How Can You Know What Your Costs Will Be Before A Colonoscopy
Ask your doctors office for an estimate of costs before you have a colonoscopy. The billing department can usually estimate an average cost based on Medicare and other private insurance you may have.
If for any reason your doctors office thinks Medicare wont cover your colonoscopy costs, theyre required to give you a special notice called an Advance Beneficiary Notice of Noncoverage.
Another consideration is if youll receive anesthesia for the procedure. Anesthesia providers bill costs separately from the doctor performing the colonoscopy.
If you have insurance that requires an in-network doctor, you may also need to ask whos providing the anesthesia to ensure that your costs are covered.
If It Is A Preventive Screening
If you get your preventive colonoscopy from a healthcare provider who participates with Medicare and has agreed to accept assignment for Medicare-covered services, youll pay no copayment or deductible.11 Accepting assignment means that the provider agrees or is required by law to accept Medicare-approved amounts as payment in full. Most doctors who accept Medicare accept these payment terms, but its a good idea to confirm before you get services.
Two Sets Of Procedure Codes Used For Screening Colonoscopy:
CPT® code 45378
Colonoscopy, flexible, proximal to splenic flexure diagnostic, with or without collection of specimen by brushing or washing, with or without colon decompression
Healthcare Common Procedural Coding System codes G0105 and G0121
G0105 colorectal cancer screening colonoscopy on individual at high risk)
G0121 (colorectal cancer screening colonoscopy on individual not meeting the criteria for high risk.
Why two sets of codes in coding colonoscopy guidelines?
The Centers for Medicare and Medicaid Services developed the HCPCS codes to differentiate between screening and diagnostic colonoscopies in the Medicare population.
Common diagnosis codes for colorectal cancer screening include:
- Z12.11
- Z80.0
- Z86.010 .
Clinical scenario one:
A 70-year-old Medicare patient calls the surgeons office and requests a screening colonoscopy. The patients previous colonoscopy was at 59-years old, and was normal. The patient has no history of polyps or colorectal cancer and none of the patients siblings, parents or children has a history of polyps or colorectal cancer. The patient is eligible for a screening colonoscopy. Reportable procedure and diagnoses include:
- G0121, colorectal cancer screening colonoscopy on individual not meeting the criteria for high risk
- Z12.11, encounter for screening for malignant neoplasm of colon
| HCPCS and CPT® screening colonoscopy codes |
|
HCPCS/CPT® code |
| Personal history of colonic polyps |
Recommended Reading: Is Medicare Advantage A Good Choice
After Polyps Are Detected Patients May No Longer Qualify For Free Colonoscopies
By Michelle AndrewsJanuary 30, 2018
We encourage organizations to republish our content, free of charge. Heres what we ask:
You must credit us as the original publisher, with a hyperlink to our khn.org site. If possible, please include the original author and Kaiser Health News in the byline. Please preserve the hyperlinks in the story.
Have questions? Let us know at
Referrals & Prior Authorization
You can get many services without a referral from your Primary Care Provider . This means that your PCP does not need to arrange or approve these services for you. You can search for participating health partners using the Find a Doctor/Provider tool and schedule an appointment yourself. You can also check your provider directory for a list of participating health partners who offer these services.
Also Check: Will Medicare Pay For Drug Rehab
When And What Can I Eat After My Procedure
You can eat as soon as you leave the procedure facility. It is recommended that your first meal consist of relatively âlightâ food such as chicken soup, a turkey sandwich, or eggs & toast. Since you will have received sedation and your stomach will be empty, eating anything too rich or heavy might give you an upset stomach. You may resume your normal diet after the initial meal following your procedure.
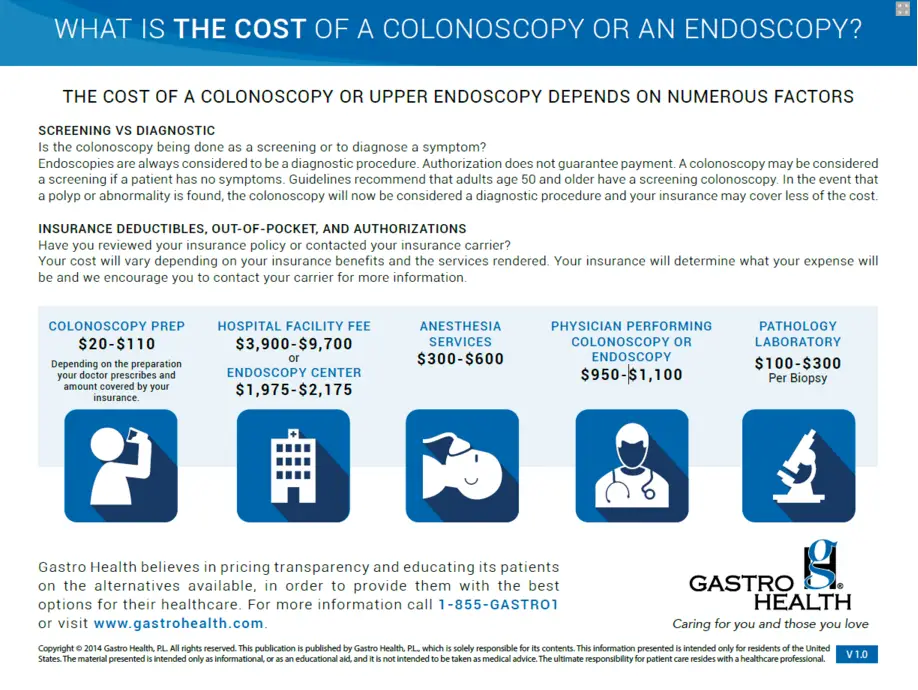
What Bills Will I Receive For My Procedure
You may receive up to four statements for different fees associated with your procedure:
Recommended Reading: Are Cancer Drugs Covered By Medicare
Covered Preventive Services That Include Cost
- Diabetes self-management training, for people at risk of diabetes complications. Youll pay your Part B deductible if you havent already met it for the year , plus 20 percent of Medicares cost for the training.
- Diagnostic mammogram . Youll pay your Part B deductible if you havent already met it for the year, plus 20 percent of the cost of the screening.
- Digital rectal exam for prostate cancer .
- Glaucoma test if you are at risk. Youll pay your part B deductible if you havent already met it for the year, plus 20 percent of the cost of the screening. A copay may also apply if the screening is conducted in a hospital outpatient setting.
If youre enrolled in a Medigap plan, it may pay some or all of the Part B charges incurred for these services.
What Does Medicare Consider High Risk For Colon Cancer
The Centers for Medicare and Medicaid Services consider people to be high-risk if they have or have had any of the following:
- A personal or family history of colon cancer
- A personal history of inflammatory bowel disease such as Crohns Disease
- A sibling, parent or child whos had colon cancer or an adenomatous polyp
- A personal or family history of adenomatous polyposis
You May Like: Does Medicare Pay For Ensure
What Is The Medicareco
Technically, there is no co-pay for a colonoscopy under Medicare. As stated previously, Medicare will cover the entire cost of a colonoscopy, so long as the procedure is preventative. If any polyps or abnormalities present themselves during the procedure, the procedure will become diagnostic, and you will be responsible for out-of-pocket costs equal to a 20 percent coinsurance.
In terms of co-payments, you would be responsible for a co-payment if your colonoscopy procedure is done in the hospital. If you have Medigap , part or all of your copayment may be covered.
Coverage For Medications Related To A Colonoscopy
If this laxative is ordered by prescription, Medicare Part D may provide coverage. If you purchase a laxative over the counter, you may be responsible for the total cost of the purchase.Any medications administered during the course of the colonoscopy, including sedatives, will be covered by Medicare as part of the outpatient procedure itself. If medications are required after a colonoscopy to treat any conditions found during the procedure, Medicare Part D would apply toward these drugs as long as they are listed in your plans formulary and are purchased from a retail pharmacy for home use.
Don’t Miss: Should I Enroll In Medicare If I Have Employer Insurance
What Are The Benefits Of Direct Access Colonoscopy
Direct Access Colonoscopy offers many benefits to patients and physicians.
First, it empowers patients to take charge of this preventive health screening and schedule it on their own time.
It saves you time because you don’t need to make an appointment with your GI doctor in the office, said Dr. Swaroop. This type of colonoscopy saves you money, too, as you avoid paying a co-pay and other related expenses.
Direct Access Colonoscopies also enable doctors to perform endoscopic procedures in a timely and efficient manner while maintaining the highest quality standards.
Single Course Of Treatment

A referral covers a single course of treatment for the referred condition. A single course of treatment is an initial attendance at the specialist or consultant physician. It includes subsequent attendances for the continuing management until the patient is referred back to the referring practitioner.
A new referral doesnt always mean a new course of treatment.
If a referral is for continuing management of a condition, the specialist or consultant physician must bill subsequent attendance items. However, you can bill an initial attendance item if it meets all the following:
- the referring practitioner decides the patients condition needs to be reviewed
- the patient is seen by the specialist or consultant physician after the expiry of the last referral
- the patient was last seen by the specialist or consultant physician more than 9 months earlier.
If the patient has a new or unrelated condition, the specialist can start a new course of treatment if there is a new referral in place.
Recommended Reading: How Can I Get My Medicare Card Number
Medicare Coverage For Colorectal Cancer Screening
Medicare covers an initial preventive physical exam for all new Medicare beneficiaries. It must be done within one year of enrolling in Medicare. The Welcome to Medicare physical includes referrals for preventive services already covered under Medicare, including colorectal cancer screening tests.
If youve had Medicare Part B for longer than 12 months, a yearly wellness visit is covered without any cost. This visit is used to develop or update a personalized prevention plan to prevent disease and disability. Your provider should discuss a screening schedule with you for preventive services you should have, including colorectal cancer screening.
Types Of Medicare Advantage Plans
Congress authorized Medicare Part C to bring wider choices for senior consumers. The wanted the private sector to offer innovative approaches that provided new or additional benefits and cost savings. The Medicare Advantage insurers used a number of management approaches to allocating resources.
The insurers created options that would emphasize costs, flexibility, and user choice. They include the HMO, PPO, PFFS, and HMOPOS. The below listed items describe Medicare Advantage types of plans and whether they require referrals.
- HMO stands for Health Maintenance Organization. The HMO type of care plan requires a primary care physician and referrals for network resources
- HMOPOS plans are health maintenance plans with the Point of Service option. The primary care physician can make referrals network resources, but also to outside resources. The insurance covers them at a higher cost to the consumer.
- PPO, or preferred provider Organization, gives higher insurance payment for network resources and lower payments when users go outside of the network. Users do not need referrals for specialists.
- PFFS plans, or Private Fee-for-Service Plans do not require referrals subscribers can go to doctors that agree to the group terms.
Don’t Miss: What Medications Are Covered By Medicare
What Does Medicare Consider High Risk For Colonoscopy
Medicare covers colonoscopy screenings the most frequently for any high-risk patient.
The Centers for Medicare and Medicaid Services identifies you as high-risk if you meet one or more of the following:
- Having an immediate family member who has or had colorectal cancer or polyps. Direct family such as a child, sibling, or parent.
- Have a family history of colorectal cancer a family history of familial adenomatous polyps or having Lynch syndrome.
My Friend Recently Had A Procedure And His/her Prep Was Different Than Mine Why
Different physicians prefer different preparations for colonoscopy. You should follow the preparation instructions exactly as it was prescribed for you. Our physicians have a lot of experience in using the different colonoscopy preparations and have decided upon using SUPREPor MOVIPREP because of its low total volume and superior cleansing results. Any questions you have should be directed to our staff.
Recommended Reading: When Does Medicare Coverage Start
Prices Are All Over The Map
The prices vary widely: Weve found as little as $600 all in, and as much as $8,000 or even more .
There are links to our detailed price lists in this post from clearhealthcosts.com .
Here are examples from our community members reporting:
Charge of $3,200 individual paid $370.41: $3,200 was billed and $2,331 was the allowed amount under my health care plan . However, I received a separate bill from my doctor who performed the procedure for $800 and the allowed amount by my insurance was $370.41 which went to my deductible. because they found a polyp the procedure coding changed from preventive to diagnostic, therefore, I was no longer covered under preventive care.
Charge of $8,000 individual paid $800: I spoke to the CEO of the surgical center. He agreed the fee was high but said there is a standard list of prices that he and most centers adhere to.
Charge of $2,312 individual paid $844: Was charged three initial different fees, for MD, facility, and lab work, all reduced via contract, not payment: 426, reduced to 285 1400, reduced to 279, and 486 reduced to 280, thus $2312 overall reduced to $844, zero by carrier.
Charge of $2,722, insurance paid $743, individual paid $1,979: I did not shop around when I did this. Im embarrassed to admit that it hadnt occurred to me to do that. This price check concept is a wonderful service and eye opener for the public. Many thanks.
Tests That Primarily Detect Cancer
- Annual fecal immunochemical test with high test sensitivity for cancer or
- Annual guaiac-based fecal occult blood test with high sensitivity for cancer or
- Stool DNA test with high sensitivity for cancer, interval uncertain.
The USPSTF found convincing evidence that screening for colorectal cancer in adults aged 50 to 75 years reduces colorectal cancer mortality. The USPSTF found no head-to-head studies demonstrating that any of the screening strategies it considered are more effective than others, although the tests have varying levels of evidence supporting their effectiveness, as well as different strengths and limitations:
- Colonoscopy every 10 years
- CT colonography every 5 years
- Flexible sigmoidoscopy every 5 years
- Flexible sigmoidoscopy every 10 years plus fecal immuohistochemical test every year
- Guiaic-based fecal occult blood test every year
- FIT test every year
- Stool DNA every one or three years.
Read Also: Who Can Get Medicare Part D
Does Medicaid Require Prior Authorization For Referrals
Today in the United States, Medicaid covers over 17 percent of all U.S. healthcare spending and assists with healthcare expenses for more than 75 million Americans of all ages. Where Medicare is a health insurance program, Medicaid is an assistance program that helps low income individuals and families with their medical needs and expenses.
Every U.S. state runs its own Medicaid program, but they are all based on federal guidelines. Each state has its own regulations regarding what services are covered, when written referrals are necessary, and which referrals require prior authorization.
Through Medicaid services, a referral is issued in writing by your primary care physician when he or she feels it is necessary for you to visit another health care provider for treatment or tests. A prior authorization for this referral is necessary in some cases. The authorization is issued by your Medicaid provider who reviews the case and allows you to visit the specialist or other health care provider.
Because states may vary in their requirements for coverage of services, referral allowances, and need for prior authorization, you should contact your local Medicaid office for details. Your health care provider can give you information also.
Non-formulary medications Hospice care Specialized care
If you need emergency room services or post stabilization services, these do not require prior authorization.
Related articles:
If It Is A Diagnostic Screening

If your doctor finds and removes a polyp or other tissue during your colonoscopy, Medicare considers it diagnostic,12 even if you went in for a preventive screening. For diagnostic colonoscopies, you may pay coinsurance 20% of the bill plus a copayment if you get your colonoscopy in a hospital. Your Part B deductible does not apply.
Don’t Miss: Is Prolia Covered By Medicare Part B Or Part D
What Do I Need To Bring With Me For My Procedure
Please bring a list of your current medications including over-the-counter medicines, as well as a current copy of your insurance card. It is advisable for you to bring the phone number of the person who will be picking you up after the procedure . Dress in comfortable clothing. Do not wear jewelry or finger nail polish.
Get Extra Coverage On Your Medicare Colonoscopy Screening
New, current, and future recipients can all use a helping hand in the Medicare world. Thats why were here!
Those that need a Medicare Colonoscopy Screening and have a Medigap plan could have little costs.
Give us a call today at the number above to learn more. Our team of agents can help compare plans near you and give you the best options.
Cant call right now? We get it complete our online rate form and get a free consultation with an agent today!
- Was this article helpful ?
Disclaimer: By clicking the button above, you consent to receive emails, text messages and/or phone calls via automated telephone dialing system or by artificial/pre-recorded message from representatives or licensed insurance agents of Elite Insurance Partners LLC, its affiliates or third-party partners at the email address and telephone number provided, including your wireless number , regarding Medicare Supplement Insurance, Medicare Advantage, Medicare Part D and/or other insurance plans. Your consent is not a condition of purchase and you may revoke your consent at any time. This program is subject to our Privacy Policy and Terms of Use. This website is not connected with the federal government or the federal Medicare program.
Recommended Reading: Do You Have Dental With Medicare
