How Do I Qualify For A Home Inr Machine
Which Patients Qualify for INR Home Testing
Medicare Expands Coverage For Home Blood Testing Of Prothrombin Time International Normalized Ratio
MEDICARE EXPANDS COVERAGE FOR HOME BLOOD TESTING OF PROTHROMBIN TIME INTERNATIONAL NORMALIZED RATIO
The Centers for Medicare & Medicaid Services today expanded Medicare coverage for home blood testing of prothrombin time International Normalized Ratio to include beneficiaries who are using the drug warfarin, an anticoagulant medication, for chronic atrial fibrillation or venous thromboembolism.
Medicares prior policy only provided home test coverage for Medicare patients with mechanical heart valves who are on warfarin.
Those Medicare beneficiaries and their physicians managing conditions related to chronic atrial fibrillation or venous thromboembolism will benefit greatly through the use of the home test, CMS Acting Administrator Kerry Weems said. Medicares coverage extension of home blood testing of prothrombin time International Normalized Ratio is based on current evidence for these two conditions.
Atrial fibrillation is an electrical disturbance of the heart that produces an irregular heart rhythm and increases the risk of stroke from blood clots forming in the heart chambers and then traveling to the brain. Patients with venous thromboembolism experience blood clots, usually in the legs, which may break off and travel to the lungsa potentially fatal complication.
Hcpcs Codes G0248 G0249 G0250
G0248 Demonstration, prior to initiation of home inr monitoring, for patient with either mechanical heart valve, chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria, under the direction of a physician includes: face-to-face demonstration of use and care of the inr monitor, obtaining at least one blood sample, provision of instructions for reporting home inr test results, and documentation of patients ability to perform testing and report results
G0249: Provision of test materials and equipment for home INR monitoring of patient with either mechanical heart valve, chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria includes provision of materials for use in the home and reporting of test results to physician not occurring more frequently than once a week
G0250: Physician review, interpretation, and patient management of home INR testing for a patient with either mechanical heart valve, chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria includes face-to-face verification by the physician that the patient uses the device in the context of the management of the anticoagulation therapy following initiation of the home INR monitoring not occurring more frequently than once a week
Also Check: How Do Zero Premium Medicare Plans Work
Medicare To Now Cover Inr Self Testing For Patients On Anticoagulants For Chronic Atrial Fibrillation And Venous Thromboembolism
The announcement this past week from the Centers for Medicare & Medicaid Services that Medicare coverage for at-home blood testing of prothrombin time /International Normalized Ratio will be expanded is welcome news to the millions of patients who take anticoagulants daily and will now have easier access to proactive, improved quality of health care. In addition to mechanical heart valve patients , the new decision expands coverage of home testing to those patients who take warfarin, an anticoagulant medication, for chronic atrial fibrillation or venous thromboembolism.
Warfarin a blood thinner used chronically by a large population of patients for a variety of medical conditions is a very critical, black-box drug whose dosage needs to be managed closely in order to minimize serious complications from continual use, including blood clots, stroke and hemorrhage, says Jack Ansell, M.D., an internationally recognized expert in hemostasis and thrombosis, and Chairman of Medicine at Lenox Hill Hospital in New York City. The scientific research and success of mechanical heart valve patients with INR home testing for the past six years serve as proof that weekly patient home self-testing helps patients remain in their therapeutic range, thereby reducing the risk of costly and deadly complications.
For more information about INR self testing, visit www.hemosense.com.
Note to Media:
Dr. Ansell will present for 15 minutes, with additional time allotted for media Q& A.
What Types Of Common Blood Tests Are Covered
Original Medicare and Medicare Advantage plans cover many types of screening and diagnostic blood tests. There may be limits on how frequently Medicare will cover certain tests.
You can appeal a coverage decision if you or your doctor believe a test should be covered. Certain screening blood tests, like those for heart disease, are fully covered with no coinsurance or deductibles.
Examples of covered blood tests
Here are some of the conditions that are commonly screened through blood tests and how often you can have them done with Medicare coverage:
- Diabetes: once a year, or up to twice per year if you are higher risk
- Heart disease: cholesterol, lipids, and triglycerides screening once every 5 years
- HIV: once a year based on risk
- Hepatitis : once a year depending on risk
- Sexually transmitted diseases: once a year
If your doctor thinks you need more frequent testing for certain diagnostic tests due to your specific risk factors, you may have to pay for testing more often. Ask your doctor and the lab for more information about your specific test.
It might be helpful to have a supplemental plan for more frequent testing. You can go to the Medicare Medigap policy website for information on all the plans for 2021 and whats covered. You can also call the plan directly for more information.
Examples of covered tests include:
| Condition |
|---|
Also Check: Does Medicare Have A Limit
How Do You Bill For Anticoagulation Management
4.2/5CPTmanaging anticoagulant therapyin-depth answer
Now, two new CPT codes allow payment when physicians order, review, and interpret new INR test resultseven when patients self-test at home: 93792 and 93793 .
One may also ask, how often can 93793 be billed? G0250 describes the physician review, interpretation, and patient management of home INR testing. This service is payable only once every 4 weeks. The date of service is the date of the fourth test interpretation. For 2018, there is also code 93793 describing the physician interpretation and instructions.
Hereof, how do I bill for PT INR?
The PT/INR test, performed with a CoaguChek XS System for Professional Use by CLIA-waived and non-waived laboratories, is billed under CPT® code 85610 with or without the QW modifier as explained below. Modifiers are often added to a CPT code to provide further information about a service provided.
Is home INR monitoring covered by Medicare?
Medicare may cover the cost of INR self-testing for patients with atrial fibrillation, mechanical heart valves and deep vein thrombosis .
Does Medicare Cover Coaguchek
Medicare Part B expands coverage for warfarin patients monitoring clotting time at home. Portable, handheld prothombin time meters, like the CoaguChek XS System for Patient Self-Testing, enable patients to test their clotting time at home in about a minute, using a small drop of blood from a simple fingerstick
Read Also: How To Be Eligible For Medicare And Medicaid
Does Medicare Cover Inr Testing Once A Month
- Asked June 23, 2015 in
Medicare Expands Coverage For Inr Testing
The Centers for Medicare and Medicaid Services has expanded coverage of home prothrombin time testing to include patients who are taking anticoagulation therapy for chronic atrial fibrillation and venous thromboembolism.
Patients must meet certain other criteria, and the home tests can’t be used more than once a week, according to the final decision issued by the CMS.
Medicare has covered home prothrombin time testing since 2002, but only for patients with mechanical heart valves. The request for expanded coverage was made in June 2007 by the three main manufacturers of home testing devicesRoche Diagnostics, International Technidyne Corp., and HemoSense Inc. The companies said that there was plenty of new evidence to support home testing for the two other conditions. The CMS agreed.
Medicare’s coverage extension of home blood testing of prothrombin time International Normalized Ratio is based on current evidence for these two conditions, CMS Acting Administrator Kerry Weems said in a statement. Currently, prothrombin testing is conducted about every 46 weeks, primarily in physicians’ offices, according to the CMS. Fewer than 5% of patients on anticoagulation therapy monitor prothrombin at home.
Those Medicare beneficiaries and their physicians managing conditions related to chronic atrial fibrillation or venous thromboembolism will benefit greatly through the use of the home test, Mr. Weems said.
You May Like: How To Get Help Paying Your Medicare Premium
Is There A Home Test For Inr
INR homeare availablehomeINR
. Regarding this, does Medicare pay for INR home testing?
The Center for Medicare and Medicaid Services is expanding its coverage of INR home monitoring to include patients on warfarin for DVT and PE , i.e., VTE .
Beside above, where can I get an INR test? Get your INR tested at your local Pharmacy. With the Community Pharmacy Anticoagulation Management Service you now have the option of visiting one of more than 150 pharmacies nationwide for immediate, gentle testing and an accurate result in seconds.
Similarly, it is asked, how much does an INR test cost?
A total of 29 studies reported the cost of one INR test, which was shown to range from $6.19 to $145.70.
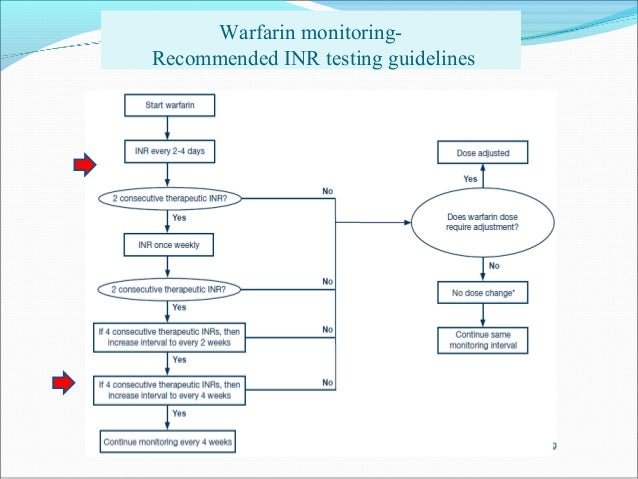
How often does INR need to be checked?
The international normalized ratio should be measured monthly once therapeutic levels are achieved and are stable for at least 8 weeks, although treatment should be individualized and an increased frequency may be required by some patients .
Inr Home Monitoring Triumphs Cms Expands Coverage
Good news! The Center for Medicare and Medicaid Services is expanding its coverage of INR home monitoring to include patients on warfarin for DVT and PE , i.e., VTE . Previously, CMS provided coverage only for home INR testing of patients with mechanical heart valves.
âThis is good news,â says Dr. Stephan Moll, chair of NBCAâs Medical and Scientific Advisory Board. âHowever, in my opinion, as long as reimbursement or the service-delivery structures do not change, I am doubtful that INR home testing will fully take off. This is very unfortunate, as INR home testing is really the way to go for many patients on warfarin. Under the present circumstances, doctors have relatively little incentive to support their patients doing self testing.â
The CMS Decision Summary is as follows:
âAfter examining additional medical evidence, we are expanding Medicare coverage of home prothrombin monitoring to include chronic atrial fibrillation and venous thromboembolism under the following conditions:
References:
Recommended Reading: Why Is My First Medicare Bill So High
Medicare Part A Costs
In-hospital blood work ordered by your doctor is generally fully covered under Medicare Part A. However, you still need to meet your deductible.
In 2021, the Part A deductible is $1,484 for most beneficiaries during the benefit period. The benefit period lasts from the day you enter the hospital through the next 60 days. It is possible to have multiple benefit periods in a year.
Medicare Part B Expands Coverage For Warfarin Patients Monitoring Clotting Time At Home
Medicare Part B has expanded coverage for warfarin patients monitoirng clotting time at home.
Medicare Part B will now pay for meter training and equipment and supplies for all long-term warfarin users who monitor their prothrombin time at home with portable handheld meters. This expansion opens the door to increased patient access to testing, which could lead to better outcomes. Medicare previously reimbursed these expenses only for patient self-testers who had mechanical heart valves. The new coverage expands to include those on anticoagulant medication with chronic atrial fibrillation and venous thromboembolism. Portable, handheld prothombin time meters, like the CoaguChek XS System for Patient Self-Testing, enable patients to test their clotting time at home in about a minute, using a small drop of blood from a simple fingerstick.
Also Check: What Are The Advantages And Disadvantages Of Medicare Advantage
American Family Insurance Dreams Foundation
Category: Insurance 1. American Family Insurance Dreams Foundation 2021 grant Mar 15, 2021 Nonprofit community organizations are invited to apply for a grant from the American Family Insurance Dreams Foundation from March 15 Aug 2, 2021 These grants are part of the American Family Insurance Free to
What Is The Cpt Code For Pt Inr
4.6/585610in-depth answer
R79. 1 is a billable/specific ICD–10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD–10-CM R79. 1 became effective on October 1, 2019.
Also Know, does Medicare cover PT INR? Medicare coverage for PT/INR testing done in a clinical setting is up to the discretion of your specific plan an agent will determine if the procedure was medically necessary using a doctors note provided by your physician. Such lab work is generally covered by Medicare Part B.
Also Know, what is procedure code 85610?
CPT 85610, Under Hematology and Coagulation ProceduresThe Current Procedural Terminology code 85610 as maintained by American Medical Association, is a medical procedural code under the range – Hematology and Coagulation Procedures.
How do you bill for anticoagulation management?
CPT code 99363 is to be used after the initial 90 days of outpatient warfarin therapy. The code is intended to reimburse the physician work involved in adjusting warfarin levels based on a review of a patient’s international normalized ratio measurements.
Don’t Miss: Does Medicare Cover Private Home Care
Cpt Codes Covered If Selection Criteria Are Met:
93792 Patient/caregiver training for initiation of home international normalized ratio monitoring under the direction of a physician or other qualified health care professional, face-to-face, including use and care of the INR monitor, obtaining blood sample, instructions for reporting home INR test results, and documentation of patient’s/caregiver’s ability to perform testing and report results 93793 Anticoagulant management for a patient taking warfarin, must include review and interpretation of a new home, office, or lab international normalized ratio test result, patient instructions, dosage adjustment , and scheduling of additional test, when performed
Does Medicare Cover Test Strips
Self-testing medical supplies have a come a long way in recent decades. Today, many people who suffer from diabetes or other insulin-related conditions are able to use simple test strips at home or on-the-go to monitor levels of certain substances in the blood. These strips are small, single-use pieces of paper-like material that are stained with a drop or two of blood and then inserted into a testing device that can provide accurate results in seconds. Through the use of test strips, diabetics and others are able to quickly address concerns regarding blood glucose levels, and they can also prevent problems by checking blood glucose levels prior to meals in order to ensure that proper levels are being maintained.
Does Medicare Pay for Test Strips?Medicare provides coverage for test strips and other self-testing supplies for individuals eligible and enrolled in Part B. Medicare Part B provides coverage for outpatient medical treatment as well as durable medical equipment. Medicare Part B covers test strips for people who take insulin and people who do not take insulin, but the program does differentiate between the two when it comes to the amount of testing supplies that are covered.
Related articles:
You May Like: How To Compare Medicare Supplement Plans
Why Are More Doctors Recommending That Their Patients Self Test
Self testing gives patients better control over their own health in several ways. First, it allows them to easily test more frequently, which has proven to help stay in range and avoid complications. Second,it allows them to test at home, reducing the cost, time and inconvenience of traveling to the lab or doctors office for a simple test. Lastly, because the doctor is alerted sooner to your test results, he or she can adjust your dosage more quickly in order to avoid any complications that might otherwise have occurred.
Does Medical Insurance Cover Dental Implants
1. How To Get Dental Implants Covered By Medical Insurance Dental implants are covered by health insurance when you can prove that the treatment is medically necessary. Unfortunately, most dental insurance policies do not cover tooth implants because most companies categorize them as a cosmetic procedure. Many insurance The good
Read Also: What Age Can You Start To Collect Medicare
The Above Policy Is Based On The Following References:
