Sleep Apnea And Medicare Coverage
Medicare coverage for treatment of sleeping disorders is generally covered by Part B. Medicare Part B is the outpatient benefit of the program, and it provides benefits for things like doctor visits, surgery, and durable medical equipment.
Medicare benefits provided by Part B may include coverage for a three-month trial use of a CPAP machine. If the use of a CPAP machine is prescribed by your doctor, Medicare may cover the rental of the equipment for up to 13 months. In order for your machine to qualify, it will need to be prescribed by a Medicare-participating physician, and the equipment will need to be available from a Medicare-approved supplier.
After the machine has been in use for 13 months, Medicare pays it off. Keep in mind that Medicare coverage for treatment of sleeping disorders using CPAP follows the standard Part B deductible requirements. This means that you will be responsible for 20% of your costs while Medicare benefits cover the remaining 80%.
TIP: Get more of your respiratory-related questions answered when you sign up for the Medicare Benefits newsletter.
To get more of your Medicare questions answered, subscribe to our free monthly newsletter
Diagnosing Sleep Apnea At Home
Getting a sleep apnea diagnosis does not need to be a stressful experience. You should always make regular visits to your doctor, but, if they want you to get tested for sleep apnea, they will just refer you to a sleep lab or a home sleep test provider. Rather than jumping through costly, drawn-out hoops, you are able to diagnose your sleep apnea at home with a home sleep testing kit.
Most at-home sleep testing kits do not even required a referral. You can take our patient questionnaire to see if you are a good candidate for sleep testing, and receive your kit in as few as 2-3 business days. Dont wait because your home sleep testing kit is the first step to a better nights sleep and a better quality of life.
Does Medicare Cover In
Yes.
In 2008, the Centers for Medicare and Medicaid Services updated the National Coverage Determination for CPAP to include home sleep apnea testing as a means to qualify patients with obstructive sleep apnea for CPAP therapy .
HST is a type of diagnostic polysomnography which is self-administered by the patient in his/her home. It is used to diagnose sleep apnea by recording several channels of information: respiratory effort, pulse, oxygen saturation, nasal flow and snoring. HST is a cost-effective alternative to in-center sleep testing for many patients if it is highly likely that the patient has moderate to severe sleep apnea, and if the patient has no other significant medical issues such as pulmonary diseases, neuromuscular disease or congestive heart failure. HST cannot be performed on children and cannot diagnose other sleep disorders such as restless leg syndrome, periodic limb movement disorder or narcolepsy. These patients should be tested in a sleep center .
You can read the American Academy of Sleep Medicine clinical guidelines for home sleep testing here.
Don’t Miss: Is It Mandatory To Have Medicare Part D
Repeat Sleep Study Indications
It may be necessary to perform repeat sleep studies up to twice a year for any of the following indications. performed in a healthcare facility is considered medically necessary for persons who meet criteria for attended NPSG in section I above in all other cases, unattended sleep studies are considered medically necessary):
Note: A home sleep study is performed over multiple nights with a single interpretation is considered a single sleep study for purposes of reimbursement.
Also Check: Is Eliquis Covered Under Medicare
How Is Sleep Apnea Treated
If you suffer from sleep apnea, treatment depends on the cause. For many people, lifestyle changes, including losing weight, can help. For others, medications may be necessary.
The use of a continuous positive airway pressure device may be necessary or individuals who suffer from obstructive sleep apnea. A CPAP machine uses a mask that is worn overnight that delivers gently forced air to keep the airway open during sleep.
If you require admittance to a hospital for treatment of your sleep apnea, Medicare Part A, the inpatient benefit, will supply coverage. This coverage also applies when admitted to a skilled nursing facility.
TIP: Read about using a CPAP machine to help manage your sleep apnea.
Find a new plan
Get recommendations based on what’s important to you, and compare them to your existing plan.
Read Also: What Will Medicare Pay For Home Health Care
Is There Any Side Effects Of Inspire Treatment
Having surgery suddenly inside the throat can cause you slight problems for some time, but nothing serious. Surgeons are familiar with patients that are worried about thinking about the post-treatment.
However, there can be two major side effects noticeable in the patients after inspire treatment.
- The first one is a bit of swelling in the incision site that is quite a common issue after any surgery.
- The second one is the slight pain or soreness on the tongue for a while. Both these pains will reduce as time goes on.
Recommended Reading: Does Medicare Pay For Physical Therapy After Knee Surgery
Does Medicare Cover Cpap Cleaners Like Soclean
Manufacturers, suppliers and sleep physicians all recommend that patients regularly clean their CPAP machines and supplies.
However, there are certain CPAP supplies Medicare wont cover.
Medicare typically doesnt pay for cleaning supplies, power solutions or certain comfort accessories.
Other CPAP supplies Medicare doesnt cover include:
- Tube covers and wraps
These items may be expensive without insurance. The SoClean device, for example, can average around $400.
You May Like: What Does Medicare Supplement Cover
What You Pay For Cpap
Because CPAP is covered as durable medical equipment, the Medicare Part B deductible applies its $233 in 2022 . Then you pay 20% of the Medicare-approved amount for the CPAP machine rental and ongoing supply purchases. If you have a Medigap plan, your 20% share should be picked up by your supplemental coverage.
If you have a Medicare Advantage plan, it may or may not cover the full costs of CPAP machines or supplies. Each plan can be different, so make sure you check your plan document or contact your plan provider to see what’s covered.
An important note: Double-check that both your doctor and your CPAP supplier are enrolled in Medicare. If not, you may be charged a non-Medicare rate for your supplies and equipment and Medicare will not pay the 80% share.
Does Original Medicare Cover Cpap Supplies
Yes. Original Medicare helps pay 80% of the cost of the following equipment after youve met your Part B deductible:6
- CPAP machine rental for a 3-month trial if youre newly diagnosed
- CPAP rental for 13 months if youve been using it consistently
- Masks or nose pieces you wear when using the machine
- Tubing to connect the mask or nose piece to the machine
Original Medicare has certain rules for replacing CPAP machine supplies. Contact your doctor or device supplier for more information.
Note: Part B also helps pay up to 80% of the costs of your sleep study if you have clinical signs and symptoms of sleep apnea. Costs covered include Type I, II, III, and IV sleep studies and devices.7
Also Check: Does Medicare Cover Bone Grafts
Philips Cpap Machine Recall
In June 2021, millions of CPAP and BiPAP machines were recalled by Philips Respironics due to the degrading of sound abatement foam inside the machines, which can break down and lead to serious health issues like inflammation in the respiratory system, cancer and other dangerous effects.
The recall was classified by the U.S. Food and Drug Administration as a Class I recall due to the toxic effects from the machines as capable of causing severe injury or death.
According to Philips, these products are not affected by the recall:
What Sleep Disorders Can Home Tests Detect
Currently, at-home sleep tests are designed to test for obstructive sleep apnea. These tests are recommended only for people with symptoms that indicate moderate to severe obstructive sleep apnea. Those with a history of cardiorespiratory diseases, stroke, insomnia, or hypoventilation should do their sleep study in a lab and not conduct an at-home sleep test.
Dont Miss: Does Medicare Cover Lasik Eye Surgery
Recommended Reading: Can I Have Humana And Medicare
Sleep Apnea & Snoring Consultation
Dr. Tucker feels so strongly that knowledge and action can improve and save lives that he is offering a no-cost, individual, 30-minute consultation on sleep breathing disorders. Whether itâs loud snoring or other sleep apnea symptoms, make sure you are not at risk for this very treatable, potentially life-threatening condition. Learn more about sleep apnea and get all of your questions answered. We have a limited number of consultation times available, so schedule yours as soon as possible.
You May Like: How To Change My Name On My Medicare Card
Cms National Coverage Policy
Title XVIII of the Social Security Act, §1862 allows coverage and payment for only those services that are considered to be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.
Title XVIII of the Social Security Act, §1862 Items and services related to research and experimentation.
Title XVIII of the Social Security Act, §1862 states Medicare will not cover any services or procedures associated with routine physical checkups.
CMS Internet-Only Manual, Pub 100-02, Medicare Benefit Policy Manual, Chapter 15, §60.1 Incident To Physicians Professional Services, §110 Durable Medical Equipment General
CMS Internet-Only Manual, Pub 100-03, Medicare National Coverage Determinations Manual, Chapter 1, Part 2, §160.7 Electrical Nerve Stimulators Chapter 1, Part 4, §240.4 Continuous Positive Airway Pressure Therapy For Obstructive Sleep Apnea Chapter 1, Part 4, §240.4.1 Sleep Testing for Obstructive Sleep Apnea
Recommended Reading: Does Medicare Supplemental Insurance Cover Hearing Aids
We Accept Medicare For Sleep Treatment
For people without traditional medical insurance who are worried about being able to afford sleep apnea therapy, we have good news: Medicare can be used to pay for a sleep oral appliance, and EZ Sleep Solutions is happy to accept many different Medicare plans as well. And, depending on your particular plan, Medicare can be used to cover much more than just an oral appliance. Our team can make the claim process nice and simple–well handle all the paperwork so you can save as much as possible without having to stress or wait. To learn how we could use your specific plan to help pay for your sleep care,give us a call today.
How Do I Choose The Right Cpap Machine For Me
A CPAP machine isnt something you buy at a local retail store. Your doctor or a respiratory therapist usually will make a specific device recommendation for you and may even point you to a supplier.
Some considerations when selecting a CPAP machine include:
- your individual preferences about a nose piece versus a full face mask
- your living situation and sleep habits
- your individual medical needs
- any specific features you may need, like compact size for travel, low motor noise, or a built-in humidifier to prevent dry mouth and nose
Your doctor will write an order for your CPAP machine with specific goals and settings in mind. Your selection should fit those needs, and your supplier should have a copy of your doctors order to ensure you receive the correct fit and device.
Don’t Miss: Is Oral Surgery Covered Under Medicare
Does Medicaid Cover Cpap Treatment
The most effective treatment for sleep apnea is the use of a continuous positive airway pressure, or CPAP, machine. These machines deliver constant and steady air pressure to your airway as you sleep through a hose connected to a mask. In general, Medicaid does cover this sleep apnea treatment.
If youre diagnosed with sleep apnea according to Medicaids criteria, the program will cover an initial 12-week period of CPAP treatment. Medicaids criteria determines how severe your sleep apnea is based on your apnea-hypopnea index . This index measures how often your breathing is interrupted each hour.
If your condition improves during the 12-week period and youve shown compliance with your usage of the CPAP machine, your treatment will continue to be covered in the future. The improvement of symptoms must be confirmed by your doctor or sleep specialist. The compliance requirement basically ensures that youre using the machine enough to gain benefits. Currently, Medicaid requires that you use the machine for at least 4 hours a night, 70% of nights within the trial period.
Keep in mind that Medicaids benefits may not cover all costs, and you may need to pay for accessories such as filters and masks.
Diagnosing Sleep Apnea In Children
Most doctors follow these guidelines from the American Academy of Pediatrics:footnote 4
- During a routine checkup, your doctor will ask you and your child about snoring. If your child snores, be sure to tell your doctor.
- A complete sleep study typically is needed to find out if your child has sleep apnea and is not just snoring.
- Children who have sleep apnea and other disorders, such as Down syndrome or sickle cell disease, may need to see a specialist.
Recommended Reading: Does Medicare Cover Rooster Comb Injections
What Are The Costs
A person enrolled in original Medicare will pay 20% of the Medicare-approved amount for DME, such as a CPAP machine, if the supplier accepts Medicare. The Part B deductible applies, which is $203 in 2021.
However, supplemental medical insurance plans, known as Medigap, may help cover out-of-pocket expenses, such as copays, coinsurance, and deductibles. Private companies offer the plans, which are available to a person with original Medicare.
In addition, a person enrolled in Medicaid may get help with out-of-pocket costs.
What Does Medicare Pay For Sleep Appliances
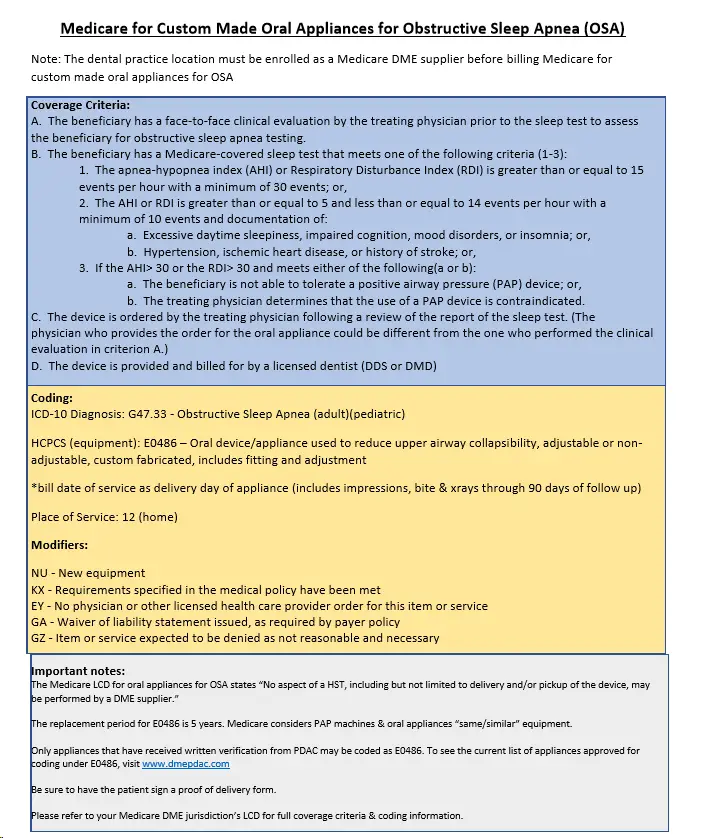
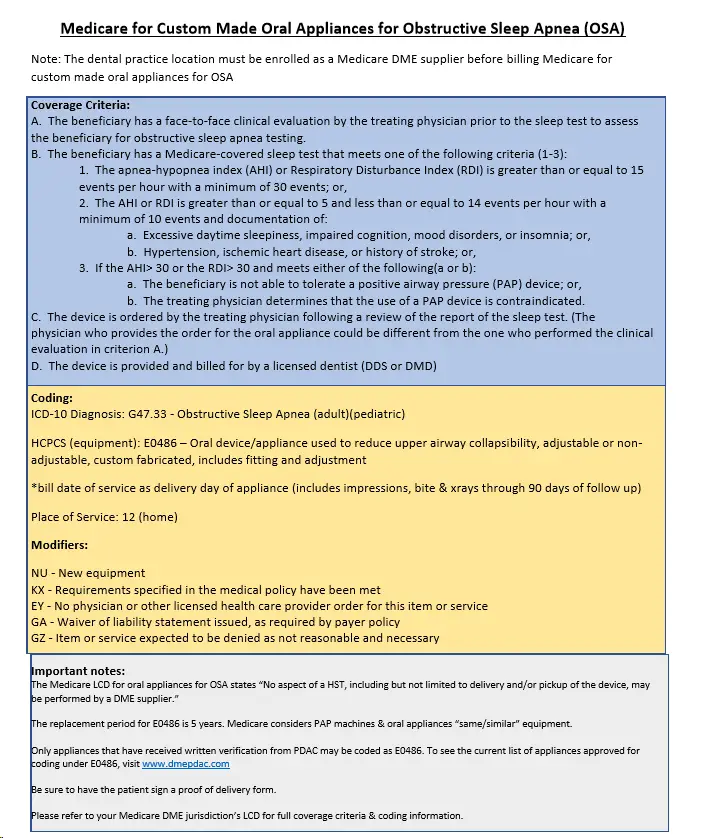
Like commercial medical insurers, Medicare offers coverage for custom-made oral appliances to treat Obstructive Sleep Apnea . It is important to know that the patient must have Part B benefits in order to be eligible for coverage. So how do you know if the patient has Part B coverage? Good news is it is easy to tell, because Part B will be listed on the front of the Medicare ID card! If only Part A is listed, the patient will not have coverage for an oral sleep appliance. Please note the dental practice location must be properly enrolled as either a participating or non-participating Durable Medical Equipment supplier to successfully bill Medicare for oral sleep appliances.
Although the patient must have Part B benefits in order to obtain coverage for an oral sleep appliance, claims for these appliances are billed to Medicare DME. Medicare DME is split into 4 geographical regions: Jurisdictions A, B, C and D. Below is a map of the Medicare DME jurisdictions, last updated June 2021):
Each jurisdiction has a different allowed amount for oral sleep appliances, and some allowed amounts within the jurisdictions vary slightly by state. The allowed amounts have not yet been officially published on any of the four Medicare DME fee schedules. Luckily, we know the allowed amounts based on processed claims from our DentalWriter Software clients and Nierman Medical Billing Service clients, and we are happy to share this information!
Don’t Miss: Does Medicare Part B Cover Blood Tests
Cost Of A Cpap Machine With Medicare
| Average cost of a CPAP machine | Medicare coverage |
|---|---|
| $203 | $373 |
The average cost of a CPAP machine without Medicare can be around $850. If it qualifies as Medicare-approved durable medical equipment, Medicare can potentially cover 80 percent of the cost, provided you meet your Part B deductible and pay any remaining costs for tubes and other accessories.
Typically, Part B assistance can go toward a three-month trial coverage for a CPAP machine if youve been officially diagnosed with obstructive sleep apnea and your doctor documents that the device is improving your health. Medicare can pay the cost of the CPAP machine rental for the first 13 months, provided that you use it on a regular basis. After that period, youll own the device.
Questions To Ask Your Sleep Surgeon

It is important to have a comprehensive understanding of the role of this treatment in your condition. The first choice for the treatment of obstructive sleep apnea is the use of continuous positive airway pressure . Success with this treatment requires proper mask fitting and optimal device settings.
In some cases, alternatives such as weight loss, bilevel therapy, the use of an oral appliance, or positional therapy can be pursued. In some cases, nothing seems to work.
Once you have exhausted treatment options with your board-certified sleep physician, it may be necessary to consider the role of the Inspire hypoglossal nerve stimulator. Consider some of these questions to ask the surgeon:
- Am I a good candidate for the surgery?
- If you couldnât do this surgery, what would they recommend as treatment instead?
- How often have they done this procedure?
- What is their success rate in resolving sleep apnea ?
- How many patients have complications such as bleeding, infection, or device removal?
- How will I know if the therapy works well for me?
- Do they have support to work through the insurance approval process?
- Will I have testing after the device is placed to determine settings and response to therapy?
- Who will I follow up with once the surgery is complete?
There may be additional considerations based on your specific circumstances.
Don’t Miss: Where Do I Apply For A Medicare Card
