What Is The Process For Purchasing Items In These Medicaid And State Funded Programs
As a participant in a program of this type, your loved one would get their doctor, or therapist, to provide a medical justification letter, saying that the equipment they want is medically necessary.
Your loved one would then contact a DME supplier, who is Medicaid-approved, and give them the medical justification letter form the doctor, or therapist.
The supplier would then fill out a Prior Approval application.
The document is sent to Medicaid at the state office where the purchase is either approved, or denied, and your loved one and the supplier would be notified.
If your loved one were unsuccessful, they will be notified as to the reasons why, and how to appeal the decision.
If your loved ones purchase were approved, unlike with Medicare, there would be nothing to pay.
American Disabilities Act Notice
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 , UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
Effective Date Of Coverage
Once an individual is determined eligible for Medicaid, coverage is effective either on the date of application or the first day of the month of application. Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
You May Like: Is Rollator Walker Covered By Medicare
Choosing A Home Health Care Agency
The next step is to find a home health care agency to provide you services. Heres where the type of Medicare you have matters.
- If you have a Medicare health plan, youll need to choose an agency that has a contract with your plan. Otherwise, Medicare might not pay the bill.
- Original Medicare lets you use any agency as long as its Medicare-certified
If your doctor cant suggest an agency, you can look at online ratings and compare.
Does Medicaid Cover Dentures For Adults
Dentures can offer a great opportunity to restore your smile, improve your bite alignment, and help you regain the ability to eat certain foods. Adults who receive health care through Medicaid services may be eligible for dental coverage in some states.
Common Types of Dentures
Dentures, which may also be called false teeth, are typically made from a composite material that can resist bacteria and breakage. The framework for dentures may be resin-based or a mixture of resin-based material with metal attachments. The teeth are usually a porcelain or ceramic that feels glass-like, which helps give an appearance that closely resembles natural tooth enamel.
Preparing for Dentures
All types of dentures require careful measurement so that they fit to the form of your mouth. When evaluating your potential need for dentures, its important to consider how long the process may take from start to finish.
If you need multiple extractions, your oral specialist may make a mold while you still have your existing teeth before they begin the extraction process. This can help shorten the time you spend waiting for your dentures after youre healed. Other oral specialists may prefer to wait until you have fully healed before trying to fit you for dentures, since the shape of your gums may change significantly.
Medicaid Coverage for Dentures
Related articles:
You May Like: Can You Receive Medicare Without Social Security
Letter Of Medical Necessity For An Air Purifier
In order to prove an air purifier is necessary for medical reasons, a doctor must write a Letter of Medical Necessity.
The letter must state that the air purifier is exclusively intended to treat, diagnose, mitigate, or cure a medical condition or disease.
For a Letter of Medical Necessity template, check out You must request this from a physician.
You cant write one up yourself and ask a doctor to sign it.
Even with this documentation, you are not guaranteed reimbursement.
For example, dependent FSA and limited care FSA will not cover air purifiers and will not reimburse you.
Examples Of Assistive Devices
The following are just a few examples of common activities and the types of assistive devices that can make them easier and safer:
- Bathing grab bars, hand-held shower head, bath seat with arm rails, non-slip floor mat.
- Dressing long-handled shoe-horn, velcro fastenings, sock pullers, rubber gloves .
- Preparing food easy-grip utensils, side-opening oven door, height-adjustable cupboards and counters, automatic-stop kettle, pouring aid.
- Moving/physical activities cane, walker, wheelchair, slip-resistant flooring
- Using the telephone loud-ringing phone, flashing light ring indicator, large numbers and buttons, automatic dialling.
- Enjoying hobbies playing card holder, long-handled gardening tools, television remote control with large buttons and a captioning button, modified keyboard that makes the computer more user-friendly, audio books, magnifying glass.
Recommended Reading: Does Medicare Cover Dexcom 6
Can One Have Dual Eligibility For Both Medicare And Medicaid
Yes, Medicare and Medicaid are not mutually exclusive programs. Persons who are eligible for both are referred to as having Dual Eligibility, Dual Eligibles, or often simply Duals. Medicare is the first payer of covered benefits, while Medicaid is the secondary payer. Typically, Medicaid will pay for Medicare premiums and co-payments for dual eligibles. In fact, many states have special programs intended to make it easier for seniors to manage their dual eligibility status as it can be confusing to know where to turn for what services. This is generally in the form of managed care.
There are also programs called Medicare Saving Programs for low-income seniors that dont quite qualify for Medicaid.
Aged & Disabled Federal Poverty Level Program
If you are aged or disabled and are not eligible for the SSI program, you may be able to get Medi-Cal through the Aged & Disabled Federal Poverty Level program. To qualify, you must:
This Medi-Cal program uses SSI countable income rules as well as a few extra rules you should know. For more information, visit the Medi-Cal section of the Disability Benefits 101 website.
You May Like: When Does Medicare Start For Seniors
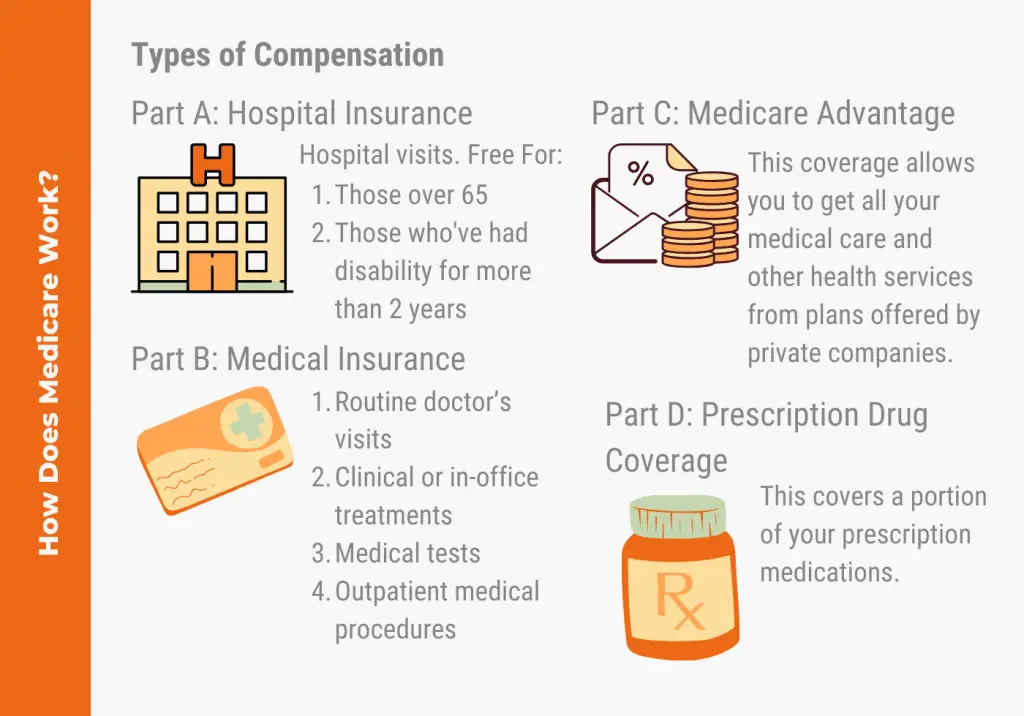
What Is Covered By Medicare Vs Medicaid
Medicare
Depends on the coverage you choose and may include:
- Care and services received as an inpatient in a hospital or skilled nursing facility
- Doctor visits, care and services received as an outpatient and some preventive care
- Prescription drugs
- Medicare Advantage plans: combine Part A and Part B coverage, and often include drug coverage , as wellall in one plan.
Medicaid
Each state creates its own Medicaid program, but has to follow federal guidelines, like the required and optional benefits they include. Some of the benefits Medicaid programs have to include are:
- Care and services received in a hospital or skilled nursing facility
- Care and services received in a federally-qualified health center, rural health clinic or freestanding birth center
- Doctor, nurse midwife, and certified pediatric and family nurse practitioner services
Medicaid Facilitates Access To Care
A large body of research shows that Medicaid beneficiaries have far better access to care than the uninsured and are less likely to postpone or go without needed care due to cost. Moreover, rates of access to care and satisfaction with care among Medicaid enrollees are comparable to rates for people with private insurance . Medicaid coverage of low-income pregnant women and children has contributed to dramatic in the U.S. A growing body of research indicates that Medicaid eligibility during childhood is associated with reduced teen mortality, improved long-run educational attainment, reduced disability, and lower rates of hospitalization and emergency department visits in later life. Benefits also include second-order fiscal effects such as increased tax collections due to higher earnings in adulthood. Research findings show that state Medicaid expansions to adults are associated with increased access to care, improved self-reported health, and reduced mortality among adults.
Figure 7: Nationally, Medicaid is comparable to private insurance for access to care the uninsured fare far less well.
You May Like: Does Kelsey Seybold Accept Medicare
How Else Can I Pay For Home Care
Besides Medicare and Medicaid, there are several programs and government aid options to help cover the costs of home care. Each has its own eligibility requirements and list of services it will cover. In addition, paying out of pocket is always an option, though many people will quickly find this cost-prohibitive without a plan to raise enough cash.
Quick Tip: To learn more about the costs of in-home care, visit our home care cost guide.
Reviewed By
I Have Been Receiving Health Care Through Medicaid Will I Lose This Coverage When I Become Eligible For Medicare
En español | You will not lose Medicaid eligibility just because you become entitled to Medicare. As long as your income falls under the limits for Medicaid eligibility in your state, you will receive both types of coverage. More than 8 million people have both Medicare and Medicaid.In this situation, Medicare becomes your primary insurance and settles your medical bills first and Medicaid become secondary, paying for services that Medicare doesnt cover and also paying most of your out-of-pocket expenses in Medicare .When you become eligible for Medicare, you must begin receiving your prescription drug coverage from Medicares Part D drug program, not from Medicaid. You will automatically qualify for the federal Extra Help program, which enables you to receive Part D drug coverage without paying premiums or deductibles and paying only low copays for your drugs. But to get this coverage, you still have to choose a Part D drug plan and enroll in it. To ensure that you pick a plan that gives you maximum coverage at the lowest cost, you may want to contact your state health insurance assistance program , which provides personal help from trained counselors on all Medicare and Medicaid issues free of charge. To find the main toll-free number of your SHIP , go to www.shiptacenter.org and select your state. For more information on the Extra Help program, see section 2 of AARPs consumer guide to the Part D program.
Don’t Miss: Can Medicare Take My Settlement
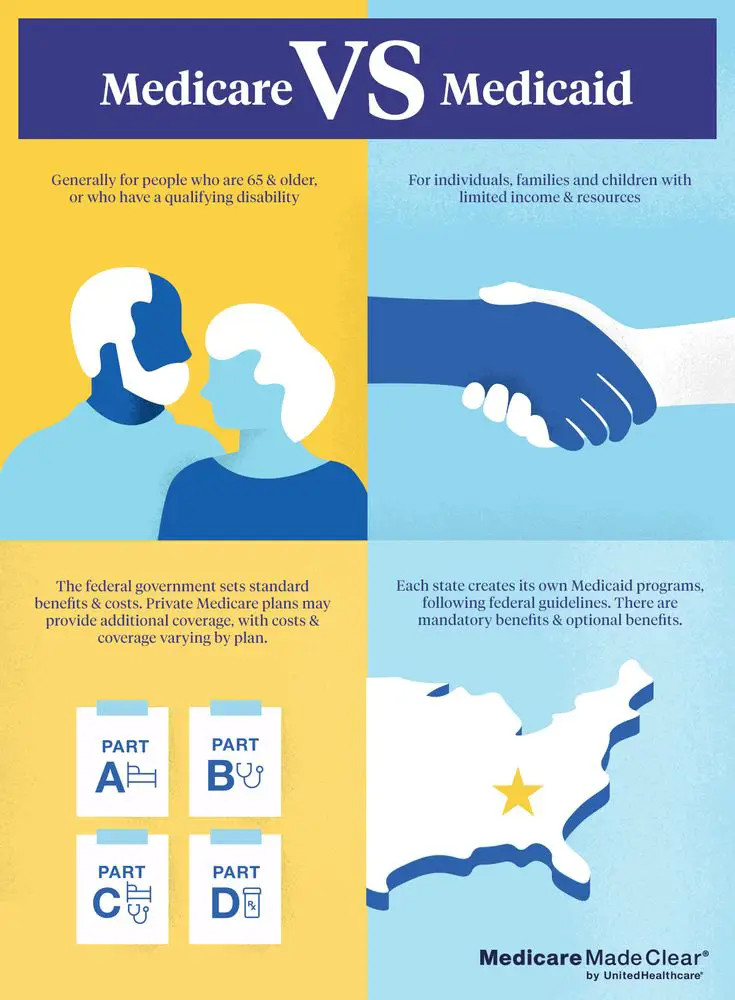
Medicare And Medicaid Coverage Explained
By Bethany K. Laurence, Attorney
Medicare and Medicaid are very different. Medicaid is a federal program for low-income, financially needy people, set up by the federal government and administered differently in each state.
Medicare was created to deal with the high medical costs that older citizens face relative to the rest of the population — especially troublesome given their reduced earning power. However, eligibility for Medicare is not tied to individual need. Rather, it is an entitlement program you are entitled to it because you or your spouse paid for it through Social Security taxes.
Although you may qualify for and receive coverage from both Medicare and Medicaid, you must meet separate eligibility requirements for each program being eligible for one program does not necessarily mean you are eligible for the other. If you qualify for both, Medicaid will pay for most Medicare Part A and B premiums, deductibles, and copayments.
The information below provides the basics of each program.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
Medicaid coverage can vary a bit from state to state, so a service or item that is covered in one state may not be covered in another. Optional benefits that may or may not be covered depending on the state include:
- Prescription drugs
- Physical and occupational therapy
- Respiratory care
- Speech, hearing and language disorder services
Again, coverage rules vary by state. If you would like to know if Medicaid will cover a particular service or item, contact your state Medicaid program for assistance.
Recommended Reading: Can You Use Medicare In Any State
Can A Person Have Both
A person can have both Medicare and private insurance at the same time. In these cases, Medicare establishes primary and secondary payers. The primary payer pays the claim first, while the secondary payer covers expenses that remain unfunded by the primary payer.
Medicare has various rules for establishing the primary payer. For example, Medicare is the primary payer when a person has private insurance through an employer with fewer than 20 employees. To determine their primary payer, a person should call their private insurer directly.
Medicaid Is Jointly Financed By States And The Federal Government
Medicaid is financed jointly by the federal government and states. The federal government matches state Medicaid spending. The federal match rate varies by state based on a federal formula and ranges from a minimum of 50% to nearly 75% in the poorest state. Under the ACA, the federal match rate for adults newly eligible was 100% for 2014-2016, phasing down gradually to 90% in 2020 and thereafter . The federal matching structure provides states with resources for coverage of their low-income residents and also permits state Medicaid programs to respond to demographic and economic shifts, changing coverage needs, technological innovations, public health emergencies such as the opioid addiction crisis, and disasters and other events beyond states control. The guaranteed availability of federal Medicaid matching funds eases budgetary pressures on states during recessionary periods when enrollment rises. Federal matching rates do not automatically adjust to economic shifts but Congress has twice raised them temporarily during downturns to strengthen support for states.
Total federal and state Medicaid spending was $577 billion in FY 2017. Medicaid is the third-largest domestic program in the federal budget, after Social Security and Medicare, accounting for 9.5% of federal spending in FY 2017. In 2017, Medicaid was the second-largest item in state budgets, after elementary and secondary education .
Figure 8: Medicaid is a budget item and a revenue item in state budgets.
Read Also: Are Walkers Covered By Medicare
How To Choose The Right Coverage For You
Although you may be eligible for both programs, in some cases, you might be in a position to choose between Medicare and Medicaid.
If youre eligible for Medicare, you have to choose between Original Medicare or Medicare Advantage, based on your preferences. But how do you decide? Take a look at some of the key differences.
What Are Dual Special Needs Plans
Dual health plans are also known as dual special needs plans. Theyre offered by private insurance companies, so you can find a dual health plan that best meets your health insurance needs. Being on a dual health plan does not change your Medicaid eligibility or benefits.
See UnitedHealthcare plans in your area.
Please note that the specific benefits dual health plans include can change depending on where you live. Search by your ZIP code to find the right plan to meet your health care needs.
Resource Center
Were here to help.
Contact us at:
Were here to help.
Contact us at:8 a.m. to 8 p.m. local time, 7 days a week.
Looking for the federal governments Medicaid website? Look here at Medicaid.gov.
Recommended Reading: When Does Permission To Contact Expire Medicare
Medicare Vs Private Insurance Out
Medicare out-of-pocket costs may include deductibles, coinsurance, monthly premiums, and copays for eligible healthcare treatments, items, and services, including prescription drugs. However, plans that private medical insurers offer generally have various rules about out-of-pocket expenses, including copays.
For example, health plans that private insurance companies administer usually put a limit on out-of-pocket costs, which means that after a person pays a certain amount in coinsurance fees, the insurance covers 100% of the costs for that benefit until the next membership period.
Original Medicare does not have an out-of-pocket maximum. This means that there is no cap on how much healthcare may cost due to copays for services.
The maximum out-of-pocket limit for Advantage plans in 2022 is $8,700 for one person and $17,400 for a family.
How Does Medicaid Affect Work Incentives
Medicaid supports work, evidence shows. Most Medicaid beneficiaries who can work do so: two-thirds of non-elderly adults enrolled in Medicaid who dont receive federal disability benefits live in a family with at least one worker. Moreover, one recent study found that people in states with more generous Medicaid eligibility levels and benefits are more likely to leave a job for another position with greater growth potential. This research suggests that comprehensive Medicaid coverage can support work and help beneficiaries take advantage of promising job opportunities without worrying about losing their coverage.
In 2018, the Trump Administration began encouraging states to take Medicaid coverage away from people who are not working or participating in work-related activities for a specified number of hours each month. In Arkansas, the first state to implement such a policy, more than 18,000 individuals lost coverage in the first seven months, before a federal court blocked the policy. Researchers found no significant increases in employment, number of hours worked, or overall rates of community engagement activities among those subject to the work requirement.
You May Like: Does Medicare Cover Insulin Pens
What Are The Disadvantages Of Medicaid
The list of services not covered by Medicaid is not the only downside to the program. Some other disadvantages of Medicaid include:
- Eligibility differs by state, so you may not qualify where you live but otherwise would if you lived in a different state.
- Benefits can change year to year based on budget cuts and other legislation.
- Options for providers may be limited and quality of care can be sometimes diminished.
