Fast Facts On Kidney Disease
Chronic kidney disease affects more than 1 in 7 U.S. adultsan estimated 37 million Americans.1 For Americans with diabetes or high blood pressurethe two most common causes of kidney diseasethe risk for CKD is even greater. Nearly 1 in 3 people with diabetes and 1 in 5 people with high blood pressure have kidney disease.1 Other risk factors for developing kidney disease include heart disease and a family history of kidney failure.
Despite the prevalence of kidney disease in the United States, as many as 9 in 10 people who have CKD are not aware they have the disease.1 Early-stage kidney disease usually has no symptoms, and many people dont know they have CKD until it is very advanced. Kidney disease often gets worse over time and may lead to kidney failure and other health problems, such as stroke or heart attack. Approximately 2 in 1,000 Americans are living with end-stage kidney disease kidney failure that is treated with a kidney transplant or dialysis.2
Learn more about kidney disease from the National Institute on Diabetes and Digestive and Kidney Diseases . The NIDDK spearheads research to improve kidney disease management and treatment. For information about current studies, visit ClinicalTrials.gov.
What Major Innovations And Reforms Have Recently Been Introduced
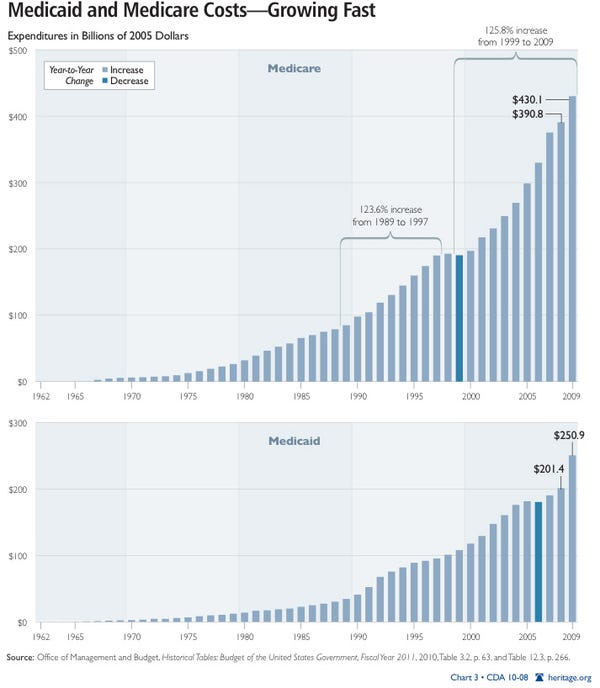
Medicare and Medicaid Innovations. The Affordable Care Act ushered in sweeping insurance and health system reforms aimed at expanding coverage, addressing affordability, improving quality and efficiency, lowering costs, and strengthening primary and preventive care and public health. The most important engine for innovation is the new Center for Medicare and Medicaid Innovation. The ACA allocated $10 billion over 10 years to the agency with the mandate to conduct research and development that can improve the quality of Medicare and Medicaid services, reduce their costs, or both.
If initiatives undertaken by the Center for Medicare and Medicaid Innovation are certified by federal actuaries as improving quality of care at the same costor maintaining quality while reducing health care coststhe U.S. Secretary of Health and Human Services has the authority to spread these initiatives, without congressional approval, throughout the Medicare and Medicaid programs.
The Trump administration has rolled out several other changes to the Medicare and Medicaid programs. These include the 2019 announcement of Primary Care First, a new voluntary payment model intended for launch in 2021 that aims to simplify primary care physician payments. In addition, since 2018, several states have instated a requirement for able-bodied individuals to document that they are meeting minimum work requirements to qualify for or keep their Medicaid coverage.
34 Ibid.
How Often Do People In The United States Access The Internet
According to a report, almost half of the internet users in the US use the internet several times per day, and 31% use the internet almost constantly.
Lets take a look at how often people in the United States access the internet:
- 48% access the internet several times per day
- 31% access the internet almost constantly
- 7% never access the internet
- 6% access the internet once a day
- 4% access the internet several times per week
- 4% infrequently access the internet
Read Also: What Income Is Used For Medicare Part B Premiums
Distribution Patterns Of Medicare Reimbursement
Although discussions of per capita reimbursements for the aged and disabled provide a broad overview of the average experience, they obscure the important fact that large variations exist in the use of services by beneficiaries. As shown in Table 27, the average Medicare reimbursement for an aged enrollee in 1983 was $1,724. Yet, as in all other years, a large proportion of aged enrollees in 1983 had small claims or none at all. As shown in Table 28, 37.4 percent of all aged enrollees had no reimbursements made on their behalf, and an additional 33 percent had reimbursements of less than $500. Thus, 70 percent had reimbursements less than $500 and 30 percent had reimbursements that were $500 or more.
Which States Have The Highest Percentage Of People Covered By Group Health Insurance
The states with the greatest percentage of residents who have employer-sponsored health insurance coverage are:
Each of these states has more than half of its people covered by group health insurance.
Recommended Reading: What Is Qualified Medicare Beneficiary
Quality Of Beneficiary Services
A 2001 study by the Government Accountability Office evaluated the quality of responses given by Medicare contractor customer service representatives to provider questions. The evaluators assembled a list of questions, which they asked during a random sampling of calls to Medicare contractors. The rate of complete, accurate information provided by Medicare customer service representatives was 15%. Since then, steps have been taken to improve the quality of customer service given by Medicare contractors, specifically the 1-800-MEDICARE contractor. As a result, 1-800-MEDICARE customer service representatives have seen an increase in training, quality assurance monitoring has significantly increased, and a customer satisfaction survey is offered to random callers.
What Is A Small Business Hra
Small business HRAs are health care plans designed for small businesses to offer to their employees. This type of health reimbursement arrangement is specially designed for organizations with smaller profit margins and less capital to provide insurance coverage for their employees. As mentioned above, the more people who have health insurance, the less of a burden it is on the taxpayers. Therefore, it is in the interest of the public purse for these types of plans to exist.
Today, Qualified Small Employer HRAs are increasingly popular as a solution that works well for proprietors and their employees and families. These types of plans are an excellent resource for employers who see the value of investing in a healthy, secure workforce.
Don’t Miss: Does Medicare Cover Nursing Home For Dementia Patients
Should I Sign Up For Medical Insurance
With our online application, you can sign up for Medicare Part A and Part B. Because you must pay a premium for Part B coverage, you can turn it down.
If youre eligible at age 65, your Initial Enrollment Period begins three months before your 65th birthday, includes the month you turn age 65, and ends three months after that birthday.
Note: Important Upcoming Change Rules for 2023 and later: If you accept the automatic enrollment in Medicare Part B or if you sign up during the first three months of your IEP, your coverage will start the month youre first eligible. Beginning January 1, 2023, if you sign up during the month you turn 65 or during the last three months of your IEP, your coverage starts the first day of the month after you sign up.
The following chart shows when your Medicare Part B becomes effective in 2022:
| In 2022, if you sign up during this month of your IEP | Your Part B Medicare coverage starts |
|---|---|
| One to three months before you reach age 65 | The month you turn age 65. |
| The month you reach age 65 | One month after the month you turn age 65. |
| One month after you reach age 65 | Two months after the month of enrollment. |
| Two or three months after you reach age 65 | Three months after the month of enrollment. |
The following chart shows when your Medicare Part B becomes effective in 2023:
How Much Is Medicaid Spending In 2019
In 2019, Medicaids share of total U.S. health care spending amounted to 16 percent. The program is funded by both federal and state government. As the percentage of people under Medicaid was growing during the last decade, Medicaid spending was increasing, too. According to estimates of the Centers for Medicare and Medicaid Services ,
Don’t Miss: Does Medicare Pay For Power Chairs
How Many People Use Tiktok In The Us In 2023
- Fact Checked by
Quick Answer
How many people use Tiktok in the US in 2023?
TikTok is a social video app that allows users to create and share various videos.
It was the in 2021 and was identified as a fast-growing social media app in the US.
This platform recorded 1.2 billion monthly active users worldwide in the fourth quarter of 2021 and was projected to exceed 1.8 billion the following year.
It is accessible in 154 countries and has 75 available languages.
Are you using TikTok and curious about how many people use this platform in your country? This article will give you the answer.
Should I Take Medicare Part B
You should take Medicare Part A when you are eligible. However, some people may not want to apply for Medicare Part B when they become eligible.
You can delay enrollment in Medicare Part B without penalty if you fit one of the following categories.
Employer group health plans may cover items normally not covered by Medicare Part B. If so, and you meet one of the categories above or below, then you may not need to enroll in Medicare Part B and pay the monthly premium.
If you are:
- a spouse of an active worker
- a disabled, active worker
- a disabled spouse of an active worker
and choose coverage under the employer group health plan, you can refuse Medicare Part B during the automatic or initial enrollment period. You wait to sign up for Medicare Part B during the special enrollment period, an eight month period that begins the month the group health coverage ends or the month employment ends, whichever comes first.
You will not be enrolling late, so you will not have any penalty.
If you choose coverage under the employer group health plan and are still working, Medicare will be the “secondary payer,” which means the employer plan pays first.
If the employer group health plan does not pay all the patient’s expenses, Medicare may pay the entire balance, a portion, or nothing. An employer group health plan must be primary or nothing.
You May Like: How Much Does Medicare Cover For Dental
General Fund Revenue As A Share Of Total Medicare Spending
This measure, established under the Medicare Modernization Act , examines Medicare spending in the context of the federal budget. Each year, MMA requires the Medicare trustees to make a determination about whether general fund revenue is projected to exceed 45 percent of total program spending within a seven-year period. If the Medicare trustees make this determination in two consecutive years, a “funding warning” is issued. In response, the president must submit cost-saving legislation to Congress, which must consider this legislation on an expedited basis. This threshold was reached and a warning issued every year between 2006 and 2013 but it has not been reached since that time and is not expected to be reached in the 20162022 “window”. This is a reflection of the reduced spending growth mandated by the ACA according to the Trustees.
Prevalence Of Multiple Chronic Conditions Among Us Adults 2018
RESEARCH BRIEF â Volume 17 â September 17, 2020
Peter Boersma, MPH1 Lindsey I. Black, MPH1 Brian W. Ward, PhD2
Suggested citation for this article: Boersma P, Black LI, Ward BW. Prevalence of Multiple Chronic Conditions Among US Adults, 2018. Prev Chronic Dis 2020 17:200130. DOI: .
PEER REVIEWED
Summary
What is already known on this topic?
Research has shown increases in the overall percentage of US adults with multiple chronic conditions, as well as variation by population subgroups.
What is added by this report?
In 2018, 51.8% of US adults had at least 1 chronic condition, and 27.2% had multiple chronic conditions. Prevalence was highest among women, non-Hispanic white adults, adults aged 65 or older, and those living in rural areas.
What are the implications for public health practice?
These results may inform efforts to track and monitor multiple chronic conditions among the US population.
Recommended Reading: Does A Medicare Advantage Plan Replace Medicare
What Is Medicare Part B
Part B benefits are, for most people, the most-used part of Medicare. This part of Medicare covers outpatient care, including most tests and doctor visits. It will also cover durable medical equipment, such as wheelchairs and hospital beds under some circumstances.
In 2023, Part B has a deductible of $226. For many procedures, you will also pay a coinsurance fee of 20 percent for applicable procedures. The Part B premium is $164.90. Although you can pay this directly to Medicare, for many people it will be more convenient to have the costs deducted directly from your Social Security check each month.
What Did Medicare Cost In 2021 What Does It Cost In 2022
Medicare Part A is free for most people receiving Social Security. Those enrollees that pay for Part A of Medicare paid up to $471 every month in 2021. This increased to up to $499 per month in 2022.
Medicare Part B cost $148.50 per month in 2021. In 2022, Part B costs $170.10 per month. Depending on your income, your Part B premium may be higher.
Medicare Part C premiums vary by plan, but the average premium across all plans was $21.22 per month in 2021 and is $19 per month in 2022.
Medicare Part D premiums also vary by plan but the average premium was $31.47 per month in 2021 and is $33 per month in 2022.
This is the cost of the monthly premium and does not include copays, coinsurance, or deductibles.
Some consumers with lower incomes may qualify for cost subsidies like Extra Help or a Medicare Savings Program, which could significantly lower these costs.
Read Also: Does Medicare Cover Ear Nose And Throat Doctors
Families Usa Works To Preserve And Improve The Protections That Medicare Provides Us
Health care costs should not be shifted to those who can least afford them. Thats why we work to protect low income people with Medicarewe promote changes in federal policy to expand enrollment in programs that serve Medicare beneficiaries with limited incomes.
For years, we have joined national and state advocacy organizations to beat back proposals that increase costs for beneficiaries by shrinking Medicare. In partnership with those groups, we work with federal officials to ensure that changes to Medicare meet the needs of the people it serves.
Medicare Trends In Price
- In 2018, 15% of the total federal spending budget was spent on Medicare. This number is projected to rise to 18% of the federal budget by 2029 .
- A 2019 Medicare Trustees report projected that the Medicare Part A fund will be depleted by 2026 .
- Medicare consumers spent more out-of-pocket on prescription drugs in 2016 than on doctors visits and hospital care combined .
Recommended Reading: Do I Need To Keep Medicare Summary Notices
What Are The Major Strategies To Ensure Quality Of Care
The ACA required the U.S. Department of Health and Human Services to establish a National Quality Strategy,32 a set of national aims and priorities to guide local, state, and national quality improvement efforts, supported by partnerships with public and private stakeholders. The strategy includes annual reporting on a selected set of quality measures.33
Since 2003, the Agency for Healthcare Research and Quality has published the annual National Healthcare Quality and Disparities Report, which reports on national progress in health care quality improvement. The 2018 report found that the quality of U.S. health care had improved overall from 2000 to 2016, but that improvement was inconsistent. For example, while most person-centered care and patient-safety measures improved, affordability did not.34
Federal law requires certain providers to report data on the quality of their care, and the Centers for Medicare and Medicaid Services to publicly report performance on quality measures. For example, Hospital Compare is an online public resource summarizing the performance of more than 4,000 hospitals on measures of care processes, care outcomes, and patient experiences. Related quality-reporting programs include Nursing Home Compare and Physician Compare.
Dont Miss: How To Hide Money From Medicaid
What Should You Do If You Are Injured In A Boating Accident
You should get prompt medical help if you are hurt in a boating accident. Have your doctor document your injuries in case you wish to recover compensation. You should report the accident to your insurer if you are the owner of a vessel damaged in the incident. You may also be able to make a legal claim against those responsible for the accident. An experienced boating accident attorney can help you to understand and enforce your rights.
Also Check: Do You Have To Have Social Security To Get Medicare
Social Security & Medicare
Social Security provides cash benefits to retirees and those unable to work due to disability. Medicare is a public healthcare program for people over 65, as well as those enrolled in Disability Insurance and those with end-stage renal disease. Combined, Social Security and Medicare account for more than a quarter of all government spending in the United States.
State Children’s Health Insurance Program
What do I worry about as a parent? I know one of my biggest worries is my daughter’s well-being. If she is healthy the rest we can deal with. Last year for several months, we were without health insuranceand I really felt we were living on borrowed time. I was constantly worriedwhat if my daughter breaks her arm, or was in a car accident, or just got really sickhow would I pay for that with no health insurance? It’s a frightening position to be in.
Kentucky Parent
Before Medicare was enacted, the elderly were among the population groups most likely to be without health insurance. Now, children are among the population groups most likely to be without health insurance: more than 11 million children, or one in seven, are uninsured. To address this problem, the SCHIP was enacted in 1997 to provide health insurance coverage to children from working families who do not qualify for Medicaid and cannot afford private insurance.
Recommended Reading: How Much I Have To Pay For Medicare
