborative Care Model. This is a set of integrated services that provides care planning for behavioral health conditions, ongoing assessments, medication support, counseling and other treatments.
Part B covers an alcohol misuse screening once per year for those who use alcohol but dont meet the medical criteria for dependency. If its determined that you are misusing alcohol, you can receive up to four in-person counseling sessions each year.
Various treatments for substance abuse may be covered by Medicare Part A, Part B, Part D or Medicare Advantage for those who meet certain restrictions. These services may include:
- Patient education
You May Like: How To Get A Medicare Provider Number
Does Medicare Part A Cover Mental Health
Medicare Part A, your hospital insurance, covers mental health services that require your admission to a psychiatric or general hospital. If youre in a psychiatric hospital, youre covered for only up to 190 days of inpatient services over your lifetime.
Does Medicare Cover Mental Health Therapy

Yes, Medicare covers mental health care, which includes counseling or therapy. Depending on your needs, mental health care can be provided in a variety of settings. The goal is that you get the right kind of support when you need it.
Mental health pertains to our emotional, psychological, and social well-being. Our mental health can impact how we think, feel, and act. From a holistic, whole-person perspective, mental health plays a big part in our general overall health. Just as Medicare helps cover physical ailments, it also offers various benefits to support emotional, psychological, and social health.
Mental health concerns include anxiety and depression, substance abuse, eating and stress disorders, schizophrenia, and attention-deficit/hyperactivity disorders. These concerns can range from mild to severe and can be addressed on an outpatient or inpatient basis.
You can access mental health benefits through Original Medicare or Medicare Advantage plans, an alternative to Original Medicare. MA plans offer the same services, follow the same Medicare rules as Original Medicare, and generally require in-network providers, referrals, and prior authorization to receive benefits.
You May Like: What Does It Cost For Medicare Part B
Does Medicare Cover Psychologist Visits
Clinical psychologists diagnose and treat mental, emotional, and behavioral disorders and are one of the health care providers covered by Medicare Part B.
Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs. Check that your psychologist accepts assignment or is in your insurance providers network, otherwise Medicare will not pay for the services.
Medicare Plus A Medicare Supplement Plan Can Help You Save Money For Mental Health Treatment
Navigating mental health problems can be challenging, but Medicare helps ensure you have one less thing to worry about.
Original Medicare can cover common treatment options, and a Medicare Supplement plan can help ease your financial burden during this already stressful time by paying for certain Medicare deductibles, coinsurance, copays and more. That means you can focus on improving your mental health without worrying about the cost of treatment.
A licensed agent can help you decide on a Medicare option that works for you. Call today to speak with a licensed agent and compare the Medigap plans that are available where you live.
Also Check: How To Find A Dentist That Accepts Medicare
How Much Does Medicare Pay For Mental Health Care Services
An annual depression screening is free if the doctor accepts Medicare assignment. Otherwise, Medicare Part B pays 80 percent of the Medicare-approved amount for most covered mental health care services. You are responsible for the remaining 20 percent, and the Part B deductible applies.
Medicare Advantage plans also help pay for mental health care services and may cover additional mental health services or items. Check with your plan provider to get coverage and cost details.