Pdf: Documentation Requirements For Catheters
In order to cover sterile catheters and lubrication, Medicare requires proper documentation in the prescribing doctors notes. These notes, which are referred to as PDF, must also match the plan of care/prescription.
PDF stands for the permanence of the condition, the diagnosis, and the frequency of cathing per day or per week, etc.
Permanence
The doctors notes must indicate that the need for catheters is a chronic or permanent condition. If the medical record indicates the condition is of long-term or indefinite duration , this meets the measure of permanence.
Diagnosis
Frequency
Documentation must also show the recommended number of times the patient should catheterize per day . Also, this must match the prescribed frequency listed on the Plan of Care.
Additional Doctors Progress Notes
Any additional notes in the records may be helpful for approval.
Notes may include:
Is It Possible To Receive Over 200 Catheters Per Month With Medicare
Typically, if you self-catheterize between 6 and 7 times per day, 200 sterile catheters and lubricating jelly packets should be enough. However, if you run out of catheters or run low every month, its possible that you may qualify for more.
Usually, this frequent shortage is due to a unique medical condition or an above-average urine output.
If you feel you may qualify, keeping a cathing journal or a written schedule may help you and your doctor better understand your bodys urine production, typical output, and frequency of catheterizations.
You can download 180 Medicals handy Catheterization Diary here: 180 Medical Cathing Diary PDF.
In 2019, CGS for Medicare discontinued their prior guidelines to limit intermittent catheters to only 200 per month .
Nevertheless, its important to note that Medicare still requires proof in the form of medical documentation from a qualified healthcare practitioner.
Intermittent Urinary Catheters Through Medicare
Broadly, Medicare covers 200 intermittent single-use catheters each month . This also includes closed-system catheters, or catheters with sterile insertion supplies.
200 catheters per month allows for the catheter user to change their catheter at least 6 times a day with additional catheters leftover, should any difficulties with insertion arise.
One of the greatest barriers to regular catheter use is the discomfort of insertion. For this reason, we recommend a hydrophilic catheter through Medicare. Hydrophilic catheters decrease the possibility of failed insertions due to their sterile saline lubrication. They can also reduce the buildup of scar tissue from catheterization over time, which can be especially helpful for patients whose need to catheterize is lifelong or chronic. By eliminating difficulties to reliable and regular catheterization, individuals can experience an increase in the effectiveness of their treatment and their quality of life.
In order for Medicare to cover the coudé tip catheter, a medical need that inhibits the user from using a straight tip catheter must be demonstrated. This type of catheter can be especially beneficial for male patients with BPH , also known as an enlarged prostate.
Don’t Miss: How Long Do You Have To Sign Up For Medicare
Medicare Coverage For Catheters
Medicare requires a prescription and related doctors notes in order to cover catheter supplies. 180 Medical works with your healthcare providers office to get that documentation. Because integrity is one of our core values, well do what it takes to do the right thing and ensure total compliance with Medicares guidelines.
Questions about insurance? Let us help. by one of our catheter insurance specialists.
Does Private Insurance Pay For Catheters

Private insurance plans differ depending on your plan and the company. Its difficult to accurately quote your out-of-pocket cost without verifying your insurance. This is because each plan has varying annual deductibles and out-of-pocket limits. Also, most private insurance companies have different percentages paid toward your disposable incontinence supplies after your deductible has been met.
The good news is that many private insurance plans cover advanced catheter products. For example, you could receive closed system catheters, ready-to-use travel catheters, or hydrophilic catheters. It mainly depends on the company and your specific plans coverage.
Well be more than happy to verify your insurance for you and discuss your plan in depth. We want you to fully understand your insurances catheter coverage and available product options.
Read Also: How Can I Enroll In Medicare Part D
Does Medicare Cover Incontinence Surgery
Original Medicare and Medicare Advantage plans cover certain surgical procedures and implantable medical devices that can help control incontinence
Examples of Incontinence Surgical Procedures Medicare Covers
- Urethroplasty
- Medicare covers urethroplasty a surgical procedure that repairs an injury or defect within the walls of your urethra. But you are responsible for your Part B deductible and 20 percent of the remaining Medicare-approved cost of the surgery. Medicare estimates your average out-of-pocket costs at $610 in an ambulatory surgical center and $1,080 in a hospital outpatient department.
- Transurethral radiofrequency micro-remodeling
- Medicare will help pay for this procedure to treat urinary stress incontinence in women. It uses energy from radio frequencies to shrink and stabilize tissue in your body to support your urethra and bladder neck.
You are responsible for your Medicare Part B deductible and a 20 percent coinsurance payment based on the Medicare-approved cost for the procedure. Medicare estimates your average out-of-pocket costs at $204 in an ambulatory surgical center and $403 in a hospital outpatient department.
Medicare may help pay for other incontinence surgical procedures. Talk with your doctor about Medicare coverage for any surgeries recommended for you.
You can also call Medicare at 1-800-633-4227 to ask if a procedure is covered. If you have a Medicare Advantage plan, contact your plans administrator.
How To Reimburse Intermittent Catheters With Insurance
There are two main ways to get your intermittent catheters reimbursedthrough Medicare or private insurance. Insurance coverage of catheters and supplies varies with each persons plan, whether private or government-sponsored. To get reimbursement, doctors must provide a prescription since catheters are not sold over-the-counter or for self-diagnosis and self-treatment purposes.
Recommended Reading: Is Medical Part Of Medicare
How Many Catheters Will My Insurance Cover
In order to buy catheters, whether with or without insurance, you must have a prescription from a healthcare professional. All insurance plans will require a prescription at a minimum, but many plans also require additional documentation.
For example, Medicare requires a prescription and additional documentation in your doctors notes to show how many catheters you will need within a 30 day period. Medicare will cover up to 200 single-use catheters per month. This is enough to self-cath sterilely between 6 and 7 times a day within a 30 day period. The amount you can receive up to this limit will entirely depend on your prescription.
However, each insurance plan is different, so the limits on how many sterile-use catheters they allow may vary.
Concerned about having to do the footwork to gather a prescription or documentation for your medical supply provider? 180 Medical takes care of everything for you, including communicating with your doctors office to obtain any information your insurance requires.
Where Can I Get Insurance
180 Medical is one of the largest and highly-rated catheter suppliers in the nation. Were contracted with over 1,200 insurance plans, including Medicare, state Medicaids, and a growing number of private insurance plans. Our specialists are glad to help you find an insurance-covered catheter to fit your needs.
First, well verify your insurance policy. Next, well call you back and inform you fully about how your catheter supplies will be covered. Additionally, before we ship your first order, we make sure to let you know about any potential out-of-pocket costs based on your insurance coverage.
Also Check: How Much Do Medicare Plans Cost
License For Use Of Physicians Current Procedural Terminology Fourth Edition
End User Point and Click Amendment:CPT codes, descriptions and other data only are copyright 2020 American Medical Association. American Medical Association. All Rights Reserved . CPT is a trademark of the American Medical Association .
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services . You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, AMA Plaza, 330 Wabash Ave., Suite 39300, Chicago, IL 60611-5885. Applications are available at the AMA Web site, .
Why Would I Need A Urinary Catheter
According to the U.S. National Library of Medicine, a doctor may recommend a urinary catheter for certain medical conditions such as:
- Being unable to control when you urinate
- Being unable to empty your bladder when you need to
- Surgery on the prostate or genitals
- Medical conditions such as multiple sclerosis, spinal cord injury, or dementia
Keep in mind that urinary catheters may have many complications, such as urinary tract infections, bladder cancer, bladder stones and kidney damage. Intermittent catheterization is preferable to long-term catheterization, according the American Family Physician.
To prevent infection, you should drink plenty of fluids and clean the area where an indwelling urinary catheter exits your body every day, according to the U.S. National Library of Medicine.
Recommended Reading: Can I Get Medicare If I Have Cancer
Do You Have More Questions About Medicare Coverage
Im here to help you with your Medicare questions and coverage needs.
- You are welcome to call or email by clicking one of the buttons below.
- To research additional Medicare plan options, click the button that says, Compare Plans Now.
New To Medicare?
Becoming eligible for Medicare can be daunting. But don’t worry, we’re here to help you understand Medicare in 15 minutes or less.
Medicare Might Cover It
One of the absolute best things about condom catheters is that Medicare could cover the cost. While Medicare does not cover absorbent incontinence supplies, it does cover urology supplies, which is the category that condom catheters are a part of. This means you could potentially use your Medicare benefits to cover the cost. to learn more.
Note: Dont forget that . If you have Medicaid, contact us to see if you could get your supplies as a covered benefit.
Recommended Reading: Do You Need Medicare If You Are Still Working
Does Medicare Cover Catheters
Home / FAQs / Medicare Coverage / Does Medicare Cover Catheters
Medicare covers catheters and related medical supplies that a doctor says is medically necessary. Coverage depends on the type of catheter and the medical reason for it. The type of facility may also determine what benefits are available. Benefits also include catheter supplies like irrigation kits, bedside drain bags, leg bags, irrigation syringes, and extension tubing.
Getting Catheters Reimbursed Through Medicare
Medicare benefits under Medicare or a Medicare Advantage plan may cover intermittent catheters under specific circumstances, such as having underlying diseases or conditions. Medicare Part A is the coverage for inpatient hospital services and may cover the cost of catheters used when you are officially admitted into a Medicare-approved hospital. Medicare Part B covers outpatient care, home healthcare, doctors services, and durable medical equipmentintermittent catheters are considered durable medical equipment.
Recipients of Medicare who require catheters as part of their permanent medical conditions usually have catheters and supplies covered as prosthetics.
Recipients who have purchased a Medigap may have additional coverage for out-of-pocket expenses, such as coinsurance, copayments, or deductibles.
Medicare pays only for services that they deem medically necessary. The criteria for medical necessity are:
- Appropriate and needed for diagnosis, or treatment of your medical condition.
- Are provided for direct care and treatment of your medical condition.
- Meet the standard of care in the medical community
- Not primarily for the convenience of you or your doctor.
Recommended Reading: When Is Medicare Supplement Open Enrollment
Medicaid Coverage For Catheters
180 Medical is in-network with most state Medicaid programs. Coverage and allowable amounts on catheters and related supplies vary according to each states guidelines. Just contact us to find out what your states plan covers.
No matter what your particular Medicaid plan requires in order to cover catheters, well work diligently to obtain documentation and/or authorization for you.
Private Insurance Coverage For Catheters
We accept a wide variety of private insurance plans, and that number is growing all the time. Curious if we accept your particular insurance plan? Just give us a call or contact us online. Well verify your plans coverage for you, and after that, well discuss your catheter supply options with you.
Contact 180 Medical today to find out what your insurance plan covers. Youre just a call away from getting top-quality catheter supplies discreetly delivered to your home.
Read Also: Is Omnipod Covered By Medicare
Getting Catheters Reimbursed Through Medicaid
It will vary state by state because Medicaid is state-run, whereas Medicare is federally funded. It will likely be very close to the Medicare program and will require paperwork and doctors prescription. Eligibility is based on the level of income but you can be under the poverty level and still not qualify for the states program. If you do, you may also qualify for Social Security Income if you have permanent disabilities.
How Much Does A Catheter Cost With Medicare
Even if Medicare covers your catheter, there are some out-of-pocket costs you should expect to pay, which may include:
- Part A deductibleThe Medicare Part A deductible is $1,364 per benefit period in 2019.
You could potentially experience more than one benefit period in a given calendar year, since the Part A deductible is not based on an annual period.
- Part B deductibleMedicare Part B deductible in 2019 is $185 per year. You must meet the deductible before your Part B coverage kicks in.
- Part B coinsurance or copaymentOnce you meet your Part B deductible, you typically pay 20 percent of the Medicare-approved amount for most doctors services.There is no limit annually on how much you could pay for the Part B coinsurance in a specific year.
Talk to your doctor directly for specific cost and coverage information related to your catheter.
Also Check: How To Qualify For Extra Help With Medicare Part D
How To Get Help With Catheter Coverage With Medicare
Medigap plans will cover all or most out-of-pocket expenses for urinary catheters after Medicare pays their portion. Part B will cover 80% of the cost, and your Medigap plan will cover the remaining 20%. Without a supplemental plan, youll be responsible or 20% of the cost of the urinary catheter and supplies.
Give one of our licensed Medicare agents a call today at the number above. We can help you find an affordable supplement plan to help fill in the gaps in Medicare coverage. We can compare Medicare Supplements, Medicare Advantage, and Part D. If you cant call us, fill out an online rate comparison form to see all available policies in your area side by side now.
- Was this article helpful ?
Disclaimer: By clicking the button above, you consent to receive emails, text messages and/or phone calls via automated telephone dialing system or by artificial/pre-recorded message from representatives or licensed insurance agents of Elite Insurance Partners LLC, its affiliates or third-party partners at the email address and telephone number provided, including your wireless number , regarding Medicare Supplement Insurance, Medicare Advantage, Medicare Part D and/or other insurance plans. Your consent is not a condition of purchase and you may revoke your consent at any time. This program is subject to our Privacy Policy and Terms of Use. This website is not connected with the federal government or the federal Medicare program.
Condom Catheters In Maryland

Please visit specific items below. You can also contact Mary for further information at 301-774-8200 or Bethany in Towson at 410-882-4005. Prescriptions may be faxed directly to Mary at 301-774-5767. Thank-You for your Time and for Choosing our Company to provide you with excellent medical supplies and service!
Showing all 4 results
You May Like: Does Medicare Cover While Traveling Abroad
C Coverage For Purewick
Medicare Advantage plans also provide coverage for Purewick catheters. These plan have to cover everything Original Medicare covers. However, they will provide additional benefits as well. What additional benefits they provide and what the costs for these added benefits are will depend on what plan you have.
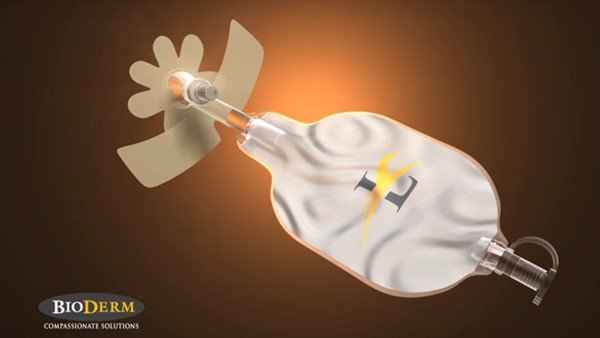
Purewick Urine Collection System
The PureWick system is a urine collection system that includes the PureWick female external catheter, a flexible, disposable “wick”, which is attached to a continuous low-pressure pump, the PureWick urine collection system. The system is designed to gently pull the urine from the external catheter into the sealed collection canister. The female external catheter works outside the body to absorb and wick urine. The wick is replaced every 8-12 hours or if its soiled with feces or blood.
There are no peer-reviewed published literature specific to the PureWick system, or external urinary collection system using a continuous low-pressure pump. Thus, there is no evidence to show the PureWick system to be as an equally effective alternative in managing urinary incontinence.
The revised July 2020 Noridian Medicare Local Coverage Determination for urological supplies does not include HCPCS code E0740 coverage details.
You May Like: Where Do I File For Medicare
Medicare Advantage Plans May Cover Catheters
Medicare Advantage plans are sold by private insurance companies and are required by law to cover everything that Part A and Part B cover.
If your catheter is covered by Original Medicare, it will also be covered by a Medicare Advantage plan.
Most Medicare Advantage plans offer prescription drug coverage. Some Medicare Advantage plans also offer additional benefits, such as:
