What Part Of Medicare Pays For Prolia
For those who meet the criteria prescribed above, Medicare Part B covers Prolia. If you don’t meet the above criteria, your Medicare Part D plan may cover the drug. GoodRx reports that 98% of surveyed Medicare prescription plans cover the drug as of October 2021. With Medicare Part D coverage, youre likely to pay coinsurance or a copay.
Medicare Prescription Drug Plans
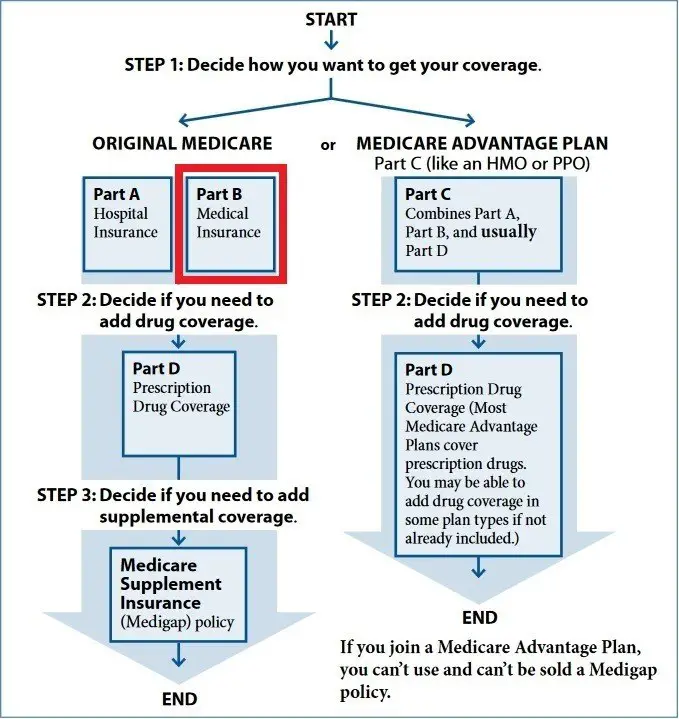
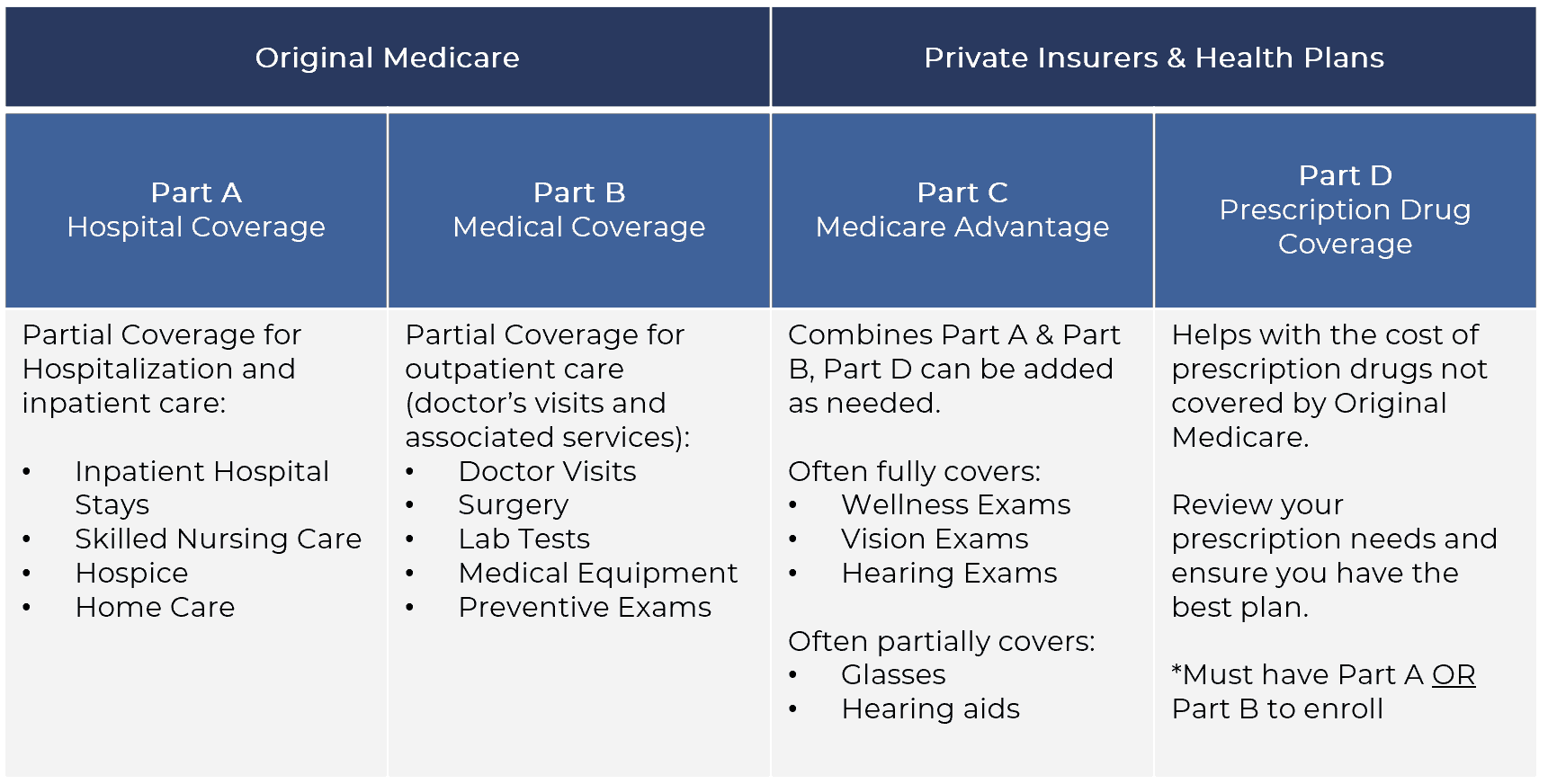
Original Medicare, Part A and Part B, does not include most prescription drug coverage. Medicare Part A may cover prescription drugs you receive as a hospital inpatient, while Medicare Part B covers certain prescription drugs administered to you as an outpatient often drugs you wouldnt take on your own, such as infusions. For coverage of most medications you take at home, you can enroll in a Medicare Prescription Drug Plan from a private, Medicare-approved insurance company. You can get this coverage in two different ways:
- A stand-alone Medicare Part D Prescription Drug Plan, which works alongside your Original Medicare coverage.
- A Medicare Advantage Prescription Drug plan, which includes all the same benefits as Medicare Part A and Part B , as well as prescription drug coverage, and may include other benefits, such as routine vision care.
Every Medicare Prescription Drug Plan maintains its own formulary, or list of covered drugs. Formularies are organized in tiers, or levels, with lower-numbered tiers generally including lower-priced drugs and higher tiers including more expensive drugs. Lower tiers often include generic drugs. A plans formulary may change at any time. You will receive notice from your plan when necessary.
Find Plans in your area instantly!
Does Medicare Pay For Prescription Drugs
When becoming eligible for Medicare, many Medicare beneficiaries make the mistake of thinking they automatically get prescription drug coverage. This is not the case. Original Medicare does not cover prescription drugs. If you want prescription drug coverage, you must join a plan run by an insurance company or other private company approved by Medicare. Medicare recipients can get prescription drug coverage one of two ways:
Medicare Advantage Plan : Medicare Advantage plans not only provide all of the same coverage as Medicare Part A and Medicare Part B , they also generally offer additional benefits, such as vision, dental, and hearing, and prescription drug coverage. Medicare Advantage Plans that include prescription drug coverage are sometimes called MA-PDs and may include an amount for drug coverage in the monthly premium.
This all-in-one coverage can combine your hospital, medical, and prescription drug coverage into one plan. Therefore, you would use one single Medicare card from the insurance provider instead of the red, white, and blue Original Medicare card.
Compare Medicare Advantage Plans with prescription drug coverage that contract with Medicare.org here.
You cannot have both a Part D Plan and a Medicare Advantage Plan. If you join a Part D plan, your Medicare Advantage Plan will disenroll you and youll return to Original Medicare.
Compare Prescription Drug Plans that contract with Medicare.org here.
Read Also: What Is Blue Cross Blue Shield Medicare Advantage
Request A Formulary Exception
If you or your physician believe that the non-covered medication would be the most effective for treating your condition, the next thing you can do is to request a formulary exception. A formulary is a list of prescription drugs covered by the Medicare plan. Every Medicare Prescription Drug Plan and Medicare Advantage Prescription Drug plan has one, although the specific medications included by each plans formulary will vary. Formularies may change at any time youll be notified by your Medicare plan if necessary.
A formulary exception can be granted if your doctor and/or Medicare plan determines that the prescription drug you requested is medically necessary for your health, so you will need a written statement from your doctor or health-care provider to support your case. Once your Medicare plan has received the statement from the prescribing physician, it will make a determination whether or not to cover the non-formulary medication. For a standard formulary exception request, your plan will make its decision and notify you within 72 hours of receiving the prescribing doctors statement.
If waiting 72 hours for a decision could endanger your health, you also have the right to ask for an expedited formulary exception request. If you submit an expedited request, your Medicare plan must respond within 24 hours with its decision.
How Does A Tiered Formulary Work
Many plans have a tiered formulary where the plan’s list of drugs are divided into groups based on cost. In general, drugs in low tiers cost less than drugs in high tiers. Additionally, plans may charge a deductible for certain drug tiers and not for others, or the deductible amount may differ based on the tier.
Formulary tiers:
Read Also: What Does Original Medicare Mean
Are You Looking For Free Insurance Quotes
Secured with SHA-256 Encryption
|
D. Gilson is a writer and author of essays, poetry, and scholarship that explore the relationship between popular culture, literature, sexuality, and memoir. His latest book is Jesus Freak, with Will Stockton, part of Bloomsburys 33 1/3 Series. His other books include I Will Say This Exactly One Time and Crush. His first chapbook, Catch & Release, won the 2012 Robin Becker Prize from Seve… |
Cutting Part B Reimbursement
Medicare pays for medications administered in the healthcare provider’s office a bit differently than the ones you get from the pharmacy. Your practitioner purchases these medications in advance. Because their office is responsible for storing these medications and preparing them for use, medical professionals are paid 6% above the wholesale acquisition cost of the drug. They are paid separately to actually administer the medication.
Concerns have been raised that some healthcare providers may have been abusing the system, ordering the most expensive drugs in order to make a profit. Because patients are still required to pay 20% of the treatment cost, this also increases out-of-pocket expenses for patients.
Medications covered by the Centers for Medicare and Medicaid Services are paid at a 6% rate, while there’s a 3% add-on cost for new prescription drugs.
Don’t Miss: What You Need To Know About Signing Up For Medicare
Does Medicare Advantages Include Vision Test
Medicare Part B includes coverage for diagnostic and preventive vision examinations as well as United healthcare vision benefits. If you prefer to go with the original vision insurance program, then there is coverage for vision tests for once.
As the original Medicare coverage doesnt have support for vision, people who wish to enjoy the maximum benefits of the federal insurance program are advised to become a member of the UnitedHealthMedicareAdvantage program which also incorporates vision examination within the United Healthcare hospitals.
If you wish to know more about the United Healthcare Medicare prescriptions which are available for the general public, then you need to talk with the authorized person who will be able to provide you with more genuine and accurate information regarding the UnitedHealthMedicareAdvantages and United Healthcare Medicare prescriptions.
What Is The United Healthcare Medicare Phone Number
For those in search of the United Healthcare Medicare phone number, also known as the MyAARPMedicare phone number, then you need to dial the number of United Healthcare vision providers phone number, which is 1877-889-6358.
In case the above-mentioned number is not working for you, then you can try the alternative United Healthcare Medicare Phone Number of 1877-842-3210.
Final Words
We believe that the above article contained enough information about does Medicare cover vision and the Medicare vision coverage benefits. In case you have any doubts about the United Healthcare Medicare advantages or MyAARPMedicare advantages, feel free to get in touch with us by leaving a comment below.
Don’t Miss: Why Sign Up For Medicare At 65
How Parts B And D Work Together
Medicare Parts B and D pay for medications you receive in the ambulatory setting but they won’t pay towards the same prescription. You can only turn to one part of Medicare or the other. However, you may be able to use them both for drugs you receive in a hospital setting.
Medications you receive in the hospital when you are admitted as an inpatient will be covered by your Part A deductible. It is important to understand what happens when you are evaluated in the emergency room and sent home or are placed under observation, even if you stay overnight in the hospital. In this case, you can turn to Parts B and D to pay for your drugs.
When you are placed under observation, Part B will still pay for the medications reviewed above. If you receive IV medications, these will generally be covered. However, you may also receive oral medications during your observation stay that are not on the Part B list of approved medications. In this case, you will be billed for each pill administered by the hospital.
Send copies of your hospital bills to your Part D plan for reimbursement. Unfortunately, if you receive a medication that is on your Part D formulary, your plan may not pay for it.
Paying For Your Prescription Drugs
If you prefer to remain with the same Medicare Part D Prescription Drug Plan or Medicare Advantage Prescription Drug plan and your request for a formulary exception was denied, you may have to pay full price for your prescription drug, instead of the usual copayment or coinsurance. Choosing a generic medication instead of a brand-name prescription drug may be your best option if your doctor decides that could work for your health condition.
Some prescription drug manufacturers offer payment assistance programs, especially for newer or expensive medications. You would need to contact the prescription drug manufacturer on your own to explore this possibility.
Do you have questions about your options if your Medicare plan doesnt cover a medication you need? If youd like assistance finding Medicare Part D coverage that may cover your prescription drugs, feel free to contact eHealth to speak with a licensed insurance agent. Were here to help.
This website and its contents are for informational purposes only. Nothing on the website should ever be used as a substitute for professional medical advice. You should always consult with your medical provider regarding diagnosis or treatment for a health condition, including decisions about the correct medication for your condition, as well as prior to undertaking any specific exercise or dietary routine.
New To Medicare?
Also Check: Does Medicare Cover Dexa Scan
D Appeals And Grievances
Coverage Determinations and Exceptions
All Part D plans must have an appeal process through which members can challenge a denial of drug coverage. The Part D appeals process is based on and similar to the Part C appeals process.
Denials of drug coverage by a PDP or MA-PD are called coverage determinations. For example, a coverage determination may be issued by the plan if the drug is not considered medically necessary or if the drug was obtained from a non-network pharmacy. It is necessary to have a coverage determination in order to initiate an appeal. A doctors supporting statement is not required for this type of appeal, but it may be helpful to submit one. If the request for coverage is denied, the member may proceed to further levels of appeal, including redetermination by the plan, reconsideration by an Independent Review Entity , Administrative Law Judge review, the Medicare Appeals Council , or federal district court.
One type of coverage determination is called an exception request. An exception request is a coverage determination that requires a medical statement of support in order to proceed to appeal. There are two types of exceptions that may be requested:
Formulary Exceptions This type of exception is requested because the member:
- needs a drug that is not on the plans formulary,
- requests to have a utilization management requirement waived for a formulary drug).
What to do When a Drug is Denied at the Pharmacy
The Medical Statement
Grievances
What Is The Alternative To Taking Prolia

The FDA has approved another brand-name version of denosumab, called Xgeva. Your Medicare Part D plan might not cover the medication. If it does, your out-of-pocket price for Xgeva injections may cost more or less than Prolia, depending on where the drugs are classified on the formulary.
Instead of Prolia, doctors may prescribe other drugs for people at risk of suffering fractures due to osteoporosis, such as:
- Bisphosphonates like alendronate, ibandronate, risedronate and zoledronic acid
- Bone-building medications like teriparatide, abaloparatide and romosozumab
- Hormone-related therapy like raloxifene
Read Also: Does Kelsey Seybold Accept Medicare
How To Get Prescription Drug Coverage
Medicare drug coverage helps pay for prescription drugs you need. Even if you dont take prescription drugs now, you should consider getting Medicare drug coverage. Medicare drug coverage is optional and is offered to everyone with Medicare. If you decide not to get it when youre first eligible, and you dont have other creditable prescription drug coverage or get Extra Help, youll likely pay a late enrollment penalty if you join a plan later. Generally, youll pay this penalty for as long as you have Medicare drug coverage. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage. Each plan can vary in cost and specific drugs covered.
How Much Does Prolia Cost Per Year
The list price for one dose of Prolia was around $1,300 as of October 2021, according to Amgen, the manufacturer of the drug. Most people get one Prolia injection every six months, making the average cost for one year of treatment with no insurance or Medicare coverage around $2,600. You may pay more or less depending on where you live and choose to fill your prescriptions.
Recommended Reading: Is Sonobello Covered By Medicare
Medical Equipment Used To Administer Medications
- Infusion pumps
- Nebulizer machines
* Oral chemotherapy and anti-nausea agents have to meet certain criteria to be covered by Part B. While the majority of injectable medications will be covered by Part B, keep in mind that some drugs may be excluded. The coverage requirements change on an annual basis.
** Hepatitis B risk factors for the purpose of Part B coverage include diabetes mellitus, ESRD, hemophilia, living with someone who has Hepatitis B, or being a healthcare worker who could be exposed to blood or other bodily fluid.
There Are 2 Ways To Get Medicare Drug Coverage:
1. Medicare drug plans. These plans add drug coverage to Original Medicare, some Medicare Cost Plans, some Private FeeforService plans, and Medical Savings Account plans. You must have
and/or
to join a separate Medicare drug plan.
or other
with drug coverage. You get all of your Part A, Part B, and drug coverage, through these plans. Remember, you must have Part A and Part B to join a Medicare Advantage Plan, and not all of these plans offer drug coverage.
To join a Medicare drug plan, Medicare Advantage Plan, or other Medicare health plan with drug coverage, you must be a United States citizen or lawfully present in the United States.
Visit Medicare.gov/plan-compare to get specific Medicare drug plan and Medicare Advantage Plan costs, and call the plans youre interested in to get more details. For help comparing plan costs, contact your State Health Insurance Assistance Program .
Don’t Miss: Does Medicare Part B Cover Prolia Shots
What Should I Know About A Plan’s Drug List
Medicare Part D and Medicare Advantage plans have a drug list that tells you what drugs are covered by a plan. Medicare sets standards for the types of drugs Part D plans must cover, but each plan chooses the specific brand name and generic drugs to include on its formulary. Here are some important things to know:
- A plan’s drug list can change from year to year.
- Plans can choose to add or remove drugs from their drug list each year. The list can also change for other reasons. For example, if a drug is taken off the market. Your plan will let you know if there’s a coverage change to a drug you’re taking.
- Many Part D plans have a tiered formulary.
Medicare Part D Penalty For Late Enrollment
All eligible Medicare beneficiaries have a seven-month Initial Enrollment Period when they can enroll in Medicare Part A and/or Part B, as well as sign up for a Medicare Advantage Plan and/or a Medicare Prescription Drug Plan . The IEP starts 3 months before you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65.
If you enroll in a Medicare Prescription Drug Plan after your Initial Enrollment Period , you may have to pay a late-enrollment penalty.
According to Medicare.gov, the cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage.
Medicare calculates the penalty by multiplying 1 percent of the national base beneficiary premium times the number of full, uncovered months you didnt have Part D or creditable coverage. The monthly premium is rounded to the nearest $.10 and added to your monthly Part D premium. The national base beneficiary premium may increase each year, so your penalty amount may also increase each year.
Also Check: Is Blood Pressure Monitor Covered By Medicare
What Is Extra Help And Who Is Eligible
You may be eligible for lower premiums, deductibles and coinsurance through Medicares Extra Help program. In 2022, those enrolled in the program pay $3.95 for each generic and $9.85 for each brand name drug.
In 2021, you may qualify if your income is up to $19,320 for an individual and $26,130 for a couple and you have a limited amount of resources such as savings, stocks and bonds. If your income or resources change, you can apply for Extra Help at any time.14
The Medicare Catastrophic Coverage Act Of 1988
The Medicare Catastrophic Coverage Act of 1988 began with the 1984 report of the Social Security Advisory Council chaired by Otis Bowen, a physician and former Republican governor of Indiana. The council’s report did not focus on prescription drugs but on the limited hospital coverage provided by Medicare and the out-of-pocket expenses for both hospital and physician services. After Bowen was appointed as secretary of HHS by President Ronald Reagan in November 1985, he urged the White House to support the council’s reform proposals and successfully lobbied for an initial proposal in the 1986 State of the Union address. The combination of Bowen’s interest and changes in the political climatethe Iran/contra scandal in the White House and Democrats regain of control of the Senate after the 1986 election, along with their continuing control of the House of Representativessoon created the opportunity for new Medicare benefits, among them prescription drug coverage .
In the spring of 1988 the chairman of the Senate Finance Committee, Lloyd Bentsen , proved to be the final arbiter when he accepted a drug benefit scaled back to catastrophic coverage and not a routine benefit. Medicare would cover 80 percent of drug costs once the beneficiary met a $600 deductible. The administration, weakened by scandal, did not have the will to fight over prescription drugs, and it ultimately supported the final package .
Recommended Reading: Can I Change My Medicare Advantage Plan Now
