Psychiatric Prescription Drug Coverage
When it comes to mental health care, drug coverage is a distinct area under Medicare. Drugs are covered by Part D plans, not Original Medicare. This means that if you want prescription drug coverage, you need to get one of these plans — no exceptions.
Part D plans are offered by private insurance companies, not by the government. This means that unlike Original Medicare, prices and coverage will both vary.
Compare Medicare Advantage Plans That Cover Counseling
For California residents, CA-Do Not Sell My Personal Info, .
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
How Does Medicare Work For Therapy
Medicare covers many forms of therapy, including psychotherapy. This is also referred to as talk therapy. Studies show that psychotherapy tends to be beneficial to about 75% of the people who pursue it to address mental health challenges.
Medicare also helps cover hospitalization at a general or psychiatric hospital if you are admitted for inpatient care. Medicare limits the number of days of inpatient psychiatric hospital services covered during your lifetime.
Your mental health therapy and other services typically are not free under Medicare. You may get free mental health screenings, but you typically have to pay 20% of the Medicare-approved amount for the majority of services. Your total out-of-pocket expenses will depend on your deductible, coinsurance, provider fees, and location where you receive services.
Don’t Miss: Does Medicare Cover Any Medical Alert Systems
How To Verify Medicare Mental Health Benefits
Athena Care is in-network with many insurance plans and providers. The simplest and fastest way to find out if Medicare covers behavioral health therapy and services is to fill out our free and confidential online insurance verification form.
Allow our highly trained and knowledgeable care coordinators to manage the challenges of contacting your insurance company for information on your Medicare mental health coverage.
After completing the form, a care coordinator will review your insurance and thoroughly explain your options. Rest assured that any information exchanged or discussed will remain confidential.
Does Medicare Cover Mental Health Counseling In Texas
If youre struggling to understand Medicare in Texas, Connie can help. Ask Connie your question, and a local, licensed agent will help you navigate your Medicare journey.Complete this form to have your question answered. It could be featured on Dear Connie.
Dear Connie,
My husband and I are struggling because hes been feeling down lately.
Im trying my best to support him, but Im beginning to feel like he needs more help. And Im starting to feel hopeless in my efforts. This has been coming and going for a while now. Im wondering, does Medicare cover mental health and counseling in Texas?
Hoping for help,
Find the right Medicare plan for you
Dear Virginia,
Thank you for reaching out. There is help available for you both. If you or your husband are in crisis, please seek help immediately. You can call 911 or call or text the 988 Suicide and Crisis Lifeline at 988.
Mental health is an essential part of our overall well-being. Its estimated that 20% of people age 55 and older will experience a mental health concern. So, you and your husband are not alone. But, you should also know that its not a standard part of aging, so help should be sought out and is available.
Unfortunately, men over the age of 85 tend to experience conditions like anxiety or mood disorders at a higher rate, along with the highest suicide rate. We are happy that youve taken notice of mental health warning signs and are seeking help.
Read Also: What Is Original Medicare Plan
How Much Does Medicare Cover For Therapy
The typical monthly premium for Medicare Part B is $170.10 for 2022. It could be more than that if your income in 2020 exceeds the thresholds. There is also an annual deductible of $233. After you pay your deductible, you may have a coinsurance of 20%. The coinsurance is calculated using the Medicare-approved amount.
For example, suppose you have a $1,000 bill for mental health therapy services.
-
You will pay the $233 annual deductible. This is what you pay before Medicare covers any qualified expenses for therapy.
-
Then, you will pay 20% of $767 for coinsurance. Coinsurance represents your share of health care costs you split with your insurer until the end of the plan year. You pay your coinsurance after youve met your annual deductible.
-
Your total out-of-pocket expenses will be $386.40 . Traditional Medicare does not have any limits on out-of-pocket expenses.
Can A Supplemental Medicare Plan Provide Coverage For Mental Health
A supplemental Medicare or Medigap plan is private insurance. You pay a monthly premium, and the policy covers one person. You still have to pay premiums on Medicare Part A and Part B.
Medigap plans are for the gaps in coverage for Medicare. These Medigap policies may include Plan A, B, C, D, F, G, K, L, M, or N. A Medigap plan will pay for all or part of the deductible, copays, and coinsurance for Medicare Part A and Part B. This includes coverage for qualified mental health services. You may want to seek the help of an insurance agent or financial planner to help you pick the best plan for you.
Also Check: Does Everyone Go On Medicare At 65
Does Medicare Cover Mental Health Counseling A Complete Guide
Never before have Americans been at such high risk for mental health disorders. Mental Health America reports that nearly one in five Americans is dealing with a mental illness right now. The number of mental health sufferers has gradually increased for several years. As the coronavirus pandemic hit, drastic changes to all aspects of Americans lives further exacerbated our mental health crisis.
Of the over 50 million Americans experiencing a mental illness right now, more than 12 million have admitted to having serious suicidal thoughts. That is equivalent to nearly 5% of all Americans. For multiracial individuals, the figure is more than twice as high.
Nearly one third of those suffering from any form of mental illness have been unable to find treatment. One in ten of those believe they are unable to afford medical care for their mental health problems. However, Medicare plans offer a range of mental health services to their beneficiaries. Here is a detailed look at Medicare plans for mental illness.
What Services Are Included In The Medicare Mental Health Benefits
Medicare mental health coverage is available in an inpatient or outpatient setting, depending onwhich is medically necessary for your treatment. The following services areexamples of whats covered by Medicare for people who need to be treated in aninpatient setting:
Some of the services available to people inoutpatient care include:
- Some medications, ifgiven in a medical setting
- Visits with a doctor orsocial worker
Theseare just a few examples of the services that Medicare offers. Medicare alsooffers an annual depression screening, which you can schedule this with yourprimary care physician at your convenience.
Don’t Miss: What Is The Window To Sign Up For Medicare
Lindsay Malzone Medicare Expert
Medicare beneficiaries might be aware that they have some sort of mental health coverage, but may not understand what it entails regarding services, co-payments, and prescriptions
When it comes to mental health benefits, Kayrish says keep the following in mind:
- Original Medicare includes a 20% co-insurance and if you have a supplement, it will most likely cover it.
- Medicare Advantage includes the same type of coverage and a co-payment.
- Medicare Advantage may require a gatekeeper system, which means your primary carephysician has to refer you to mental health care.
What Part Of Medicare Covers Mental Health Care
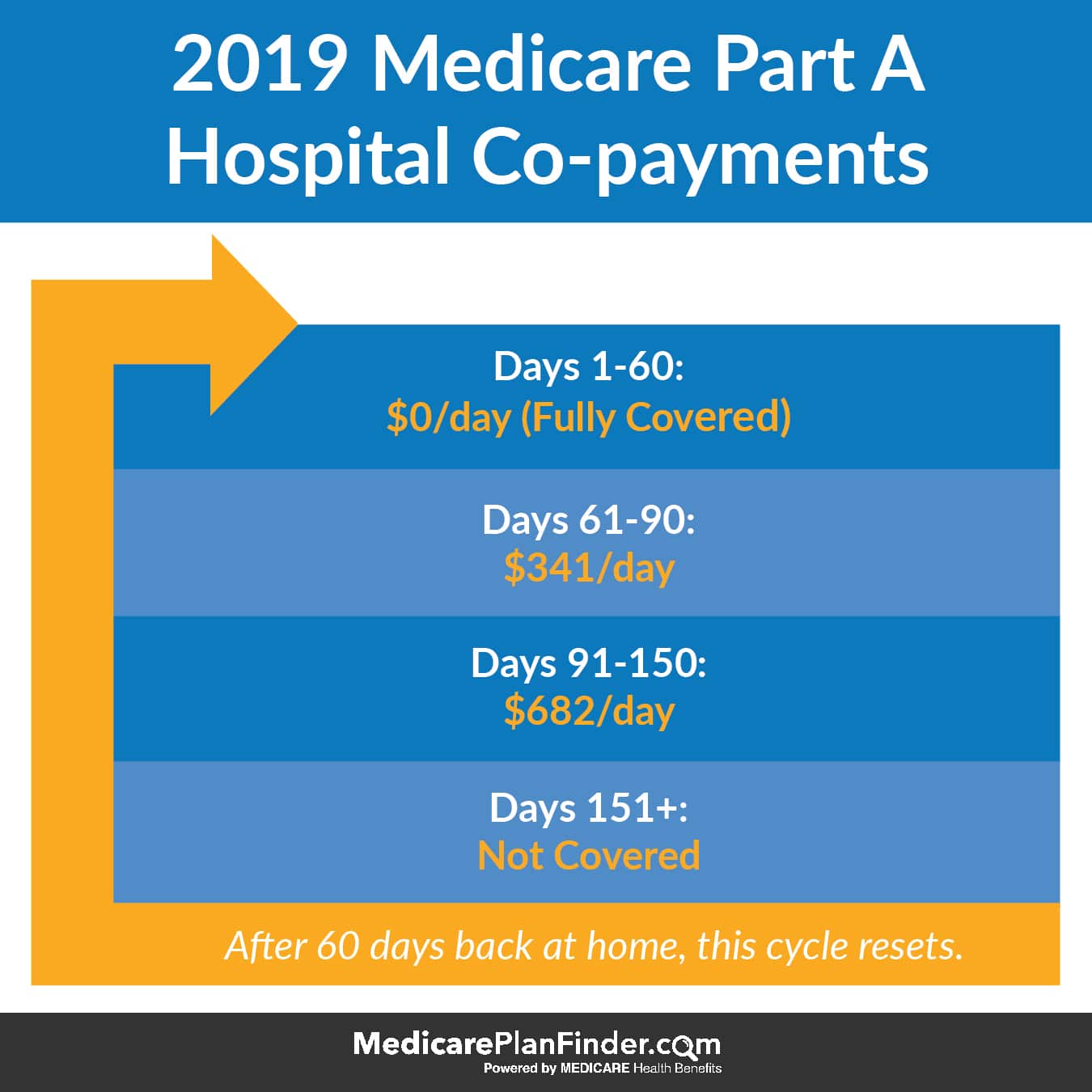
Medicare Part A covers mental health care in an inpatient setting. Part A mental health care is in a general hospital or a psychiatric hospital only for people with mental health concerns. If you get inpatient care in a psychiatric hospital, Part A will cover up to 190 days in a lifetime. There is no limit to the number of benefit periods you can have for mental health care in a general hospital.
Part A covers your room , meals, nursing care , therapy and treatment, lab tests, medications, and other services and supplies you need. Part A does not cover personal items or a phone or TV in your room.
Medicare Part B covers mental health care on an outpatient basis in these types of settings:
- A doctors or other health care providers office
- A hospital outpatient department
- A community mental health center
And from these types of providers :
- Psychiatrist or another doctor
- Clinical psychologist, social worker, or nurse specialist
- Nurse practitioner
- Physician assistant
Part B helps pay for these outpatient mental health services:
Part D helps cover self-administered prescribed drugs.
Medicare Advantage plans cover all services offered through Original Medicare Part A, Part B, and usually Part D. Copays and coinsurance amounts vary, depending on your plan. Providers and services must be in-network and typically require referrals and prior authorizations before you can receive services.
Recommended Reading: Are Medicare Supplement Plans Worth It
Does Medicare Cover Outpatient Mental Health Services
You must have Medicare Part B to be covered for outpatient mental health treatment, partial hospitalization, and annual depression screenings.
Like inpatient care, Medicare will cover most of your outpatient treatment services but there are certain financial requirements you must meet before Medicare will pay.
Here are the basic costs for Medicare Part B:
- $144.60 premium, if you have one
- $198 deductible
- 20 percent of all Medicare-approved costs during your treatment
- any copayment or coinsurance fees if you receive services at a hospital outpatient clinic
Theres no limit to the frequency or amount of sessions that Medicare will cover for outpatient mental health counseling. However, because there are out-of-pocket costs associated with these services, youll have to review your own financial situation to determine how often you can seek treatment.
If youre looking to begin counseling or therapy appointments under your Medicare plan, here is a list of mental healthcare providers that Medicare approves:
- psychiatrist or doctor
- clinical psychologist, social worker, or nurse specialist
- nurse practitioner or physician assistant
There are many types of mental health specialists that you can visit for help. If youre not sure who to see, talk to your doctor about which specialist may be best for you.
As we age, we become more susceptible to health problems, which can place older adults at a higher risk of mental illnesses like depression.
Does Medicare Cover Mental Health Therapy
Yes, Medicare covers mental health care, which includes counseling or therapy. Depending on your needs, mental health care can be provided in a variety of settings. The goal is to get the right kind of support when you need it.
Mental health pertains to our emotional, psychological, and social well-being. Our mental health can impact how we think, feel, and act. From a holistic, whole-person perspective, mental health plays a big part in our general overall health. Just as Medicare helps cover physical ailments, it also offers various benefits to support emotional, psychological, and social health.
Mental health concerns include anxiety and depression, substance abuse, eating and stress disorders, schizophrenia, and attention-deficit/hyperactivity disorders. These concerns can range from mild to severe and can be addressed on an outpatient or inpatient basis.
You can access mental health benefits through Original Medicare or Medicare Advantage plans, an alternative to Original Medicare. MA plans offer the same services, follow the same Medicare rules as Original Medicare, and generally require in-network providers, referrals, and prior authorization to receive benefits.
Don’t Miss: Do I Really Need A Medicare Supplement
Does Medigap Cover Mental Health Care
Medigap plans can cover some or all of the costs of mental health care, dependent on the Medigap plan you choose. For instance, while many Medigap plans will cover part of your costs, only Medigap plan C and F will cover all mental health service costs by a Medicare approved provider. Medigap C and F will cover your Part A and B deductibles, copays, and coinsurance.
If you were to have one of these plans, you should not have any out of pocket expenses besides your monthly premium -unless you were to go beyond your lifetime care days .
Medicare Part D Coverage
Your doctor may prescribe medications as part of your treatment. Keep in mind that Original Medicare, Part A and Part B, includes only limited prescription drug coverage, although Part B covers certain prescription drugs you get in an outpatient setting, such as medications you cant give yourself. For most other prescription needs, youll need to enroll in a stand-alone Medicare Part D Prescription Drug Plan if you have Original Medicare.
Another option is to sign up for a Medicare Advantage Prescription Drug plan, which includes both health and drug benefits. These plans must provide at least the same level of coverage as Medicare Part A and Part B, but may include additional coverage, including drug benefits, routine vision and dental, and more. You need to continue paying your Medicare Part B premium along with any plan premium. There are only certain times when you can enroll in a Medicare Advantage plan.
Keep in mind that prescription costs may vary by plan, even for the same medications. One way to minimize your costs is to compare plans and find a Medicare Part D Prescription Drug Plan that covers your prescriptions with low cost-sharing. Remember, costs to consider include not only premiums and copayments or coinsurance, but also deductibles and out-of-pocket maximum limits.
To browse plans in your area, simply enter your zip code where indicated on this page.
To learn about Medicare plans you may be eligible for, you can:
You May Like: Are Legal Residents Eligible For Medicare
Does Medicare Cover Couples Therapy
Yes, Medicare provides coverage for couples therapy, but only in certain circumstances. Medicare specifies what type of therapist will receive payment for couples therapy. For example, couples therapy provided by a psychologist or clinical social worker is typically covered by Medicare, however couples therapy provided by a marriage and family therapist is not. Medicare also establishes that couples therapy needs to be part of an individuals treatment plan in order for it to be covered by insurance. That is, that including the clients partner in sessions is helpful for their diagnosable mental health condition.
Because its nuanced who receives coverage for couples therapy, speak with your prospective couples therapist about whether or not they receive Medicare reimbursement for their services. You might also consider calling your Medicare plans customer service hotline to verify.
Medicare And Mental Health Coverage
When a person first enrolls in Medicare, they receive a Welcome to Medicare preventive visit. During this visit, a doctor reviews risks of depression.
Yearly wellness visits can then include discussions with a persons doctor on any changes to mental health that may have occurred since the last visit.
In addition to the wellness visits, Medicare covers certain mental health services both inside and outside of a hospital.
Recommended Reading: Is Medicare Advantage A Good Choice
Where Can I Find Medicare Mental Health Providers
With traditional Medicare, you can see any eligible mental health provider who participates in the program and who accepts assignment, when required. But finding a psychiatrist who accepts Medicare patients can be a challenge. A recent Kaiser Family Foundation analysis found that 60 percent of psychiatrists are accepting new Medicare patients, compared with almost 90 percent of physicians who arent pediatricians, while other psychiatrists and mental health professionals refuse patients paying with Medicare or private insurance.
If you go to a provider who has opted out of Medicare, youll be responsible for the total bill Medicare wont reimburse you. A doctor who has opted out should ask you to sign a contract noting this, but its wise to ask mental health providers if they accept Medicare before youre treated.
To find a psychiatrist or other physician in your area who accepts Medicare, go to Medicares physician compare website. It helps that Medicare relaxed some of its restrictions on using telehealth services during COVID, which has improved access to mental health providers.
Other Parts Of Medicare
Although parts A and B cover most of your mental health needs, you can get additional coverage by enrolling in the following Medicare plans:
- Medicare Part C: automatically covers all Medicare Part A and Part B services, plus prescription drugs and other coverage areas
- Medicare Part D: can help cover some of your mental health medications, including antidepressants, anti-anxiety medications, antipsychotics, mood stabilizers, etc.
- Medigap: can help cover some fees associated with your inpatient or outpatient care such as coinsurance and deductibles
If youre ready to seek mental health treatment, visit the Substance Abuse and Mental Health Services Administrations website to find behavioral health treatment services near you.
Recommended Reading: Does Medicare Pay For Home Health Care For Dementia Patients