When Can Cms Add New Medicare Preventive Services
We may add preventive services coverage through the National Coverage Determination process if the service is:
- Reasonable and necessary for prevention or early detection of illness or disability
- United States Preventive Services Task Force recommended with grade A or B
- Appropriate for individuals entitled to Part A benefits or enrolled under Medicare Part B
We may also add preventive services through statutory and regulatory authority.
The USPSTF Published Recommendations webpage has more preventive services information.
We Can Help You Find The Best Medicare Plans For Cancer Patients
A Medicare Advantage plan is a great option if you are looking for additional benefits like genetic testing beyond BRCA 1 and 2 and myPath.
Some may even offer fitness classes like SilverSneakers®, which can help promote a healthy, physically active lifestyle and help lower your risk of cancer.
If youre diagnosed with cancer, you may be eligible for a type of MA plan called a Chronic Special Needs Plan . These plans are specially designed for people with certain chronic illnesses and conditions. Your C-SNP will involve a network of healthcare providers that will coordinate your treatment plan with each other.
If you are interested in arranging a no-cost, no-obligation appointment with a licensed agent to discuss your options for MA plans including C-SNPs, call us at 833-438-3676 or fill out this form.
This post was originally published on November 29, 2018, by Kelsey Davis and updated on March 24, 2020, by Troy Frink.
You May Like: Is Spaceoar Covered By Medicare
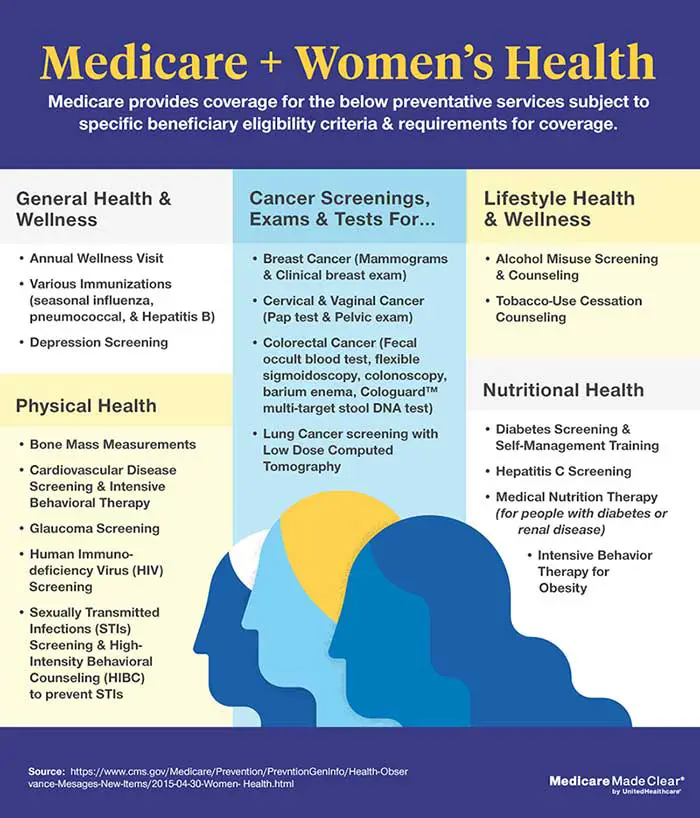
Cervical & Vaginal Cancer Screenings
Medicare Part B covers Pap tests and pelvic exams to check for cervical and vaginal cancers. As part of the pelvic exam, Medicare also covers a clinical breast exam to check for breast cancer. Medicare covers these screening tests once every 24 months in most cases. If youre at high risk for cervical or vaginal cancer, or if youre of child-bearing age and had an abnormal Pap test in the past 36 months, Medicare covers these screening tests once every 12 months.
Part B also covers Human Papillomavirus tests once every 5 years if youre age 30-65 without HPV symptoms.
If your doctor or other qualified health care provider accepts assignment, you pay nothing for the following:
- the lab Pap test
- the lab HPV with Pap test
- the Pap test specimen collection
- the pelvic and breast exams
You May Like: Does Medicare A& b Cover Dental
Does Medicare Cover Skin Cancer Treatment
If you are found to have skin cancer, Medicare will cover skin cancer treatment through various parts of the program. If a cancerous growth needs to be removed surgically, Medicare Part B will pay for the procedure as long as it takes place in an outpatient setting.
Any treatment administered while you are admitted to a hospital or skilled nursing facility will be covered by Medicare Part A, the inpatient benefit. If medications are prescribed for home use in the treatment of skin cancer, Medicare Part D may provide coverage for drugs listed in your plans formulary.
Hereditary Breast And Ovarian Cancer Genetic Testing
Hereditary breast and ovarian cancer associated with BRCA1 and BRCA2 mutations is the most common form of hereditary breast cancer. A 2015 population-based study of 396 African American women diagnosed with breast cancer before age 50 found that 12% of the study participants had BRCA1/2 mutations, more than double what was found in white women .
In 2005, the USPSTF recommended that women whose family history may be associated with an increased risk for deleterious BRCA1/2 mutations be referred for genetic counseling and evaluation for BRCA testing . Through time, the Centers for Medicare and Medicaid Services and other federal health agencies have issued clarifications broadening the criteria for coverage .
You May Like: Does Medicare Cover Eylea Injections
Will A Positive Genetic Test Result Make It Harder For Me To Get Health Insurance
Some people have worried that genetic testing for future health risks could affect their ability to get or keep their health insurance. Fortunately, a federal law called the Genetic Information and Nondiscrimination Act, or GINA, was passed in 2008 and enacted in May 2009 and works together with pre-existing nondiscrimination laws such as the Health Insurance Portability and Accountability Act .
GINA generally forbids health insurers or health plan administrators from using genetic test results for decisions regarding coverage or rates health insurance companies cannot consider genetic testing results as a preexisting condition. GINA also protects the individual from hiring, firing, or promotional decisions in the workplace based on genetic information. There is also additional protection available under individual states laws and through the Affordable Care Act.
What Preventive Services Arent Free
If your doctor finds something during a screening that requires additional treatment, you may have to pay extra, for example, if your doctor finds and removes a polyp during a colonoscopy. You also will pay extra if you schedule a separate doctor visit before or after receiving your screening.
Also in 2022, Medicare covers the following preventive services, but you must pay the 20 percent Part B coinsurance:
- Diabetes self-management training. Up to 10 hours of education to help people diagnosed with diabetes lower their blood sugar, prevent complications and improve their quality of life.
- Glaucoma tests. Every 12 months if you have certain factors that give you higher risk of developing this eye disease that can cause blindness.
- Screening barium enemas. This colorectal cancer test is covered every 48 months if youre 50 or older instead of a flexible sigmoidoscopy or colonoscopy. If youre at high risk for colorectal cancer and 50 or older, Medicare covers the test every 24 months.
Keep in mind
If you have coverage through a Medicare Advantage plan, rather than original Medicare, the plan must cover free preventive services without any cost to you if you use an in-network provider. You may be charged if you use an out-of-network provider.
You May Like: Does Medicare Pay For Laser Cataract Surgery
Evidence Of Benefits From Early Detection Of Skin Cancer Through Screening
The best evidence of benefit from skin cancer screening would come from a prospective randomized clinical trial that randomly selected people to be screened or not screened and then followed both groups long enough for differential outcomes to be evident. Because cancer screening trials typically require very large study populations, long follow-up periods, and significant administrative complexities, they usually have been undertaken only for cancers that affect many people and cause major mortality and morbidity.
The committee identified no randomized trials of clinical skin cancer screening. Discussions during the committee’s June 1999 workshop indicated that such a clinical trial would require from one-half million to one million participants and would not likely be funded in the United States. The committee heard that a trial is underway in Australia involving at least 500,000 people in 60 communities that have been randomly assigned to have a screening program established or to continue with current care. Current care includes intensive education and awareness campaigns for both the general population and the health professions. The study was reported to be in its first year of a 10-year follow-up period.
Medicare Covers Skin Cancer Screening: Different Types Of Skin Cancer
Skin cells themselves are where skin cancer first appears. Even while other cancers can spread to the skin due to their nature and place of origin, these are not thought of as skin cancers. There are three prevalent kinds of skin cancer, according to the American Cancer Society:
| Squamous cell carcinomas | It is more common for cancer in the outer epidermis cells to spread to deeper skin layers and other body regions. |
| Basal cell carcinomas | When left untreated, cancer in the lower epidermis cells might infect surrounding bone or other tissue because of its slow growth. |
| Melanomas | When left untreated, cancer in the skins pigmented cells can grow and spread rapidly. |
These less rare forms of skin cancer account for fewer than 1% of skin cancer diagnoses.
| Soft tissue sarcomas | Although the majority of soft tissue sarcomas are exceptionally rare, this category of skin cancer includes all sarcomas that manifest in tissues, including muscle, blood vessels, nerves, fat, or other regions of the epidermis. |
| Merkel cell carcinoma | Carcinoma, Merkel cell, or neuroendocrine, is the term for cancer that arises in a nerve or hormone-producing cell. |
| Skin adnexal tumors | The skins glands and hair follicles are where this cancer first develops. |
| Cutaneous lymphoma | A non-Hodgkin lymphoma kind that starts in the skins lymphoid tissue. |
Recommended Reading: What Is The Difference Between Medicare & Medicaid
Rules On Free Screening Tests
Here’s what you should know about cancer screening tests:
Does everyone get a free screening? People who are in grandfathered or short-term health plans may not be eligible for these benefits.Call your insurance company to see if you get free screening tests. Otherwise, you might need to meet your planâs deductible or pay a copay or coinsurance at the time of your appointment.
Your state might require that private health plans and Medicaid offer free screenings. Call your state health department or Medicaid office to see what is covered. Medicare does cover cancer screenings free of charge.
Keep in mind, though, that screening tests without any extra costs are just for people who donât have any symptoms. If you have symptoms and your doctor orders a colonoscopy, it is not considered a preventive screening test and is likely to come at a charge . If you have colon cancer and get a colonoscopy, it is not free either. In both of these cases, a colonoscopy is a diagnostic test, not a screening test.
Can I make an appointment just for the free screening? You can schedule a cancer screening by itself or as part of your annual checkup. For some screenings, you might need a separate visit to the doctor. A colonoscopy is one example. You can have others, like a Pap test, during a regular checkup.
Show Sources
Does Medicare Cover Dermatology Cancer Screening
If a dermatologist appointment is required for a medical reason, such as to check or further evaluate a skin lesion or mole, Medicare will cover the cost? However, a dermatologists preventive melanoma screening or skin check is typically not covered. Call your Medicare Advantage plan if you have one to find out the specifics of your coverage.
You May Like: Is Massage Covered By Medicare
Does Medicare Advantage Cover Cancer Screenings And Treatments
If you have a Medicare Advantage plan, the plan must still provide at the least the same coverage as Original Medicare but it could have different rules and costs. If you have cancer and a Medicare Advantage plan be sure to check with your plan provider to understand what the rules and costs may be for screenings, chemotherapy, radiation and other related services or items needed for your treatment.
Different parts of Medicare can help cover the various screenings, treatments and prescription drugs you may need as part of your cancer treatment plan. Make sure to always read your coverage details carefully so you understand what is covered, how and where youll need to receive treatments, and what your costs will be.
For further information related to how Medicare works for cancer-related health services, tests and treatments, please see the various reference sources listed below.
Reducing Hereditary Cancer Act Promises To Expand Access To Cancer Screenings And Interventions For High
Bipartisan legislation will remedy outdated policy to facilitate cancer prevention and early detection, aligning genetic risk assessment and related health services with guideline-recommended care
Newswise Washington DC Yesterday, United States Senators Ben Cardin and Lisa Murkowski introduced the Reducing Hereditary Cancer Act, bipartisan legislation to expand access to medically-appropriate genetic testing to determine an individuals risk of developing hereditary cancerand access to evidence-based medical care to reduce risk for those who have a predisposing genetic mutation. The Senate bill is identical to H.R. 4110, introduced in the House in June of 2021.
Medicare currently covers genetic testing only for people who have already been diagnosed with cancer, regardless of a history of cancer or known genetic mutations in their family. It does not cover medically necessary cancer screenings or risk-reducing interventions for individuals who have a genetic mutation increasing their cancer risk.
FORCE: Facing Our Risk of Cancer Empowered and the National Comprehensive Cancer Network® are proud to advocate for this legislation that would remedy a longstanding Medicare gap, ensuring that beneficiaries at increased risk of cancer have access to standard-of-care genetic counseling, testing, screening, and risk-reducing interventions.
Resources:
Don’t Miss: Are You Eligible For Medicare At 62
Does Medicare Cover Radiation Therapy
Medicare Part A or Part B may cover radiation therapy. Part A will provide coverage for radiation therapy if youre an inpatient, and youll pay the Part A deductible and coinsurance. Part B will provide coverage if you receive radiation therapy as an outpatient or as a patient of a freestanding clinic. You will pay 20 percent of the Medicare-approved amount and be responsible for the Part B deductible if therapy is done at a freestanding clinic.
Does Insurance Cover Brca Testing
In the United States, BRCA testing is usually covered by insurance if the patient meets certain criteria. Insurance coverage and criteria varies by insurance plan, and genetic counselors will review potential costs and insurance coverage with you during your appointment.
Some insurance companies have specific testing criteria or do not cover testing in certain situations, even when it is considered medically appropriate. For example, Medicare has specific BRCA testing criteria that only includes individuals with a personal history of cancer. Therefore, Medicare does not cover someone with a known mutation in the family who has no personal history of cancer. Medicaid coverage typically varies by state.
Don’t Miss: Is Medicare A Social Security Benefit
What Are The Costs Of A Doctor Visit For Medicare Skin Cancer Screening 2022
You will incur some out-of-pocket fees for dermatologist appointments, as with the majority of Medicare doctor visits. If you just have Original Medicare, you will also need to pay a 20% coinsurance payment in addition to your deductible . Some Medicare Supplement plans, often known as Medigap, can assist in defraying dermatologists out-of-pocket expenses.
Accuracy Of Screening Tests
The literature review in identified four recent studies of screening by total skin examination for both melanoma and nonmelanoma skin cancers . As summarized in , these studies found suspicious lesions in from 4 to 28 percent of those screened. Between 30 and 58 percent of those found to have a suspicious lesion who then followed up and had a biopsy were diagnosed with some form of skin cancer, mostly basal cell carcinomas. It is important to distinguish between the number who were referred for biopsy on the basis of a positive screen and the usually smaller number who actually followed up and had a biopsy. When analyses of the outcome of the screening program also included those who were referred for a biopsy but did not have one, the percentages of those with a positive screening result who were diagnosed with skin cancer dropped considerably for two studies. This latter kind of analysisincluding all those referred for further testingbetter reflects the reality that people do not always follow up as advised.
One study did follow patients with negative screening results for 42 months . Of the 15 patients diagnosed with skin cancer by the end of that period, a review of their records showed three lesions that had been misdiagnosed during the earlier screening . Thus, those with an initial negative result had a 99.8 percent chance that the initial negative result was accurate.
Don’t Miss: Does Aarp Medicare Complete Cover Dental
What Are Your Cancer Treatment Options
Cancer treatment is highly individualized. Several types of doctors work together to come up with a treatment plan that addresses your needs. A comprehensive cancer treatment plan will include one or more of the following types of treatments, all of which can be covered by Medicare.
- Surgery. Surgery may be recommended for removing cancerous tumors.
- Chemotherapy.Chemotherapy involves chemicals given orally or intravenously to kill cancer cells and stop cancer from spreading.
- Radiation.Radiation therapy uses intense beams of energy to kill cancer cells.
- Hormone therapy.Hormone therapy uses synthetic hormone and hormone blockers to target cancers that use hormones to grow.
- Immunotherapy.Immunotherapy drugs use your bodys immune system to attack cancer cells.
- Genetic therapy. These newer therapies typically deliver a virus to a cancer cell that will target and help destroy it.
One kind of cancer treatment that isnt covered by Medicare is alternative or holistic therapy. These treatments, which can include dietary changes, supplements, oils, and natural extracts, are not part of Medicares cancer coverage.
Statements Of Others About Skin Cancer Screening
A number of organizations have made statements and recommendations about clinical screening for skin cancer. The organizations vary in the extent to which they explicitly link their conclusions to systematic assessments of the evidence.
The U.S. Preventive Services Task Force stated that there is insufficient evidence for or against routine screening for skin cancer by primary care physicians using total body skin examination. Clinicians should remain alert for skin lesions with malignant featureswhen examining patients for other reasons especially those with established risk factors . A recommendation to consider referring to skin cancer specialists for evaluation and surveillance may be made on the grounds of patient preference or anxietyalthough evidence of benefit from such referral is lacking. The USPSTF is again reviewing the evidence related to skin cancer screening and could reaffirm or change its 1996 recommendation, but an announcement is not expected before the release of this report.
Since 1985, the American Academy of Dermatologists has sponsored free skin cancer examinations as part of a public education program . The Academy’s materials for the public stress sun avoidance and skin self-examination rather than routine clinical skin examinations for asymptomatic individuals.
You May Like: Where Do I Send My Part B Medicare Application