Will Medicare Pay For Home Health Care Aide
Home Health Aide. A home health aide is a worker who helps a patient at home with activities of daily living. Medicare does not pay separately for aides to perform custodial care, but they may do light housekeeping related to personal care during the visit. Medicare will not pay for home health aide services unless they are accompanied by
Home Health Services In Different Cities
One can apply for a demonstration program of Medicare. You can also request a review of your claim given in the program. The review might help you to decide whether Medicare is your home health aide or not. If your doctor recommends home health and you live in one of the states mentioned above in the U.S, you should immediately request the pre-claim review to know if you have to pay for the services.
Reach out Today at NewMedicare.
Iii Medicare Coverage Of In
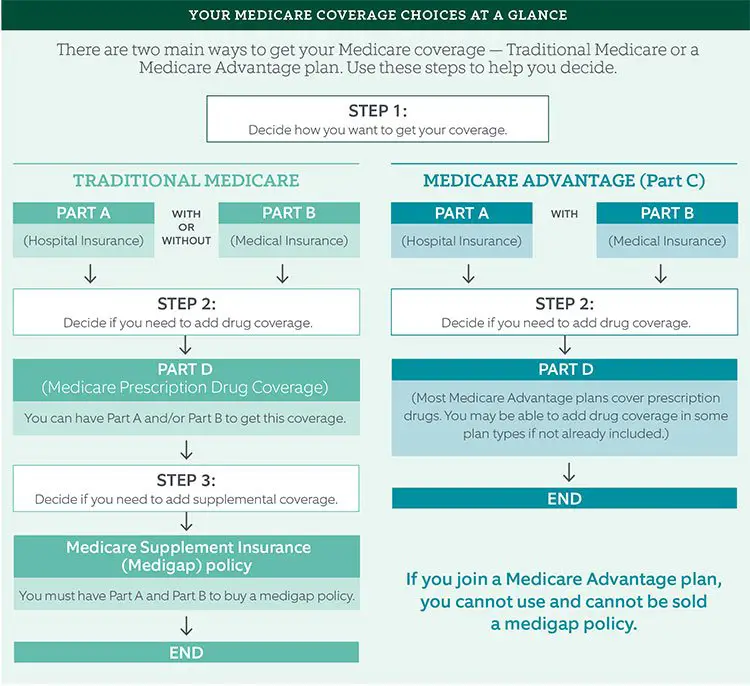
When it comes to Medicare coverage of in-home care, it is crucial to distinguish between standard home care and home health care. Medicare does not cover any standard in-home care because it is considered custodial care rather than health care. However, Medicare does cover eligible home health care services, which we explore in more detail below. Furthermore, in some cases, Medicare may actually cover custodial in-home care if delivered with home health care services from the same provider. Ultimately, seniors and their families should be aware that theyre unlikely to get help from Medicare paying for regular in-home care, but may have at least some home health care services covered by Medicare.
Read Also: How Much Does Medicare Cover For Surgery
Qualifying For Home Health Coverage
To be eligible for Medicare home health benefits, you must meet all of these conditions:
- You are homebound. That means you are unable to leave home without considerable effort or without the aid of another person or a device such as a wheelchair or a walker.
- You have been certified by a doctor, or by a medical professional who works directly with a doctor , as being in need of intermittent occupational therapy, physical therapy, skilled nursing care and/or speech-language therapy.
- That certificationarises from a documented, face-to-face encounter with the medical professional no more than 90 days before or 30 days after the start of home health care.
- You are under a plan of care that a doctor established and reviews regularly. The plan should include what services you need and how often, who will provide them, what supplies are required and what results the doctor expects.
- Medicare has approved the home health agency caring for you.
Is Home Health Aide Covered By Medicare
homemaker services, such as doing laundry, cleaning, or shopping personal care, such as help with bathing, getting dressed, or using the bathroom If personal care services from a home health aide are the only care you need, Medicare doesnt usually cover these. They do cover home medical care services.
Don’t Miss: Does Medicare Help Pay For Incontinence Supplies
Whos Eligible For Home Health Services
If you have Original Medicare , you may be eligible if:2
Note: If you need full-time skilled nursing care for a long time, its unlikely that youll be eligible for home health care services.3
The Medicare Home Health Benefit: An Unkept Promise
An in-home nurse cares for the mother of the photographer while she continues to recover from COVID-19 at her home on May 6, 2020, in Baltimore. Medicare rules state that if a beneficiary is considered homebound and requires skilled nursing, physical therapy, or speech language pathology services, he or she also can qualify for dependent services, including home health aides. Photo: Arturo Holmes via Getty Images
An in-home nurse cares for the mother of the photographer while she continues to recover from COVID-19 at her home on May 6, 2020, in Baltimore. Medicare rules state that if a beneficiary is considered homebound and requires skilled nursing, physical therapy, or speech language pathology services, he or she also can qualify for dependent services, including home health aides. Photo: Arturo Holmes via Getty Images
-
Associate Director, Center for Medicare Advocacy
-
Associate Director, Center for Medicare Advocacy
-
Misunderstandings about Medicare-covered home health care, along with changes in Medicare payment and regulations, have greatly restricted access to these important services
-
Home health benefits could help many beneficiaries with long-term or debilitating conditions, but a lack of information and misaligned incentives prevents them from receiving this care
You May Like: When Can I Change My Supplemental Medicare Insurance
How Much Does Medicare Pay For Home Health Care Per Hour
The average cost of home health care in 2022 is $21 per hour. However, this can significantly vary depending on the state. Medicare pays the entire approved amount of all home care and caregiver costs. In this regard, you will pay $0 for receiving any of the covered services. However, the in-home care must be part-time or intermittent.
How Much Does Home Health Care Cost With Medicare
Even if your home health care services are covered by Medicare, you may have to pay some money out of pocket.
Typically, youll pay $0 for Medicare-covered home health care services and 20% of the Medicare approved amount for durable medical equipment .
Ask your home health agency how much Medicare will pay before you begin receiving home health care. This can help prevent you from being surprised by unexpected out-of-pocket costs.
Recommended Reading: How Can I Contact Medicare By Telephone
Additional Help Available If You Are Moving Out Of A Nursing Home
If you enroll in one of the above waiver or PACE programs after you have been in a nursing home for more than 90 days, then you may be entitled to additional services aimed at transitioning you back to your home. You can get assistance making modifications to your house and with temporary rental payments while home modifications are being completed. These services are provided under Virginias Money Follows the Person program, a demonstration project administered by the Virginia Department of Medical Assistance Services. You can get these services if you are moving into your own home or apartment, your familys home or apartment, or a small community-based group home containing no more than four unrelated people.
What Home Care Services Does Medicare Cover
The primary objective of Medicares home care program is to provide seniors with short-term skilled services in the comfort of their own homes as an alternative to recovering in a hospital or skilled nursing facility.
Skilled nursing services are those that must be provided by a qualified health professional, such as a Registered Nurse or a Licensed Practical Nurse .
Examples of these services include:
- Monitoring of a patients vital signs and overall health
- Wound care for a pressure ulcer or surgical incision
- Administration of intravenous drugs or nutrition therapy
- Catheter changes
- Patient and caregiver education
Skilled therapy services are those that must be provided by or under the supervision of a licensed physical therapist, occupational therapist or speech-language therapist.
- Physical therapy exercises typically focus on improving and restoring strength, balance and range of motion for optimal physical function.
- Occupational therapy assists in regaining the ability to independently engage in activities of daily living and adapting these tasks or the surrounding environment to improve functionality and accessibility.
- Speech-language therapy helps patients regain the ability to speak and communicate as well as overcome swallowing difficulties .
Recommended Reading: Does Costco Pharmacy Accept Medicare
Home Health Services Covered By Original Medicare
If youre eligible for Medicare-covered home health care, services covered may include:4
- Part-time or intermittent skilled nursing care
- Physical therapy
- Part-time or intermittent home health aide services
- Injectable osteoporosis drugs for women
Note: Medicare will not pay for 24-hour-a-day care or meals delivered to your home. It also wont cover homemaker, custodial or personal care if thats the only care you need.5
What Home Health Aide Services Are Covered By Medicare
![What Wheelchairs Does Medicare Cover? [Helpful Guide] What Wheelchairs Does Medicare Cover? [Helpful Guide]](https://www.medicaretalk.net/wp-content/uploads/what-wheelchairs-does-medicare-cover-helpful-guide.jpeg)
Original Medicare generally only covers home health aide services such as skilled nursing care, occupational or physical therapy, or speech-language pathology services. If you only need home health aide services for help with bathing, dressing, and other activities of daily living , Original Medicare typically doesnt cover those services.
For example, lets say your doctor arranges for home nursing and physical therapy visits to help you recover from a stroke. Medicare may cover part-time, intermittent home health aide services if your doctor believes they are medically necessary for your treatment plan.
Also Check: Does Medicare Cover Dermatologist Check Ups
How Can I Get Help Paying For A Caregiver
If you or your loved one have exhausted your financial resources paying for in-home caregivers, you may be eligible for both Medicare and Medicaid.
Every state has at least one home- and community-based health services waiver program. If you meet the eligibility guidelines, this type of waiver program could help you pay for things like:
- help with daily personal care
- modifications to your home
- help with housekeeping
If you think you or someone in your family might need custodial care, you may want to consider a long-term care insurance policy to help you cover the cost.
A Medicare supplement plan may also help you pay some of the costs that Medicare wont cover.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
- Physical and occupational therapy
- Speech-language pathology services
Home health services are typically covered only if they are considered medically necessary by your doctor. A home health care agency can help you coordinate your home health services.
Don’t Miss: How Do I Apply For Medicare In Missouri
Will Medicare Cover Skilled Nursing Care
Medicare will pay for whats considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
Skilled nursing services are generally required to treat an illness or assist in the recovery of an injury. As the name implies, those who provide this care are licensed to administer medical treatment such as injections, catheter changes, wound dressings, and tube feedings.
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it wont cover 24-hour-a-day care.
Other Options In New York
The programs that provide Medicaid coverage for home care can vary widely from state to state. The following are some programs in New York that can help provide home care assistance to participants:
Managed Long-Term Care Program This is a Medicaid program designed to assist eligible participants with disabilities or chronic illnesses who choose to receive the necessary care at home instead of at a nursing home. New York Medicaid now provides most community based long term care services, including personal care assistants through the MTLC program. Effective July 1, 2012, the New York began to require people age 21 and older, eligible for Medicare and Medicaid, and in need of community-based long term care services for more than 120 days, to enroll in Managed Long Term Care plans. This program maximizes the assistance of caregivers in the family while providing other needed professional care from home health aides, skilled nurses, personal care assistants, and others authorized by your doctor. There are different plans within this program and you should discuss your home care needs with an experienced attorney to determine which plan is best for you. The MLTC agency will contract with a Licensed Home Care Agency to provide the services required.
Don’t Miss: Does Medicare Pay For Hearing Evaluation
Who Can Receive Which Services
You may be able to receive a service or participate in a program through your private health insurance, a managed care agency, Medicaid or Medicare – depending on whether you are financially and medically eligible and meet the criteria of the service or program you are interested in – or by paying for it yourself.
- Some services are available to persons who are eligible for Medicaid, have Medicare coverage, use their own funds , or have private health or long term care insurance.
- Some services are available only to persons who are eligible for Medicaid.
Home Health Aides Are Not Nurses
Although they do provide a certain type of care to patients, home health aides are not nurses and, therefore, they cannot provide any type of professional nursing care nor offer any medical advice to the patient or to the family and friends of the patient.
Home health aides follow a plan of care developed by a registered nurse who supervises the care provided by the home health aide. This means that an RN will likely be making joint visits with the home health aide from time to time in order to observe the care provided by the aide and to offer any further teaching if needed.
You May Like: Can You Get Medicare Advantage Without Part B
What Is Home Health Care
Home health care is care that occurs within your home and includes nursing services like infusions, medication management, post-surgical procedures and physical therapy. Its not the same thing as home care, which typically consists of supportive care and assistance with activities of daily living .
Home health care is primarily intended to treat an acute illness or injury. The goal is for the patients health to improve enough that they regain independence and, if thats not possible, to manage symptoms to help them become as self-sufficient as they can, according to Medicare.gov.
What You Pay For Home Health Services
All eligible Medicare recipients pay the following for home health services:6
- $0 for home health services
- 20% of the Medicare-approved amount for like a walker, wheelchair or hospital bed
Before home health care begins, your home health agency should explain your bill. This includes what Medicare will help cover, what Medicare wont cover and how much youll owe . The details of what isnt covered by Medicare must be given to you in an before you receive any uncovered items or services.7
You May Like: Do You Have To Sign Up For Medicare
How To Get Approved For In
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care.
You cant simply decide that you prefer your nursing care and other therapy needs in your home. You must meet the qualifications for in-home care, and they include the following
You Must Be Under The Care Of A Doctor:
The primary step in getting approved for in-home care is that you and the nursing plan must be under the care of a Medicare-approved doctor. This doesnt mean that the doctor will be at every visit. A home health nurse specialist will administer your plan, which your will create and regularly review.
Youre Homebound:
This is when youre unable to leave your house for treatment. Homebound patients require assistance from a person or piece of durable medical equipment such as a walker or wheelchair to get around the home or to get to services outside the home. Immobile people are considered homebound as well. A doctor can deem that youre homebound if he or she believes that your illness or condition could get worse if you left the home.
You Doctor Certifies That You Need Home Care:
You Dont Need Round-The-Clock Care:
Your In-Home Care Comes From An Approved Home Health Agency:
Which Medicare Parts And Plans Cover Home Health Care
If youre enrolled in Original Medicare, you will use both Part A and Part B to cover limited home health services, says Parker.
Some Medicare Advantage plans also offer additional benefits, such as caregiver support services or home modifications. However, the benefits offered for home health care vary widely from plan to plan, so its important to understand the coverage offered before you sign up for a Medicare Advantage plan, adds Parker.
Don’t Miss: Does Medicare Help Cover Assisted Living
Top Rated Assisted Living Communities By City
- Monthly Plan Premiums Start at $0
- Zero Cost, No Obligation eHealth Review
- Find Plans That Cover Your Doctors and Prescription Drugs
Medicare will cover 100% of the costs for medically necessary home health care, provided that care is part time or intermittent. The care needed must be less than seven days a week or less than eight hours a day over a period of 21 days. The average cost of home health care in 2022 is $21 per hour, but it can vary greatly by state.
Many seniors opt for home health care if they require some support but do not want to move into an assisted living community. For seniors who are generally in good health but require help with the activities of daily living, or someone to remind them to take medication, home health care is a viable solution.
Helpful Resources
