Medicare Coverage For Nursing Home Care
It is not that Medicare does not pay for any nursing home care. It does pay for some, but only if you were recently admitted to the hospital and only if you require skilled care at least five days per week.
Not only do you need to have been hospitalized to qualify for this Medicare Part A coverage, but you need to have been admitted as an inpatient for at least three days. Trickily, the day you are transferred to the skilled nursing facility does not count, and even more tricky is how CMS defines inpatient care.
These days you can stay overnight in the hospital, but that does not mean you are an inpatient. Thanks to legislation put forth in October 2013, known as the Two-Midnight Rule, you may only be considered for inpatient care if your stay is expected to last longer than two midnights and if your level of care is considered medically necessary. That means you cannot be in the hospital receiving care that could just as easily be administered elsewhere.
Otherwise, you will be placed under observation, care that is covered by Medicare Part B.
In the case that you do get approval for skilled nursing care, Medicare Part A covers the first 20 days for you. For days 21 to 100, you will pay $194.50 per day as of 2022. After 100 days, you are on your own.
How Much Does A Nursing Home Cost
Nursing home costs can vary depending on these factors:
- Location: Costs are different in each state, ranging from $180/day in some southern states to over $1,000/day in parts of Alaska. The nationwide average daily cost of a shared room is $260/day.
- Private or shared room: Private rooms are more expensive and are not subsidized by Medicaid. Medicare will not pay for a private room even if you qualify for Medicare skilled care.
- Services required: Some nursing home rates are all-inclusive and some charge additional fees for things like physical or speech therapy or memory care.
- Low-come subsidy vs. private pay: If you pay privately, your daily rate is higher than what Medicaid pays. If you meet Medicaid income and resource limits, Medicaid will pay the nursing home. Limits vary by state, but on average your assets must be valued at less than $2,000 and your monthly income must be less than $2,523 .
- Medicare-covered: If you are eligible for skilled care after a qualifying hospital stay, Medicare will pay 100% of nursing home costs for the first 20 days and 80% for days 21 100. Medicare will not cover any costs after that.
Items And Services Covered By Medicare:
- a semi-private room, unless a private room is medically necessary
- meals
- Personal items such as razors, toothpaste, and other personal hygiene items
There are some additional rules about Medicare coverage that you should know, including:
- Your doctor can request additional services on your behalf that arent typically covered by Medicare.
- If you leave the skilled nursing facility and need to return within 30 days, you can do so without starting a new benefit period.
- Medicare coverage will not pay for long-term care. Long-term care can include custodial care, which is when you need help with your daily activities but dont need a medical professional, and assisted living, which is a residential setting that sometimes offers medical care as well.
Don’t Miss: How Does Medicare For All Work
Does The Medicare Pace Program Cover Nursing Homes
PACEprovides in-home care services that are similar to whats offered in a nursinghome. PACE may not be available in your area, and you have to meet specificincome requirements to qualify. Your costs for PACE services will vary based onyour income, so you should consult with PACE directly to determine what you maybe responsible for.
Ultimately, if you or a loved one may need long-term care at a nursing home or assisted living services in the future, you shouldnt rely on Medicare coverage to pay for them. You may want to review your options for a long-term care insurance policy, as theyre designed to cover these costs.
Nothing on this website should ever be used as a substitute for professional medical advice. You should always consult with your medical provider regarding diagnosis or treatment for a health condition, including decisions about the correct medication for your condition, as well as prior to undertaking any specific exercise or dietary routine.
How Much Will Medicare Cover
Medicares coverage for skilled nursing facilities is broken down into benefit periods. A benefit period begins the day you are admitted as an inpatient to the hospital or skilled nursing facility.
Different amounts are paid throughout the benefit period. The benefit period ends when 60 days in a row have passed without a need for hospital or skilled nursing care. If you go back to the hospital after that 60-day window, a new benefit period begins.
Here are the costs that apply throughout the benefit period:
- Days 1 through 20: Medicare covers the entire cost of your care for the first 20 days. You will pay nothing.
- Days 21 through 100: Medicare covers the majority of the cost, but you will owe a daily copayment. In 2020, this copayment is $176 per day.
- Day 100 and on: Medicare does not cover skilled nursing facility costs beyond day 100. At this point, you are responsible for the entire cost of care.
While you are in a skilled nursing facility, there are some exceptions on what is covered, even within the first 20-day window.
Also Check: Where To Get Medicare Information
What Nursing Home Services Does Medicare Cover
Medicare-covered nursing home services must be provided by, or under the supervision of, skilled professionals or technical staff. Nursing home personnel manage your care, evaluate your progress, and document the results of your treatment. Nursing home services must be ordered by your physician. Covered services include:
- Semi-private room, which is a room you share with other patients
- Meals
- Services that are not deemed medically necessary or are not on your physician-ordered plan of care
- A private room, unless your doctor says it is necessary for your condition
- Ambulance transportation if you can safely be transported another way
- Care provided at a facility that is not Medicare-certified
What Skilled Nursing Facility Costs Does Medicare Cover
Medicare can cover many of the services you receive in a skilled nursing facility, such as:
- A semiprivate room and meals
- Skilled nursing care
- Medical social services and dietary counseling
- Medications, medical equipment and supplies used in the facility
- Occupational therapy, physical therapy or speech and language pathology services if needed to meet your health goal
- Ambulance transportation if needed to receive necessary services that arent available in the facility
Also Check: How To Get Medical Equipment Through Medicare
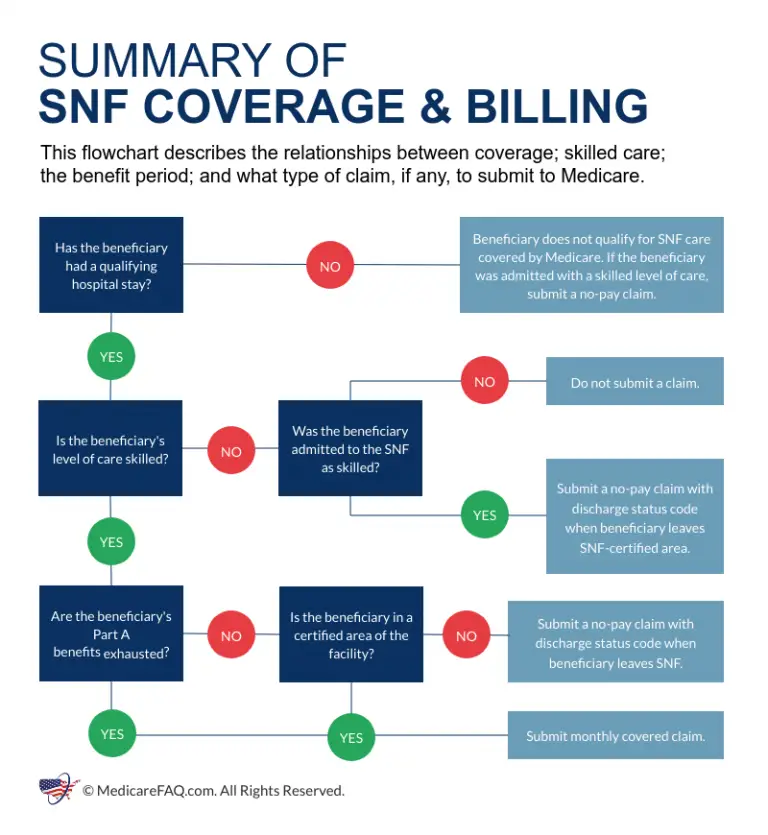
Medicare Coverage Requirements For Skilled Nursing Facility Care
SNF care is nursing and therapy that can only be performed or supervised by professionals or technical personnel. Medicare Part A may help cover SNF care in certain conditions for a limited time if all of these conditions are met:11
- You have Part A and have days left to use in your Medicare
- You have a qualifying hospital stay
- Your doctor decided that you need daily skilled care
- The SNF where you get skilled services is certified by Medicare
- You need these skilled services for a medical condition thats either:
- A hospital-related medical condition treated during your qualifying 3-day inpatient hospital stay, even if it wasn’t the reason you were admitted to the hospital
- A condition that started while receiving care in the SNF for a hospital-related medical condition
How Do I Qualify For Wound Care Benefits
To receive benefits from Medicare, you must be enrolled in original Medicare , or you must be enrolled in a Part C/Medicare Advantage plan. For wound care supplies and care to be covered, you will first need to meet your annual deductible and then pay any applicable copays or premiums due.
Before you begin treatment, its a good idea to verify that your doctor is an enrolled Medicare provider. Your doctor will have to provide a signed, dated order for the wound care supplies you need, clearly stating:
- the size of your wound
- the type of dressing needed
- the size of dressing needed
- how often your dressing needs to be changed
- how long you are likely to need the dressing
Also Check: Do I Have To Have Part D Medicare
What Is A Skilled Nursing Facility
Skilled care is nursing or therapy services that must be performed by or supervised by a professional. This may include wound care, physical therapy, giving IV medication, and more.
Skilled nursing facilities can be located within hospital units, but these are the minority. Most skilled nursing facilities are stand-alone, private, for-profit businesses. They usually provide many types of services, such as short-term medical care, rehabilitation, and long-term care.
Tip
Medicare offers an online tool to help you find approved skilled nursing facilities. Case managers and social workers can also help you with coverage for your hospital or skilled nursing facility stay.
Paying For Skilled Nursing Facility Care
There are several programs that may help you cover your out-of-pocket costs for skilled nursing care. You can call your state Medicaid office for more information about these programs and whether they are right for you.
State Medicare Savings Programs can help pay premiums, deductibles, copayments and prescription drug costs if you meet certain conditions. You must have limited resources in checking or savings accounts, stocks and bonds to qualify.
Medicaid is a joint state and federal program that helps with medical costs for some people who have limited income and financial resources. It may offer benefits for services not covered by Medicare.
In some cases, PACE, or Program of All-inclusive Care for the Elderly, may be an alternative if the services you require can be performed in the home, community or a local PACE center.
PACE is a joint Medicare and Medicaid program that helps people meet health care needs in their community instead of going into a nursing home or other care facility. You may be required to use a PACE-preferred doctor when you enroll.
Also Check: Does Medicare Pay For Hip Replacement Surgery
Exceptions To Medicare 3 Day Hosptial Stay Rule
If the patients health conditions are not appropriate for placing into a nursing facility directly after leaving the hospital, the hospital will determine when to begin appropriate care. Another exception to this rule is if the patient requires around the clock nursing services.
Get A Free Quote
Find the most affordable Medicare Plan in your area
When Does Medicare Cover Nursing Home Care

Medicare will not usually cover services that help with everyday life functions, such as assistance with dressing, eating or going to the bathroom.1 Generally, if the care you receive in a nursing home does not require a degree to provide, Medicare wont cover it.2 However, Medicare Part A may provide coverage for skilled nursing facility care thats medically necessary .3
Note: If you have a Medicare Advantage plan , contact your insurance carrier. You may have extra benefits for vision, hearing and dental that Original Medicare doesnt cover.4
Read Also: Is Breo Covered By Medicare
When Does Medicare Cover Wound Care
Medicare Part A covers medical care you receive in an inpatient facility like a hospital, inpatient rehab facility, or skilled nursing facility.
Medicare Part B covers any outpatient wound care you receive from either your healthcare provider or skilled nursing care facility. Part B covers both the cost of your treatment and any medically necessary supplies your healthcare provider uses to care for your wounds.
Medicare Part C, also known as Medicare Advantage, is a health insurance plan that provides the same basic coverage as Medicare parts A and B but usually with additional benefits. Talk to your Medicare Advantage insurer for details of your plans wound care coverage.
Medigap, or supplemental insurance, is a private insurance plan that helps cover your part of Medicare costs. This kind of plan will help you pay for any additional out-of-pocket wound care costs after Medicare pays its portion.
keep in mind
If your doctor recommends a newer type of wound care therapy, like stem cell treatments for example, verify first that Medicare will pay for the therapy. If its not an approved therapy, you will be responsible for the full cost, which can be expensive.
The following types of supplies are generally covered, when prescribed or provided by a healthcare provider:
Primary dressings :
- sterile gauze pads
Do All Nursing Homes Accept Medicaid
A majority of nursing homes accept Medicaid however, this is also largely dependent on the state you reside in. To avoid complications with payment and coverage, Id recommend checking with your nursing home facility to see if they are a Medicaid-certified nursing facility. If it is, then you should be eligible for coverage under the Medicaid skilled nursing facility.
In the event that you find out the nursing home is not Medicaid-certified, you would have to transfer to a nursing facility thats covered by Medicaid.
Also Check: Is Obamacare Medicare Or Medicaid
What Is Palliative Care
When someone receives a diagnosis of a life threatening illness, they may need palliative care.
Palliative care doctors and nurses provide treatments that relieve the symptoms of a health condition and improve a persons quality of life. They may provide care in the individuals home, a hospital, a nursing home, or a palliative care clinic.
Various conditions may lead to the need for palliative care, including:
This type of care involves helping improve the physical, mental, and emotional quality of a persons life. The exact care that someone receives will depend on their individual needs.
Physical support typically involves pain relief for symptoms and in completing everyday tasks that the person may have difficulty with, such as personal care and hygiene.
Palliative care professionals can also provide practical help, such as helping a person navigate treatment options or helping them work out their finances.
Mental healthcare provides support for the persons emotional and spiritual needs.
Palliative care and hospice care are related forms of support. If someone receives a diagnosis of a terminal illness and a doctor does not believe that they will survive for longer than 6 months, they may choose hospice care.
Hospice care provides the best possible quality of life for someone in their final months of life.
The different parts of Medicare cover inpatient care, outpatient care, mental health support, and necessary prescription drugs.
Legislative History And Benefit Trends
The ensuing discussion is based on the data for the aged shown in Table 2. During the period from 1967 through 1969, the use of SNF services far exceeded the level projected by actuaries during the development of the Medicare legislation . Actuarial projections for 1967, the first year that the benefit would be available, estimated total Medicare payment for SNF services at about $30 million. Instead, SNF payments in 1967 were $313 million, ten times the projection. In 1968, SNF payments rose to $402 million. It was apparent that the SNF benefit was being misinterpreted to provide long-term nursing home care beyond the scope intended by the legislation. In April 1969, the Bureau of Health Insurance2 issued Intermediary Letter No. 371, Determining coverage of care in an extended care facility . This intermediary letter re-emphasized the legislative intent of the SNF benefit as previously described and, to promote uniformity among intermediaries in making coverage determinations, provided a list of services that would be covered.
The effects of the letter were immediate. All measures of SNF benefit utilization and program payments decreased significantly. In 1970, the days of SNF care used were one-half of that in 1968. Reimbursements dropped from $402 million in 1968 to $245 million in 1970. The SNF share of total Medicare program payments was cut in half, from 6.8 percent in 1968 to 3.4 percent in 1970.
You May Like: Is Stem Cell Treatment Covered By Medicare
Day Hosptial Stay Rule With Medicare Billing For Coverage In Skilled Nursing Facilities
For a beneficiary to extend healthcare services through SNFs, the patients must undergo the 3-day rule before admission. The 3-day rule ensures that the beneficiary has a medically necessary stay of 3 consecutive days as an inpatient in a hospital facility. This doesnt include the day of the patients discharge, any outpatient observations, or the time spent in the emergency room.
Stopping Care Or Leaving
If you stop getting skilled care in the SNF, or leave the SNF altogether, your SNF coverage may be affected depending on how long your break in SNF care lasts.
If your break in skilled care lasts more than 30 days, you need a new 3-day hospital stay to qualify for additional SNF care. The new hospital stay doesnt need to be for the same condition that you were treated for during your previous stay.
If your break in skilled care lasts for at least 60 days in a row, this ends your current benefit period and renews your SNF benefits. This means that the maximum coverage available would be up to 100 days of SNF benefits.
Don’t Miss: How Soon Can I Sign Up For Medicare
Medicare Part A Covers
- Certain care in a skilled nursing facility
- Certain home health services
- Certain hospice care
You will not pay a Part A monthly premium if you are eligible for Social Security retirement benefits or Railroad Retirement benefits. If you have 30-39 quarters of Social Security credits, you may buy Part A coverage and pay a monthly premium of $274 in 2022. If you have 0-29 quarters of Social Security credits, you may buy Part A coverage and pay a monthly premium of $499 in 2022.
