When Will Medicare Pay For A Caregiver
For the most part, whether Medicare will cover in-home caregivers depends on exactly what type of care one is receiving. Keep in mind that to remain eligible for Medicare at-home medical care coverage, you will need to see your doctor fewer than 90 days before, or 30 days after, you begin to receive home healthcare services.
In the following scenarios, Medicare benefits may apply:
Whether Medicare Pays For A Caregiver Comes Down To The Level And Type Of Care You Need
The short answer here is: Medicare will sometimes pay for a caregiver. You or a loved one may need a caregiver for a wide variety of home care needs, and Medicare will only pay for a caregiver under a very limited selection of these. The basic idea to remember is that Medicare will pay for your caregiver if their care is part of an overall medical rehabilitation strategy, rather than if it is just general care and help in the home.
This is spelled out in various specific requirements that you should be knowledgeable about.
Donât Miss: How To Reorder Medicare Card
What Is Home Health
Home health provides skilled services, including nursing care and physical, occupational, speech and respiratory therapy. The agency will send a licensed professional to assess home health needs and develop a complete care plan. These services are usually short-term, as in the case of a person recovering from surgery or other health issues.
Medicare will cover home health if it is ordered by a physician and the person is homebound and in need of skilled services.
A home health care agency employs the healthcare professionals sent to the home and must be licensed by the state. Many seek additional accreditation to assure consumers that they have met quality standards. Common accreditations are the Community Health Accreditation Program , Accreditation Commission for Health Care and The Joint Commission .
You May Like: Will Medicare Pay For Dental Care
Recommended Reading: How Do I Get A Medicare Explanation Of Benefits
How Much Does Medicare Cover For Home Health Care
If your client has original Medicare, they dont pay anything for home health services although they will be liable for a co-pay of 20% of the Medicare-approved amount for durable medical equipment .
Before starting with home health care, you, as the agency, will need to advise your client what costs will be incurred and which are covered by Medicare. Youll also need to inform them of any services that arent covered by Medicare. This should be communicated in-person and in writing and youll also need to provide them with an Advance Beneficiary Notice before any non-Medicare services are provided.
In some states you may submit a pre-claim review request to Medicare. This helps you and the client determine whether Medicare is likely to cover the services.
The specific amount a client will owe for non-Medicare covered services will depend on:
- Any other medical insurance they have
- Their doctors rates
- If their doctor accepts assignment
- The type of treatment facility
- Where they get their tests or services.
In some cases, your clients doctor may recommend a treatment plan that requires more regular treatments than are covered by Medicare, or they may recommend services that arent covered. If this happens, the client will be liable for the costs.
Families Are Quite Distressed When They Discover That Medicare Will Not Pay For A Home Caregiver

Families are often surprised if not dumbfounded to learn that Medicare does not pay for most in-home care for their elderly parents. Medicare will not reimburse in-home caregivers to assist aging loved ones with basic activities of daily living such as personal care, meal preparation, transportation, medication reminders and housekeeping. In-homecare often referred to as custodial care is not covered by Medicare in spite of the dire need of these services by countless seniors. Furthermore it is exactly these non-medical homecare services that enable seniors to remain safely in their homes and age with dignity. Home care that is considered non-medical in nature is sadly not an allowable expense covered by our national Medicare program. Whether it is part-time, fulltime, or even live-in homecare the answer is still a resounding NO when it comes to Medicare reimbursement. Numerous families understandably are quite distressed when they unexpectedly discover that Medicare will not pay for in-home care to support their aging parents.
About the Author
Clare Absher is a Registered Nurse with 43 years of experience. Most of her experience is in home health serving as a caregiver, educator, patient advocate, and liaison between families and community resources. She has also worked in acute care, assisted living, and retirement settings. She is passionate about helping families care for their elderly loved ones at home.
You May Like: How Do I Get A Second Opinion With Medicare
Who Is Eligible For In
In order to access the available home health care services, your client will need to have Medicare Part A and/or Part B. In addition, they need to meet the following conditions:
- They must be under the care of a registered doctor, and their case must be reviewed regularly by their doctor.
- Their doctor must certify that they need skilled nursing care or therapy.
- They must require physical, occupational, or speech therapy for a limited period of time.
- They must be housebound, meaning that they are unable to leave home without considerable effort or support.
- They must have certification from a doctor that theyre housebound following a documented encounter with their doctor no more than 90 days before or 30 days after their home health care starts.
- They are under an established plan of care from their doctor that is reviewed regularly and includes what services are needed, how often they are needed, who will provide them, what supplies are required, and what results are expected.
- They must only require part-time skilled nursing .
- You, as the home health agency providing care, must be Medicare certified.
A client will not be eligible for home health benefits if they require more than intermittent skilled nursing care. However, they may leave their home for medical treatment for short outings such as religious services. Your client will still be eligible if they attend adult daycare.
For more on who qualifies for services, have a look at Medicares website.
Through Your Local Area Agency On Aging
Your local Area Agency on Aging may be able to provide more detailed information on whether your states medicaid program will pay a family member to provide care to a Medicaid recipient.
In addition, your Area Agency on Aging will usually have additional information on federally-supported programs that aim to help ease the financial burden that caregiving can place on families.
Recommended Reading: How Does Medicare Work With Employer Insurance
How Much Will I Have To Pay If I Qualify
With Original Medicare coverage , eligible seniors will pay nothing for home health care services that are ordered by a doctor and provided by a certified home health agency. Any additional services provided outside of the approved care plan will not be covered and must be paid for out of pocket.
Be aware that before services begin, the home health agency should provide an itemized receipt or plan of care that identifies what is eligible for Medicare coverage and what is not. A written notice called the Advance Beneficiary Notice of Noncoverage will detail any services and durable medical equipment that Medicare will not pay for as well as the costs the patient will be responsible for.
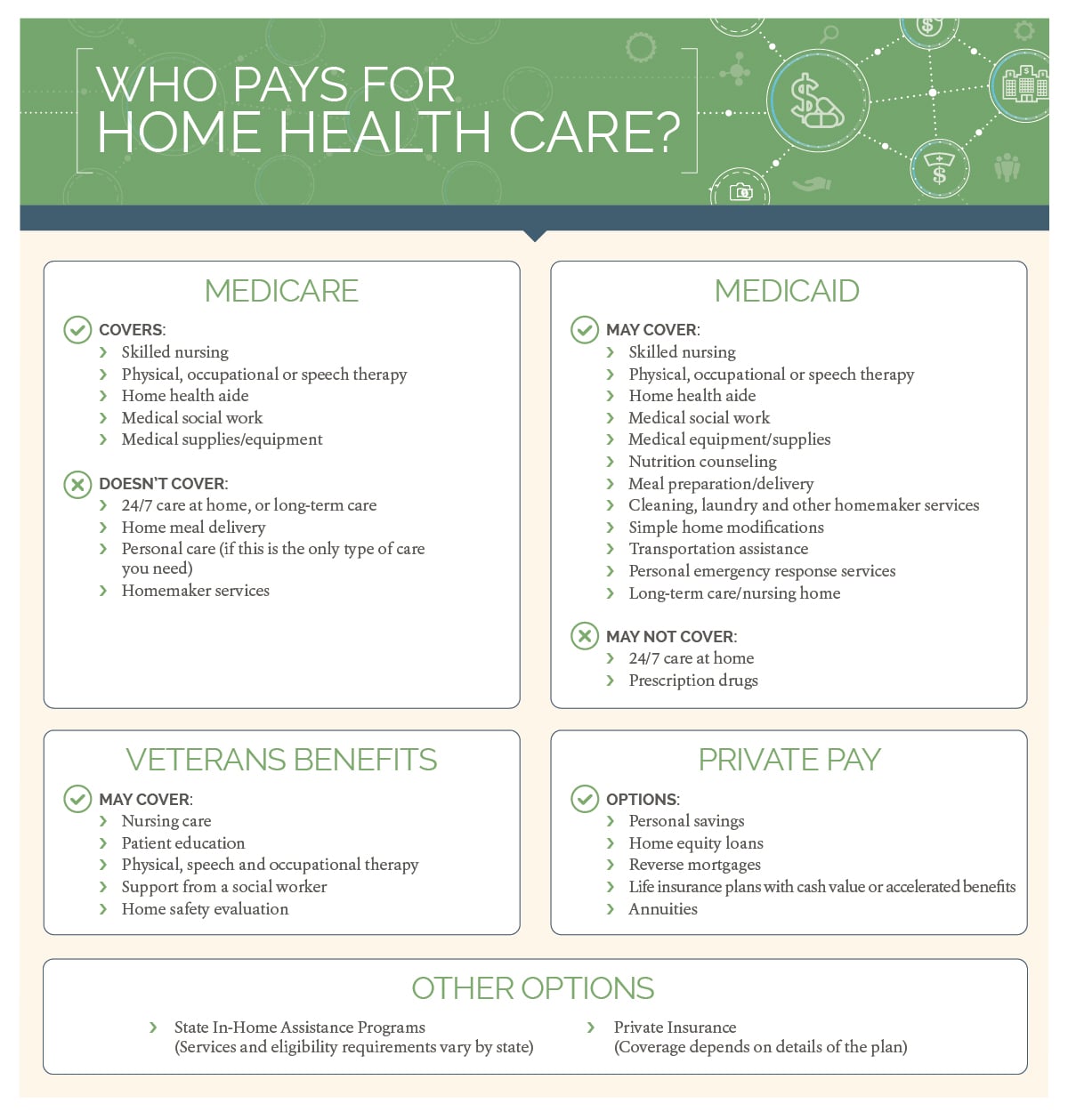
Use the guide below to determine the combination of payment options that will help your family cover home care costs.
V Frequently Asked Questions
What is the difference between home health and home care?
The difference between home care and home health care is that home health care involves skilled nursing care from trained medical professionals. On the other hand, standard home care focuses on companion care, personal care and assistance with ADLs, and household assistance. Standard home care aides do not need any nursing or medical certification, while home health aides do.
Will Medicare pay for in-home care for the elderly?
Medicare will pay for in-home care for the elderly under certain circumstances. In general only home health care, not personal or companion care, is covered. Home health care includes skilled nursing care, therapy services, and other medical services. If you need personal care and home health care and receive them both from the same Medicare-approved provider, in-home personal care should be covered.
What home health care is covered by Medicare?
Medicare covers several home health care services, including intermittent skilled nursing care , therapy services like physical and occupational therapy, and medical social services. Medicare does not cover companion care, transportation, and meal delivery.
How much does home care cost?
According to Genworth Financial, home care costs an average of $25 an hour for personal or companion care and $26 an hour for home health care. This comes out to an average of $4,481 and $4,576 per month, respectively, for 44 hours of care per week.
Also Check: How Do I Check On My Medicare Application
What Medicare May Cover
People who are homebound and under a doctors care may be eligible for certain home health services.
Home health care includes services like skilled nursing care, physical therapy, speech-language pathology services and continued occupational services.
Here are the most frequent scenarios:
Short-term care for conditions that will improve
Medicare may pay for some short-term home health care or a nursing home stay following medical treatment from which the patient is expected to recover.
To qualify, the patient must have:
- recently stayed in hospital for at least three days
- entered into Medicare-approved care within 30 days of this hospital stay
- a doctor certified requirement for some kind of skilled care such as physical therapy or skilled nursingIf the patient meets all three criteria, Medicare will pay for 100 percent of the care for 20 days and a portion of the total amount from day 21 to day 100. After 100 days, the patient is responsible for all expenses.
Doctor-prescribed care for recovery from an injury
Medicare may also cover additional care, provided your doctor says it is medically necessary to recover from an injury. This may include:
- Physical therapy
- Prescription drugs
- Hospice aide or homemaker services
- Grief counselling for the patient and his or her family
- Social work services
- Short-term in-patient care for pain and symptom management
- Short-term in-patient or in home respite care, to allow caregivers time away from caring responsibilities
Why Choose Home Care
The goal of home care is to help each person regain their independence and heal from their illness/injury so they can be as self-sufficient as possible.
Many of the services provided to a person at home will be the same services or treatments that are provided at a hospital.
The benefit to home care is that these services are usually less expensive to be provided in someones home and they are much more convenient as you can schedule the appointments when it works for your schedule, plus its in your home where you will feel so much more comfortable than in a hospital.
You might like to read: Home Care for Seniors The Complete Guide
You May Like: Does Medicare Pay For Counseling For Depression
What Are Some Other Professional Caregiver Services That May Be Covered Under Medicare
Medicare does not typically cover caregivers who are solely responsible for custodial care needs, such as dressing, personal hygiene, restroom assistance, meal prep and delivery, and daily living, unless these services are provided short-term and by professionals approved by Medicare.
Typically, Medicare will not pay for 24-hour in-home care, full-time skilled nursing care, or transportation, unless these services are covered under your specific Medicare Advantage plan. If you have additional questions or concerns about assistance for caregivers under Medicare, for additional information and resources.
For professional assistance with researching and comparing Medicare Advantage plans in your area, reach out to MedicareInsurance.com today via our online chat feature, or by phone at 950-0608. Our friendly and professional agents are fully licensed and are ready and willing to help.
Personalized Home Care Services
Vibrant Health Home Care serves clients throughout Tacoma, Lakewood, Fife, Fircrest, Parkland, Steilacoom, Graham, Puyallup, Spanaway, Gig Harbor, University Place, Dupont, and the surrounding cities.
If you need our services, we will work closely with you and your doctor to set up a custom care plan, while considering all the services, treatments, and equipment you need. Contact us online for a detailed insight into our in-home care options. Or call us at we are always a phone call away!
You May Like: Can Someone On Ssi Get Medicare
Can I Get Paid To Care For A Family Member
We receive hundreds of calls every year from family and friends asking, âHow can I get paid to care?â These caregivers arenât asking for a handout, they are simply trying to find a way to make ends meet while dedicating their time to caregiving. Unfortunately, very few programs pay family members or friends on a regular basis to provide care. Medicare does not pay for long-term care services, such as in-home care and adult day services, whether or not such services are provided by a direct care worker or a family member. Sometimes, however, caregiving families may obtain financial relief for specific purposes, such as for respite care or to purchase goods and services, and in some cases, pay for caregiving. In some states there are programs that pay family members to provide care to those receiving Medicaid . And in a very few states there are programs available to those who do not qualify for Medicaid. NOTE: These programs vary widely, often with complicated criteria for eligibility.
Steps to Consider:
Additional Resources:
Join FCA CareNav, a secure online service for quality information, support, and resources tailored to your caregiving situation.
Benefits Checkupwww.benefitscheckup.org
Eldercare Locatoreldercare.acl.gov
What Does Medicare Cover For Home Health Care In The Us
If youre looking for an answer to the question, what does Medicare cover for home health care in America?, youve probably typed it into google and immediately closed the tab. The volume of information and the level of detail can quickly become confusing and overwhelming .
Weve broken this important query down into a series of frequently asked questions, looking at what home health services can be offered by a home health agency, what services arent covered, and who is eligible.
If youre a health professional exploring the idea of establishing a home health agency or are trying to determine which services you can and cant offer, this article will help.
Don’t Miss: Are Hearing Aids Covered By Medicare Part B
What Should Caregivers Know About Medicare
Medicare is a federal government health insurance program primarily for people age 65 and older. It may also cover younger adults with disabilities.
There are different plans and coverage options within Medicare.
Your loved one or family member may be enrolled in Original Medicare, which includes two components: Part A for hospital insurance and Part B for medical coverage.
In this case, your loved one may also have a stand-alone Part D prescription drug plan. Some Original Medicare beneficiaries also have a supplemental insurance plan, also known as Medigap, which helps cover deductibles and other costs.
Part D and Medigap plans are administered by private companies that Medicare reimburses.
Alternatively, your friend or family member may be enrolled in a Medicare Advantage, or Part C, plan.
This option is also administered by a private company. Medicare Advantage plans must provide the same basic coverage as Original Medicare but may also bundle other benefits such as drug coverage, vision, hearing and dental into a single plan.
All Medicare enrollees are issued a red, white and blue Medicare card. They may also have a separate Medicare Advantage or Part D card, if theyre enrolled in these programs.
If you cant locate these cards, you and your loved one can call the Medicare helpline together. Or, your loved one can complete a form authorizing Medicare to release information to you.
To learn more, call Medicare at 1-800-MEDICARE .
Durable Medical Equipment Costs
Durable medical equipment refers to medical supplies like wheelchairs, hospital beds, crutches, and walkers. Medicare will cover 80% of the cost of this equipment when you are receiving care from an in-home caregiver. You will have to pay the remaining 20% of the Medicare-approved amount out-of-pocket.
You May Like: Does Medicare Pay For Part D
What Services Does Medicare Not Cover
While Medicare can be very helpful in funding home health care, it does not cover everything. The following are some of the services that arent covered by these benefits:
- 24-hour supervision
- You can get personal care services if you dont additionally need competent medical care or treatment.
- You can get homemaking services if you dont need specialized medical care or treatment.
Your Medicare-certified home health business should provide a breakdown of the prices and what Medicare will pay before your care begins. This notification should also mention the amount you must pay out of pocket.
Other Ways To Cover Caregiving Costs
Because Medicare probably won’t cover all your needs, there are alternatives and forms of supplemental insurance available to help pay for caregiving expenses.
If you have a Medicare Advantage plan , you might have more flexibility with your coverage. Some plans cover nonskilled in-home care, including help with custodial care. Make sure you check what your plan covers, though, as coverage varies by carrier.
Medicare Supplement insurance is another option. Medigap plans fill in the gaps left by traditional Medicare plans. However, Medigap plans vary by state, and most don’t offer enhanced in-home caregiver coverage. If you’re looking to Medigap as an option, explore what’s available.
Consider long-term care insurance, too. Though long-term care policies don’t usually cover medical costs, many can help you pay for in-home caregiver services such as custodial care and skilled nursing care. Long-term care policies can also help cover the costs of full-time care facilities, such as nursing homes and assisted living centers.
When it comes to your health or the health of a loved one, the most important thing to do is explore your options so that you can make the best possible decision. Plan for these needs early, and you won’t need to worry about your finances when you should be focused on your health.
You May Like: Do I Have To Renew Medicare Each Year