Resource Limits For Texas Medicaid
To qualify for Medicaid, you must have few resources. Resources are assets, like money in the bank, retirement accounts, land, and personal property like cars.
The resource limit for a single person to qualify for Texas Medicaid is $2,000, and for a married couple who both want to qualify for Medicaid, it is $3,000.
Some property does not count toward the resource limit. In Texas, the home you live in is excluded from the resource calculation as long as it is worth less than $585,000 . There are other excluded resources, including one car.
Texas Requirements For Medicaid Qualification
Qualification for Medicaid in Texas is more of a formula than a series of check-boxes. You have to meet certain income requirements. But the income limit varies depending on the number of people in the household, and the variety of Medicare for which you are applying.
Here is an example from the Texas HHS website:
- If the monthly income is $1,784 or less, or the yearly income is $21,404 or less, you may qualify for Children’s Medicaid.
- If the monthly income is $2,663 or less, or the yearly income is $31,951 or less, you may qualify for CHIP.
Not to be confused with Childrens Medicaid, CHIP stands for Childrens Health Insurance Program. The above figures only apply to a family of two. For Childrens Medicaid, the limit increases to $4,558 for a family of eight. Even these are not hard limits as there are circumstances where the limits could be higher.
Eligibility groups include, but are not limited to the following:
- Women who are pregnant
- Individuals who receive Supplemental Security Income
- Anyone who currently receives adoptive assistance
- Low-income households that have kids under the age of 19
The only way to truly determine your eligibility is to apply.
How Mepd Services Are Provided
If you’re an adult with a disability and qualify for MEPD, these services are typically provided by STAR+PLUS. You will choose a STAR+PLUS health plan from the ones available in your service area.
If you have a child with a disability who qualifies for MEPD, these services are typically provided by STAR Kids. You will choose a STAR Kids health plan from the ones available in your service area.
You might also be enrolled into traditional Medicaid. Traditional Medicaid just means the state pays your doctors, nurses and other caregivers directly.
Read Also: Does Humana Medicare Cover Incontinence Supplies
Who Is Eligible For Medicaid In Texas
To be eligible for Medicaid in Texas, you must:
- Be a resident of the state of Texas
- Be a U.S. national, citizen, permanent resident, or legal alien
- Need health care/insurance assistance
- Be low or very low income according to Texas
- Be 65 years of age or older or have a disability
If youre eligible for both Medicare and Medicaid, youre likely to be whats called Dual-Eligible.
Medicaid eligibility is tied to income and financial resource levels. Unlike Medicare, with Medicaid, you must recertify with Texas each year to ensure you continue to qualify.
Medically Needy Medicaid Texas
If you dont meet Texas Medicaid eligibility requirements based on your income level, you can still qualify based on spend down. This means that if you spend enough money on health care to put you below the qualifying limit, you can still qualify. However, that money that puts you below the line has to be going towards your healthcare costs.
Recommended Reading: How Do You Qualify For Medicare In Texas
Individual Does Not Have An Mco
Revision 22-1 Effective Nov. 28, 2022
If a LIDDA becomes aware that a person is not assigned an MCO, the LIDDA must contact the NF and request the NF give information and guidance to the person or LAR on how to select and enroll in an MCO. The LIDDA must not delay transition planning activities if the person does not have an MCO and is ready to transition to the community.
Note: As part of medically related social services, a NF may provide information to a person or the persons LAR about available MCOs and guidance on how to enroll in the preferred MCO. A NF may not choose an MCO on behalf of the individual.
People Who Have Both Medicare & Medicaid
People who have both Medicare and full Medicaid coverage are dually eligible. Medicare pays first when youre a dual eligible and you get Medicare-covered services. Medicaid pays last, after Medicare and any other health insurance you have.
You can still pick how you want to get your Medicare coverage: Original Medicare or Medicare Advantage . Check your Medicare coverage options.
If you choose to join a Medicare Advantage Plan, there are special plans for dual eligibles that make it easier for you to get the services you need, include Medicare coverage , and may also cost less, like:
- Special Needs Plans
- Medicare-Medicaid Plans
- Program of All-Inclusive Care for the Elderly plans can help certain people get care outside of a nursing home
Read Also: Does Medicare Pay For Mental Health Therapy
Texas Medicaid Enrollment Numbers
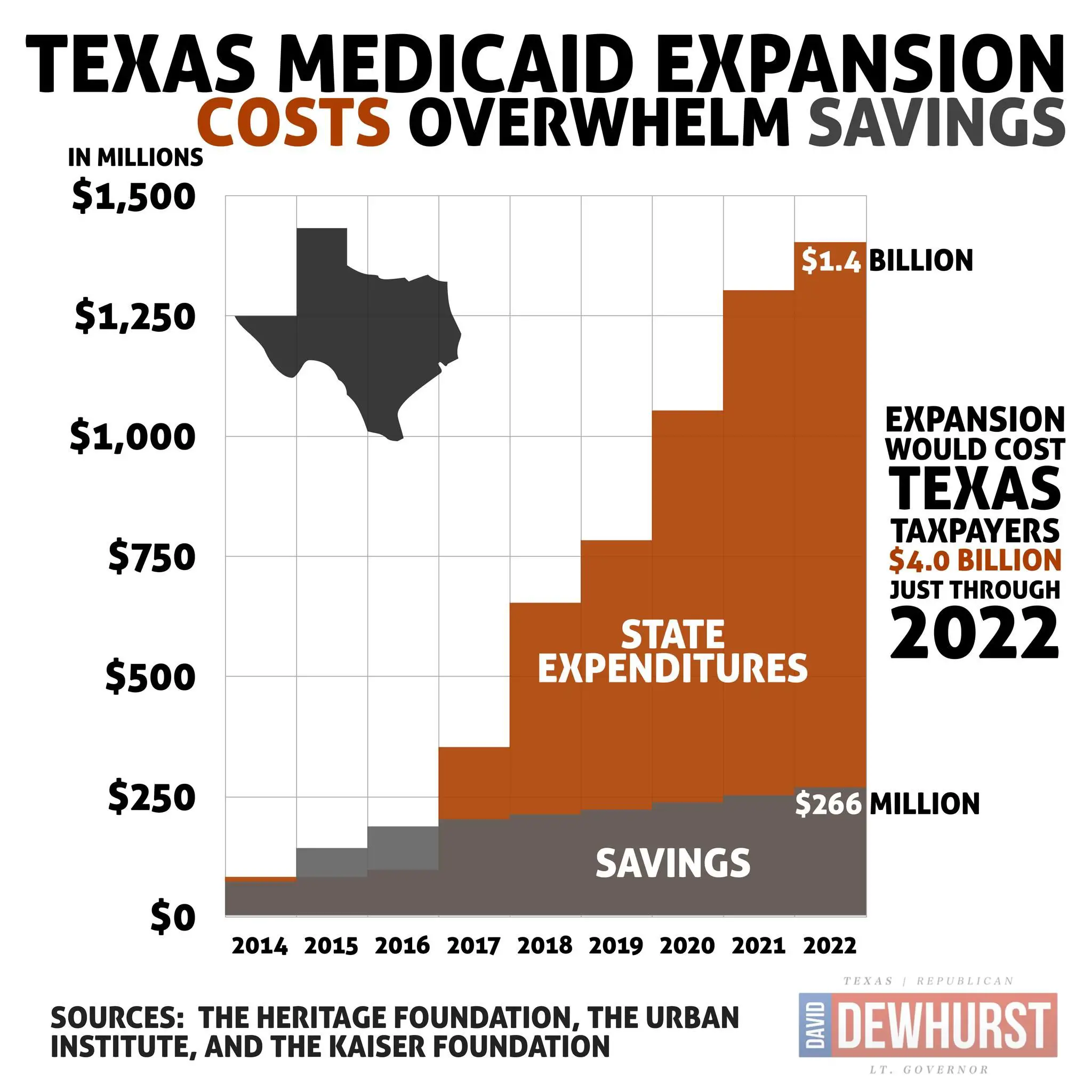
If Texas were to expand Medicaid, its estimated that 1.7 million currently uninsured people would be newly eligible for coverage. Of those people, 771,000 are currently in the coverage gap and have no realistic access to health insurance at all. They dont qualify for Medicaid, but their incomes are under the poverty level which means they are not eligible for subsidies in the exchange.
But despite the fact that the state has opted against using federal funds to expand Texas Medicaid, enrollment in Texas Medicaid/CHIP has grown by 27% more than 1.1 million people since 2013.
Much of that growth is due to the COVID pandemic and the Families First Coronavirus Response Act. That legislation, enacted in March 2020, provides states with additional federal funding but on the condition that nobody be disenrolled from Medicaid until after the COVID public health emergency ends. The PHE has been extended through mid-October 2022, and could be extended again if the COVID situation warrants it.
Once the PHE ends, millions of Americans will have their Medicaid eligibility redetermined and some will lose their coverage as a result.
Prior to 2014, Texas had the highest uninsured rate in the country, and that is still the case. According to U.S. Census data, 22.1% of Texas residents were uninsured in 2013. It stood at 18.4% in 2019, which was still the nations highest uninsured rate.
Can You Have Medicare In Two States
Can You Have Medicare and Dual Residency? You can have Medicare while living in two states, but youll choose one location as your primary residence. There will be some Medicare plans that benefit you more than others when you have multiple homes. Some retired people choose to reside in two different locations.
Also Check: What Are The Enrollment Periods For Medicare
What Are The Income Requirements For Medicaid In Texas
What are the Medicaid application guidelines related to finances? Medicaid income requirements are important to the applicants Medicaid eligibility, since financial assistance is being requested due to low income. The income requirements for Medicaid in Texas vary depending on your Medicaid benefits eligibility group.
Healthy Texas Women Program
Have you lost your Medicaid benefits? The Healthy Texas Women Program provides family planning exams, related health screenings, and birth control to women ages 18 to 44 whose household income is at or below the programs income limits .
You must submit an application to find out if you can get services through this program. Visit this site for more information.
Also Check: What Is The Average Cost Of A Medicare Advantage Plan
Who Is Eligible For Medicare
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease . Medicare has two parts, Part A and Part B . You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if:
- You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
- You are eligible to receive Social Security or Railroad benefits but you have not yet filed for them.
- You or your spouse had Medicare-covered government employment.
To find out if you are eligible and your expected premium, go the Medicare.gov eligibility tool.
If you did not pay Medicare taxes while you worked, and you are age 65 or older and a citizen or permanent resident of the United States, you may be able to buy Part A. If you are under age 65, you can get Part A without having to pay premiums if:
- You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months.
- You are a kidney dialysis or kidney transplant patient.
While most people do not have to pay a premium for Part A, everyone must pay for Part B if they want it. This monthly premium is deducted from your Social Security, Railroad Retirement, or Civil Service Retirement check. If you do not get any of these payments, Medicare sends you a bill for your Part B premium every 3 months.
Can You Use State Health Insurance In Another State
As a general rule: If you live in one state and work in another, you should usually buy health insurance in the state where you live. If you split your time between multiple states, you should buy health insurance in the state where you live most of the year.
Can you use Texas Medicaid in another state?
If a recipient is eligible for Medicaid in another state and receives Medicaid in that state, the person is not eligible for Medicaid from the state of Texas. If a person is placed in an institution located in Texas by an agency of another state, the person remains a resident of the state that made the placement.
Also Check: What Cpap Supplies Are Covered By Medicare
Individual And Family Plans
UnitedHealthcare is offering individual and family plans in Texas that are designed to provide the best possible coverage at an affordable price.
We have plan choices in all three metal levels, bronze, silver and gold, offering a variety of benefits. With most plans, you get:
- $0 virtual care with a doctor who’s specially trained to provide online urgent, specialty and primary care
- Prescriptions as low as $3 Pay for Tier 1 generic drugs at Walgreens
- Member-only discounts, like 20% off Walgreens-brand health and wellness products
- Digital fitness classes at no extra cost
- Access to a library with thousands of live and on-demand digital fitness classes
Hipp And Other Medicaid Programs
If your child gets another Medicaid program, you should check with HIPP about the rules to see if your child can be in both programs. You can learn more about Medicaid health benefits programs and services on our Medicaid page.
If your child or anyone else in your family receives health care benefits or coverage through another program like STAR, STAR+PLUS, or the Childrens Health Insurance Program , you should call HIPP at to see if getting HIPP would cause any problems with those other programs.
Read Also: Does Medicare And Medicaid Cover Dentures
How Much Does It Cost
Your cost is based on:
- Your income. We may not count all your earnings. We will take out amounts we don’t have to count. After that, if you still have more than $1,562, you will have to pay a monthly fee.
- Any other money you get above $771. Examples of other money are Social Security benefits, retirement checks and money from rental property.
Who Is Exempt From Using The New Mbis
Nobody is truly exempt from using MBIs, but there are a few scenarios in which it might be acceptable to use an HICN in place of an MBI. Some of these exceptions include:
- Medicare appeals: When you file an appeal, you can choose whether to use an MBI or an HICN.
- Checking the status of a claim: If you filed a claim before January 1, 2020, you can use an HICN to check the status of a claim. If you filed it after that date, youll have to use the MBI.
- Span-date claims: Some providers submit single claims for services that span multiple days. These might include instances of inpatient treatment or home health. If the services rendered concluded before December 31, 2019, you may submit a claim using the HICN or the MBI.
Recommended Reading: Do You Have To Reapply For Medicaid Every Year
Also Check: Do We Have To Pay For Medicare
Medicare Eligibility In Texas
If youre a Texan and meet the following criteria, you are eligible for Medicare in Texas.
- Youre aged 65 or older.
- Youre younger than 65 with eligible disabilities by the Social Security Administration.
- You have End-Stage Renal Disease or Amyotrophic Lateral Sclerosis .
If you meet the above criteria, then you can apply for Medicare in Texas. Now, youll want to learn more about your public and private Medicare plan optionsand choose a plan that meets your health and budget needs.
Not sure where to begin? Have a local Medicare agent guide you through your Medicare options. A local Connie Health agent can help you find the optimal plan. Call to speak with a local licensed agent or find your plan online.
Agent tip:
Medicare does not typically cover assisted living or long-term care. You will still need Medicare to cover doctor services and hospital care even if you move to an assisted living or nursing home care facility. Family members may pay out-of-pocket to cover the costs or get long-term care insurance to pay for the cost of assisted living or nursing home care.
Original Medicare And Private Medicare Plan Options
Texans have both public and private Medicare plan options. Original Medicare includes Medicare Part A and Medicare Part B . Original Medicare does not cover 100% of costs, and most people have a private health plan such as Medicare Part C, Medicare Part D, or Medicare Supplement.
Medicare Part C , Medicare Part D , and Medicare Supplement are your private health plan options. These are approved by the Centers for Medicare and Medicaid Services .
Learn more about your public and private Medicare plan options in Medicare in Texas.
Find the right Medicare plan for you
Also Check: Does Medicare Cover Chronic Pain Management
How Do I Apply For Medicaid In Texas
Medicaid benefits could help you pay for your Part A and/or B premiums, copays, and deductibles. It could also help you or a loved one afford additional care, like long-term care. Gather benefit information, and ensure that you meet all of the eligibility requirements for the program youre interested in applying for.
If your income or assets are over the limits or youre unsure if you meet the eligibility criteria, a local Medicare agent can help. A local agent can guide you through your Medicaid eligibility and application options. Theyll help you understand your options and the optimal dual-eligible plan for your health and budgetif youre eligible.
Want to apply for Medicaid on your own?
- Complete an Application for Benefits: Texas Health and Human Services Commission. This is a link to the PDF version that you can complete and then physically mail or fax.
- Apply for benefits online through Your Texas Benefits.
Receive help applying for Medicare and/or Medicaid. Be confident that youre on the optimal plan for your health needs and budget. Call or find your plan online.
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays, and restrictions may apply. For more information, call UnitedHealthcare Connected Member Services or read the UnitedHealthcare Connected Member Handbook. Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year.
You May Like: What Does Part B Cover Under Medicare
Responsibility To Reestablish Medicaid Eligibility
Revision 22-1 Effective Nov. 28, 2022
If a person loses Medicaid eligibility or is delayed in having Medicaid eligibility determined or re-determined, a NF and LIDDA may be unable to receive authorizations or bill for PASRR specialized services, including habilitation coordination. It is the responsibility of the representative payee to contact the appropriate entity to determine the necessary action to reinstate benefits.
If the individual or family is the representative payee, the habilitation coordinator must assist, if requested.
If the NF is the representative payee, the NF is responsible for ensuring action is taken to reestablish Medicaid eligibility. In most circumstances, assisting people with Medicaid eligibility determinations, re-determinations, and MCO selection is allowable as a medically related social service, which is a service provided by the NF that help the individual in attaining the highest practicable physical, mental, or psychosocial well-being.
If needed, the LIDDA is expected to work with the NF to help a person reestablish Medicaid eligibility. Failure of a representative payee to help reestablish Medicaid eligibility may be reported to HHSC Complaint and Incident Intake.
To minimize billing issues about habilitation coordination, LIDDAs should review the service authorization in Medicaid Eligibility Service Authorization Verification to verify that the person is admitted into the correct Medicaid program.
