What Is Tens Therapy
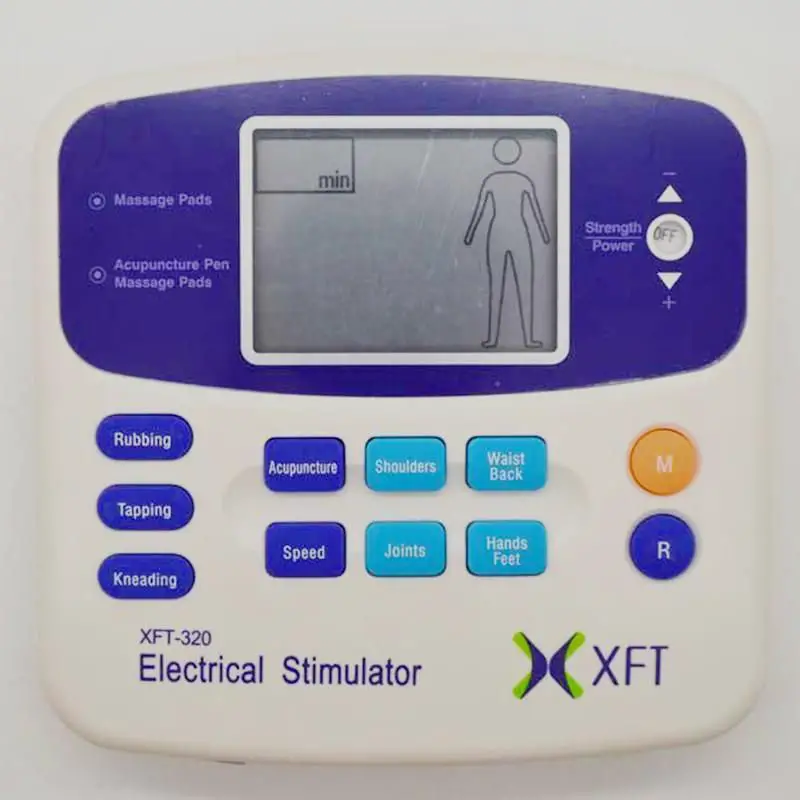
TENS involves delivering a weak electrical current via electrodes to the skins surface near the origin of pain. The electrical current passing through the electrodes stimulates the nerves in the treatment area. This electrical stimulation causes the nerves to go haywire. Instead of sending normal pain signals to the brain, they send undecipherable signals. The brain cannot interpret the signals, thus reducing pain depending on its severity.Although TENS is often mis-conceptualized as a painful process, most likely due to the use of electricity, the application is painless. Despite its sophisticated name, transcutaneous electrical nerve stimulation is a simple application that can be implemented at home using a TENS unit a battery-powered mobile device.
Can A Tens Unit Reduce Belly Fat
Surprisingly, without modifying their exercise or diet, the EMS did indeed cause significant effects on decreasing waist circumference, abdominal obesity, subcutaneous fat mass, and body fat percentage, leading the researchers to conclude: The use of the high-frequency current therapy may be beneficial for reducing Feb 6, 2019.
You May Like: What States Have Medicare Advantage Plans
What Is Functional Electrical Stimulation
Functional electrical stimulation . This device targets certain types of paralyzed muscles to help regain limited use of those muscles in patients who have suffered a back injury, stroke or other neurological injuries. Certain types of e-stim devices are better for some conditions than others. Your doctor or physical therapist can help you …
Don’t Miss: Does Kaiser Permanente Accept Medicare And Medicaid
Does Medicare Cover Tens Units For E
There are many conditions that may require e-stim therapy, which requires the use of a TENS unit. If your doctor is using a broader approach that incorporates the use of your device as part of a larger treatment plan, you’re more likely to be approved for coverage. Medicare Advantage plans vary and may have different requirements for coverage but are generally more accepting of TENS unit therapy.
Transcutaneous Electrical Joint Stimulation And Pulsed Electrical Stimulation

Transcutaneous electrical joint stimulation is also known as pulsed electrical stimulation and the Bionicare device uses this type of electrical stimulation. Zizic et al evaluated the safety and effectiveness of pulsed electrical stimulation for the treatment of osteoarthritis of the knee . Patients were treated 6 hours/day for 4 weeks. The investigators reported that patients treated with the active devices showed significantly greater improvement than the placebo group for all primary efficacy variables in comparisons of mean change from baseline to the end of treatment. Improvement of greater or equal to 50 % from baseline was shown in at least 1 primary efficacy variable in 50 % of the active device group, in 2 variables in 32 %, and in all 3 variables in 24 %. In the placebo group improvement of greater or equal to 50 % occurred in 36 % for one, 6 % for 2, and 6 % for 3 variables. Mean morning stiffness decreased 20 mins in the active device group and increased 2 mins in the placebo group . No statistically significant differences were observed for tenderness, swelling, or walking time. The authors concluded that improvements in clinical measures for pain and function found in this study suggest that pulsed electrical stimulation is effective for treating OA of the knee. The investigators noted, however, that studies of the durability of results are warranted.
Don’t Miss: What Is Gap Coverage For Medicare
Are Tens Units Available For Purchase
Patients do have the option to purchase their own TENS unit, and doing so does not require a prescription from a doctor. While the devices themselves are affordable, you will have to continue to purchase additional electrodes, which can drive the cost up if used frequently. And if the TENS unit malfunctions, the patient will be forced to purchase a new unit. In contrast, if insurance covers the cost of the unit, the policy should provide a new model.
Used And Refurbished Dme And P& O
Supply providers have the option to request used and/or refurbished DME and P& O. Equipment may be donated, passed down from a sibling, or purchased from a DMEPOS provider post refurbishment. Used equipment also includes equipment that has not been previously rented or sold . All used and refurbished equipment requires a PAR.
The DMEPOS provider must guarantee that the equipment provided to the member is in like new condition, and that any modifications are made prior to the delivery of the equipment. The cost of repairs or modifications must not exceed the cost of replacement equipment. The provider will maintain a one year limited warranty that covers all necessary parts or repairs. Comparison pricing for new equipment must be included in the PAR documentation. PAR documentation must include the make, model, and serial number of equipment. The Used Equipment modifier must be included on all used and refurbished equipment PARs and claims.
Examples of allowable used or refurbished equipment include but are not limited to:
- Manual Wheelchairs
- Speech Generating Devices
If new equipment is rented to and subsequently purchased by the same member, it would not be considered used. Supplies may not be provided as used.
Unless a part of the Upper Payment Limit, the maximum allowable for used/refurbished equipment is 60% of the equipments maximum allowable for purchase.
Recommended Reading: How To Apply For Medicare Advantage
Tens For Musculoskeletal Pain In Hemophilia
As for pharmacologic management, NSAIDs are better than paracetamol. The advantages of tramadol or tramadol/paracetamol and non-tramadol opioids are scanty. With respect to physical medicine and rehabilitation, there is insufficient confirmation that a brace has supplementary favorable effect compared with isolated pharmacologic management. Land-based curative exercise and watery exercise have at the minimum a tiny short-run benefit. Curative ultrasound can be helpful . The effectiveness of TENS for pain mitigation has not been proven. Electrical stimulation treatment can procure notable ameliorations. With respect to intra-articular injections, viscosupplementation appears to be a useful method for pain alleviation in the short-run . The short-run advantage of intra-articular corticosteroids in the treatment of joint pain has been shown.
A Commode Is Covered When The Patient Is Incapable Of Utilizing Regular Toilet Facilities
Coverage and Payment Policy
A commode is covered when the beneficiary is physically incapable of utilizing regular toilet facilities. This would occur in the following situations:
An extra wide/heavy duty commode chair is covered for a beneficiary who weighs 300 pounds or more.
A commode chair with detachable arms is covered if the detachable arms feature is necessary to facilitate transferring the beneficiary or if the beneficiary has a body configuration that requires extra width.
Commode chair with seat lift mechanism is covered if the beneficiary has medical necessity for a commode and meets the coverage criteria for a seat lift mechanism.
Duplicate devices for multiple bathrooms are not covered.
Click here for an approved PDF version of the Commode coverage guidelines.
Compression Garment
A compression garment is a custom made or custom fitted support garment fabricated to apply varying degrees of pressure to specific anatomic areas. These garments affect stress on vein walls, muscle pump activity, tissue pressure and circulation. These garments are also used in the treatment of burn patients. The majority of applications do not require custom made garments.
You May Like: Does Missouri Medicaid Cover Assisted Living
Read Also: Does Medicare Require A Referral For A Colonoscopy
Types Of Dme Not Covered By Medicare
Not all types of DME are covered by Medicare. If a device is designed for use outside the home, its likely you cant cover it through Medicare. Also, if a piece of equipment is for convenience or comfort, Medicare typically does not cover it.
Items not covered by Medicare may include:3
- Modifications to the home, such as ramps
- Most disposable or single-use items
- Stair elevators
Peripheral Subcutaneous Field Stimulation
Subcutaneous stimulation is a novel neuromodulation modality that has increased in its utilization during the past decade. It consists of introducing a lead in the subdermal level to stimulate the small nerve fibers in that layer. Unlike other neuromodulation techniques including direct peripheral nerve stimulation, spinal cord stimulation , or deep brain stimulation, the precise target is not identified. Falco et al stated that relief of regional, non-appendicular pain, particularly LBP, through SCS has proven challenging. Recently, peripheral nerve stimulation , also known as PNFS depending on the stimulation area, has demonstrated efficacy for the treatment of well-localized, small areas of pain involving the abdomen, inguinal region, pelvis, face, occipital area, and low back. More widespread application of PNFS has been limited by its narrow field of coverage in a larger group of patients with diffuse or poorly localized pain.
Don’t Miss: Does Medicare Cover Cataract Surgery And Implants
Tens For Peripheral Arterial Disease
Measures taken were initial claudication distance, functional claudication distance and absolute claudication distance. The McGill Pain Questionnaire vocabulary was completed at the end of the intervention and the MPQ-Pain Rating Index score was calculated. Four participants were excluded from the final analysis because of non-completion of the experimental procedure. Median walking distance increased with high-frequency TENS for all measures . Only absolute claudication distance increased significantly with low-frequency TENS compared with placebo . No difference was observed between reported median MPQ-Pain Rating Index scores: 21.5 with placebo TENS and 21.5 with active TENS . The authors concluded that TENS applied to the lower limb of the patients with PAD and IC was associated with increased walking distance on a treadmill but not with any reduction in pain. They stated that TENS may be a useful adjunctive intervention to help increase walking performance in patients with IC.
Will A Tens Unit Help A Herniated Disc
TENS will treat many different types of back pain including sciatica from a herniated disk, multiple disk herniations, muscle strains, muscle contusions, stiff neck from reading or staring at a laptop and other maladies. If you are suffering from back pain, consider using TENS as a treatment and therapy option.
Recommended Reading: Does Medicare Pay For Telehealth
Frequency Specific Microcurrent Therapy For The Treatment Of Back And Neck Pain
Furthermore, UpToDate reviews on Management of non-radicular neck pain in adults , Subacute and chronic low back pain: Nonpharmacologic and pharmacologic treatment , Subacute and chronic low back pain: Nonsurgical interventional treatment , and Treatment of acute low back pain do not mention frequency specific microcurrent as a management / therapeutic option.
American Hospital Association Disclaimer
The American Hospital Association has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
Also Check: Does My Doctor Accept Medicare Advantage
Does Unitedhealthcare Community Plan Cover Breast Reduction
Coverage Limitations and Exclusions UnitedHealthcare excludes Cosmetic Procedures from coverage including but not limited to the following: Breast reduction surgery when done to improve appearance without improving a functional/physiologic impairment. Liposuction as the sole procedure for breast reduction surgery.
Read Also: Does Medicare Have A Cap
Scrambler Therapy For Neuropathic Pain Associated With Chemotherapy
Tomasello and colleagues noted that chemotherapy-induced peripheral neuropathy is a common side effect of chemotherapy in need of effective treatment. Preliminary data supported the efficacy of scrambler therapy , a non-invasive cutaneous electrostimulation device, in adults with CIPN. These researchers examined the safety, efficacy, and durability of ST for neuropathic pain in adolescents with CIPN. They studied 9 pediatric patients with cancer and CIPN who received ST for pain control. Each patient received 45-min daily sessions for 10 consecutive days as a first step, but some of them required additional treatment. Pain significantly improved comparing NRS after 10 days of ST and at the end of the optimized cycle . The improvement in QOL was significantly reached on pain interference with general activity , mood , walking ability , sleep , and relations with people . The authors concluded that based on these preliminary data, ST could be a good choice for adolescents with CIPN for whom pain control is difficult ST caused total relief or dramatic reduction in CIPN pain and an improvement in QOL, durable in follow-up. It resulted in no detected side effects, and could be re-trained successfully. Moreover, these researchers stated that further larger studies are needed to confirm these promising preliminary data in pediatric patients with cancer.
Don’t Miss: Does Medicare Cover Condom Catheters
Is Tens Covered By Medicare
What is TENS Unit?A TENS unit is a little, battery-powered gadget that sends out electrical impulses to specific nerve paths in order to assist with discomfort relief. Is Tens Covered By MedicareThe Tens Unit can be used by itself or in combination with other treatment methods such as cold treatment, heat treatment, or medication. There are numerous situations in which a tens unit can be helpful:
Arthritis Elbow discomfort .The gadget releases a little electrical existing that stimulates the nerve endings on the skin.Ive been utilizing this product for about a month, therefore far Im really happy. I was trying to find something that could do more as far as various therapies. Some brand names dont have an EMS mode just TENS.
A professional massage therapist reported he used the Tens unit on his clients in addition to for himself for individual use. It helps him relax, de-stress, and lowers discomfort levels. This product is clean, lightweight, easy to use, and works well! I would suggest this item to anybody who wants remedy for discomfort or simply wants to relax & unwind from a long stressful day at work.
Medicare Part C Costs
Costs under a Medicare Part C plan will be different and will depend on which plan you have and how much coverage youve chosen. The coverage you have under a Part C plan must be at least equal to what original Medicare covers.
Some forms of outpatient pain management are also covered under Medicare Part B. This includes things like:
- medication management
- manipulation of the spine, if medically necessary
- outpatient injections
- transcutaneous electrical nerve stimulation for pain after a surgical procedure
- autogenous epidural blood graft for headaches after an epidural or spinal tap
Dont Miss: Is Stelara Covered By Medicare Part B
Recommended Reading: Who Can I Call About Medicare Questions
Let Insurance Cover It
Chronic pain is a condition that affects millions of people across the globe. And while there is no cure-all for chronic pain, there are treatments that help reduce its symptoms, such as over-the-counter medications, surgery, and TENS therapy. Transcutaneous electrical nerve stimulation works by scrambling the signals from the nerves to the brain, which temporarily eliminates pain in the treated area. There is some skepticism by researchers regarding the effectiveness of TENS therapy. Still, many patients find that its the only treatment that offers a respite from chronic pain.The convenience of TENS therapy makes it particularly appealing because it can be applied at home by using a mobile TENS unit. The costs can quickly add up if using electrodes every day, so its best to find an insurance provider that will cover the cost of the unit and the supplies. It may be an arduous process, but knowing how to get a TENS unit covered by insurance will go a long way in easing your pain.
Experimental And Investigational Indications

Also Check: Does Medicare Part A And Part B Cover Prescriptions
What Is Procedure Code E1399
HCPCS code E1399 describes durable medical equipment, miscellaneous and is currently being used to bill for inexpensive DME subject to the rules of 42 C.F.R. 414.220, other covered DME subject to the rules of 42 C.F.R. 414.229, and replacement parts of DME subject to the rules of 42 C.F.R. 414.210.
Tens For Chronic Low Back Pain
CMS issued a Medicare National Coverage Determination on June 8, 2012 that allows coverage of Transcutaneous Electrical Nerve Stimulation for chronic low back pain only when the patient is enrolled in an approved clinical study within three years after the publication of this decision under coverage with evidence development that meets the criteria outlined below. 1
The results of additional clinical research may potentially provide sufficient evidence to inform future NCDs on the topic. CMS will maintain a list of all approved studies and post that list on this website.
Recommended Reading: How Much Does Medicare Part C Cost Per Month
Cpt Codes Not Covered For Indications Listed In The Cpb :
63650 Percutaneous implantation of neurostimulator electrode array, epidural 63655 Laminectomy for implantation of neurostimulator electrodes, plate/paddle, epidural 63661 Removal of spinal neurostimulator electrode percutaneous array, including fluoroscopy, when performed 63662 Removal of spinal neurostimulator electrode plate/paddle placed via laminotomy or laminectomy, including fluoroscopy, when performed 63663 Revision including replacement, when performed, of spinal neurostimulator electrode percutaneous array, including fluoroscopy, when performed 63664 Revision including replacement, when performed, of spinal neurostimulator electrode plate/paddle placed via laminotomy or laminectomy, including fluoroscopy, when performed 63685 Insertion or replacement of spinal neurostimulator pulse generator or receiver, direct or inductive coupling 63688 Revision or removal of implanted spinal neurostimulator pulse generator or receiver