What Is Texas Medicaid
Texas Medicaid encompasses a variety of programs to provide financial health care coverage to eligible individuals throughout the state. Providing coverage for families, individuals and older adults, Texas Medicaid strives to preserve the well-being of Texans by providing quality health care services that can be accessed within beneficiaries communities.
In Texas, there are five types of Medicaid coverage:
- STAR
- STAR Health
- Traditional Medicaid
Each of the STAR programs provides managed care for recipients. While STAR, STAR Kids and STAR Health offer services for families, kids and pregnant women, STAR+PLUS features managed care for those aged 65 and older and individuals who are living with disabilities. Traditional Medicaid covers individuals who arent eligible for managed care.
Nc Medicaid Managed Care Started July 1 2021
NC Medicaid Managed Care health plans are now active. This means that you will now get care through your health plan. If you have questions about benefits and coverage, call your health plan. You can find the number on your new Medicaid ID card or visit .
You can also contact the NC Medicaid Ombudsman if you have questions or problems your health plan or provider could not answer. Call 1-877-201-3750 or visit ncmedicaidombudsman.org.
Meetings and events
You can schedule rides to medical appointments. Learn more about transportation services.
Get the free mobile app
To get the app, search for NC Medicaid Managed Care on or the App Store.
Use the app to find and view primary care providers and health plans for you and your family. Learn more about the free mobile app at .
You May Like: Does Medicaid Cover Ivf Treatment
Qualified Medicare Beneficiary Programs And Medicare Advantage
If youre currently in the QMB program, you can enroll in a Medicare Advantage plan. There are unique plans for those with Medicare and Medicaid. A Medicare Advantage Special Needs Plan for dual-eligible individuals could be a fantastic option. Generally, there is a premium for the plan, but the Medicaid program will pay that premium.
Many people choose this extra coverage because it provides routine dental and vision care, and some come with a gym membership. While not every policy has these benefits, there may be one available in your area!
You May Like: Does Medicare Cover Wheelchairs And Walkers
How To Apply For A Qualified Medicare Beneficiary Program
Anyone interested in applying for a QMB program must contact their states Medicaid office. If your income is higher than the QMB requirements, you should still reach out to determine eligibility.
Each states Medicaid program pays the Medicare cost-sharing for QMB program members. Anyone who qualifies for the QMB program doesnt have to pay for Medicare cost-sharing and cant be charged by their health care providers.
If an individual is considered a QMB Plus, they meet all criteria for the QMB program but also meet all financial requirements to receive full Medicaid services. These enrollees can receive benefits through the QMB program as well as their states health plan.
The first step in enrollment for the QMB program is to find out if youre eligible. A quick and easy way to do this is to call your local Medicaid office. The next step is to complete an application. You can request Medicaid to provide you with an application form or locate a QMB program application from your state online.
Medicare And Medicaid: How To Qualify For Both

Home / FAQs / General Medicare / Medicare and Medicaid: How to Qualify for Both
Medicare and Medicaid are different programs. Depending on your healthcare and financial situation, its possible to have both. But, just because you have one, doesnt mean youll automatically have the other. Medicare is a federal program, while Medicaid is a state program.
Don’t Miss: Can I Get Medicare If I Live Outside The Us
How Can You Find Out If Someone Is On Medicaid
Contact your state Medicaid office to ask about Medicaid eligibility tools. Many states offer online benefit-checking tools that require entering an individuals name and either a Social Security number or Medicaid number. Enter in all requested information in the forms on the benefit eligibility screening tool.
How Do I Know If I Should Be Dual Eligible
Beneficiaries can find out if theyre eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a beneficiarys state should provide the number to call but beneficiaries should make sure they are contacting a government office before sharing any personal information.
The Centers for Medicare and Medicaid Services also maintains a list of state agencies that oversee Medicaid. Beneficiaries can see if they already have Medicaid by contacting 1-800-MEDICARE and asking whether they receive Extra Help with their prescription drug costs .
Don’t Miss: Can I View My Medicare Eob Online
Medicaid Enrollees Need Access To Dental Vision And Hearing Services
Fixing gaps in coverage only in Medicare without making the corresponding changes in Medicaid would exclude many people with significant unmet needs. Providing access to a full range of preventive services and treatment for non-elderly adults with Medicaid coverage could prevent more serious conditions later in life as well as the need for more invasive, costly procedures.
As shown in Figure 4, while a significant share of traditional Medicare enrollees aged 65 and over report having unmet dental needs due to cost, the share is almost two-thirds higher among Medicaid enrollees under age 65, who are low income by definition. While Medicaid enrollees under the age of 21 are eligible for dental care as part of the Early and Periodic Screening, Diagnostic, and Treatment benefit, once young adults turn 21, many no longer have access to treatment options. Adult Medicare beneficiaries under age 65 with disabilities many of whom also receive Medicaid face disproportionate challenges in obtaining needed dental care. Low-income seniors enrolled in both Medicare and Medicaid also have higher rates of unmet dental needs due to cost than other Medicare enrollees.
Congress would need to make various design decisions in adding dental, vision, and hearing benefits to Medicaid. They include: how the federal government and states would share the cost what benefit standards the federal government would set and whether Congress would permit nominal cost sharing.
Will Medicaid Provide Payment For A Family Member Who Needs Nursing Home Care
Louisianaâs Medicaid Program provides payment for special long term care support services, as well as full Medicaid health coverage, to eligible people who, because of their medical condition, require assistance with activities of daily living . Long-term care supports may be provided either in a facility or in an individualâs own home or in the community. Visit Medicaid Long-Term Care.
You May Like: Family Doctors In Charleston Wv That Accept Medicaid
Recommended Reading: Does Medicare Pay For Inogen Oxygen Concentrator
Millions Under Expanded Medicaid Will Transition To Medicare
There are currently almost 20 million people covered under expanded Medicaid, accounting for almost a quarter of all Medicaid enrollees nationwide. Under ACA rules, there are no asset limitations for Medicaid eligibility for pregnant women, children, or adults eligible due to Medicaid expansion. Instead, eligibility is just based on an ACA-specific version of modified adjusted gross income , along with immigration status.
But Medicaid expansion and the MAGI-based eligibility rules only apply to adults under the age of 65. After that, expanded Medicaid is no longer available. To be clear, Medicaid remains available after age 65 and many older adults rely on it for example, the majority of nursing home residents in the United States have Medicaid coverage in addition to their Medicare coverage.
But once you turn 65, eligibility for Medicaid is based on both income and assets. Theres some variation from one state to another , but in general, the income limits are lower than those that apply to the Medicaid expansion population, and the asset limits are quite restrictive.
This can lead to some sticker shock for people who were eligible for expanded Medicaid prior to turning 65, but then have to transition to Medicare possibly without eligibility for any further Medicaid assistance once they turn 65.
Billing Requirements For The Qualified Medicare Beneficiary Program
Providers cant bill QMB members for their deductibles, coinsurance, and copayments because the state Medicaid programs cover these costs. There are instances in which states may limit the amount they pay health care providers for Medicare cost-sharing. Even if a state limits the amount theyll pay a provider, QMB members still dont have to pay Medicare providers for their health care costs and its against the law for a provider to ask them to pay.
Recommended Reading: What Is Step Therapy In Medicare
Frequently Asked Questions For Current Medicaid Beneficiaries
What is a Community Spouse?
A community spouse is someone whose husband/wife is currently institutionalized or living in a nursing home. The community spouse is not currently living in a nursing home and usually resides at the couple´s home.
I am a community spouse. Will I be allowed to keep any income or resources?
If your spouse is institutionalized or living in a nursing home, you will be permitted to keep some income known as a minimum monthly maintenance needs allowance . If you are currently receiving income in excess of the minimum monthly maintenance needs allowance, you may be asked to contribute twenty-five percent of the excess income to the cost of care for the institution
How do I find my local Medicaid office?
The Medicaid office is located in your local department of social services. A listing of offices can be located here:
If you live in the five boroughs of New York City, your offices are run by the Human Resources Administration . A listing of offices can be found here:
How do I order a new benefit card?
If your Medicaid is with your LDSS, to order a new Medicaid Benefit Identification Card, please call or visit your
If your Medicaid is with the and you need to order a new benefit card please call the call center at 1-855-355-5777.
Members residing in the five boroughs of NYC can call the HRA Infoline at 1 557-1399 or the HRA Medicaid Helpline at 1 692-6116.
How often do I have to renew?
Read Also: Does Disability Count As Income For Medicaid
How To Qualify For Medicare And Medicaid

Beneficiaries can enroll in Medicaid through the state program office. If you think youre eligible, contact your state health department to apply. To be eligible for Medicaid your income will need to be below a predetermined amount.
If your income is above this amount but you struggle with high medical costs, you may want to check if a Medicaid spend-down program is available in your state.
Youre eligible for Medicare if youre over the age of 65 or on disability for at least 24 months. Although, you apply for Medicare online at the Social Security Administration website.
You May Like: How To Register For Social Security And Medicare
What If I Dont Want My Medicaid Doctors And Providers To See My Health Information Through This Website
You can âopt outâ of sharing. âOpt-outâ means that you choose not to share your health information. To opt out, go to and then:
You can also opt out by calling 800-252-8263. If you opt out, we wonât share your health information with Medicaid doctors or other providers.
Read Also: Aged Blind Disabled Medicaid Nj
If I Have Medicaid Do I Need Medicare Part D
Those that have Medicare and Medicaid will automatically be enrolled in a Part D plan if they dont select one for themselves. Its in the enrollees best interest to select a policy to enroll in, instead of being dropped into a plan. But, either way, Medicaid will help cover the costs associated with premiums, copayments, or coinsurances.
You May Like: Does Medicare Part B Cover Mental Health Services
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
Are You Dual Eligible
Some people can be eligible for both Medicare and Medicaid at the same time.
Dual-eligible beneficiaries are individuals who are eligible for both Medicare and Medicaid.
People who are dual eligible share costs with state-run Medicare Savings Programs , which provide help with premiums, deductibles, coinsurance and copayments, depending on the participant’s income level and the specific MSP. There are programs where eligible participants may have no copayments or cost shares.
This material is provided for informational use only and should not be construed as medical advice or used in place of consulting a licensed medical professional. You should consult your doctor to determine what is right for you.
Humana is a Medicare Advantage HMO, PPO and PFFS organization and a stand-alone prescription drug plan with a Medicare contract. Humana is also a Coordinated Care plan with a Medicare contract and a contract with the state Medicaid program. Enrollment in any Humana plan depends on contract renewal.
Some links on this page may take you to Humana non-Medicare product or service pages or to a different website.
Y0040_GNHKMBZEN
Also Check: Who Is The Medicare Coverage Helpline
Can I Select An Insurance Plan For My Medicare And Medicaid Benefits
If you are dual eligible, you are can enroll in a dual eligible special needs plan that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid dont over individually, including over-the-counter items, hearing aids, and vision or dental care.
Beneficiaries who are dual eligible can change between Original Medicare and Medicare Advantage or switch Part D plans at each quarter.
Read more about the Medicaid benefits available to Medicare enrollees.
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals. In addition to advocacy work, Josh helped implement health insurance exchanges at the technology firm hCentive. He also has held consulting roles, including at Sachs Policy Group, where he worked with insurer, hospital and technology clients.
Not Enrolled To Medicaid Heres How To Apply
If you have not yet enrolled yourself and/or your family, there are multiple methods you can use to enroll in Medicaid. Your first option is to enroll yourself and/or your family by going online and filling out an application for yourself and/or your family at the Health Insurance Marketplace. There you can follow the steps to create an account and provide your information such as whether or not you have a disability, your income level, and enroll any minor dependent children you have in health coverage programs such as the Childrens Health Insurance Program, otherwise known as CHIP.
Another method you can use to enroll in the Medicaid program is to directly contact your states Medicaid agency. You can find the agency contact information you need by visiting the Healthcare website. Scroll down to the state in which you reside, and you will be taken to the website of your local Medicaid agency. There you will be provided with telephone numbers for your local Medicaid agency which you can call during normal business hours in order to check if you and/or your family qualify for Medicaid.
Recommended Reading: How Much Does Medicare Cover For Hospital Stay
Medicare Part B And Va Benefits
Medicare Part B can provide you with medical coverage and services outside of the VA health system. Therefore, it is recommended that you enroll in Medicare Part B in addition to your VA benefits. If you wait to enroll in Part B when you are first eligible, you will likely experience gaps in coverage and incur a penalty for each 12-month period you were without Medicare Part B coverage. Learn more about Medicare Part B.
The Difference Between Medicare And Medicaid
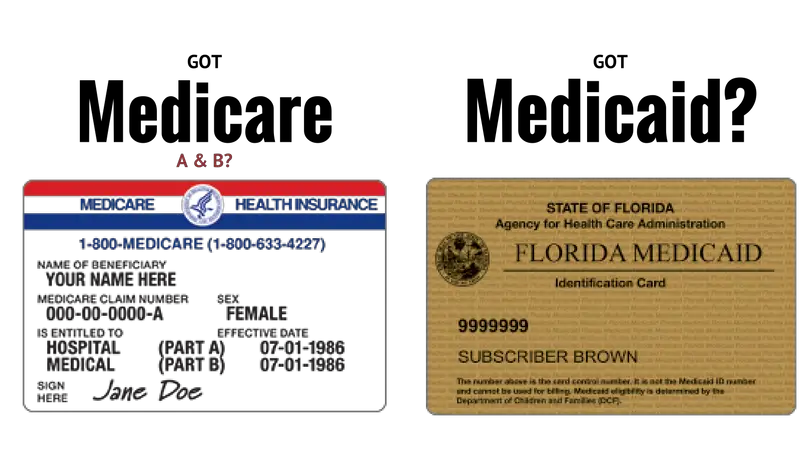
Although the two programs share the same prefix and offer health coverage, theyre different. Nearly every American will one day qualify for Medicare, but Medicaid is only for those with a low income.
With Medicare, think care for those 65+ or those with disabilities. Then, Medicaid is aid to those with a low income. Medicaid is free. Medicare is not free. Those with Medicaid wont be subject to the Part B premium or Part B late enrollment penalties. But, those with only Medicare will be responsible for applicable costs.
Just because Medicaid is free doesnt mean its for everyone. Approval time for Medicaid can take up to 60 days. Benefits are for US citizens but, children of illegal immigrants can qualify.
If you get Social Security supplemental benefits, youll qualify for Medicaid. Also, Medicaid has benefits Medicare doesnt this includes vision, dental, and long-term custodial care.
Recommended Reading: How Can I Sign Up For Medicare Part B
