How Do I Make Sure These Supplies Are Covered
In order for your blood sugar testing strips for diabetes, equipment and other supplies to be covered by Medicare, you must have a prescription from your doctor that outlines:
- Your diabetes diagnosis
- What kind of blood sugar monitor you need and why
- Whether you use insulin or not
- How often you should test your blood sugar
- How many test strips and lancets you need for one month
In addition, its important to not accept any supplies you did not order because Medicare will not pay for or reimburse you. For example, if a supplier automatically sends you items, you cannot get reimbursed by Medicare.
Medicare Guidelines For Diabetic Shoes And Inserts
20
A pedorthic device is created to treat a variety of possible foot-related problems such as congenital deformity, improper walking and partial foot amputations. If you are covered by Medicare Part B, you qualify for therapeutic shoes and/or inserts. Medicare coverage can help prevent suffering while saving you money!
Medicare Part B covers one pair of therapeutic shoes and/or inserts and one fitting each calendar year. If you qualify, you are limited to one of two types of the following shoes each year:
- One pair of depth-inlay shoes and three pairs of inserts
- One pair of custom-molded shoes if you cant wear depth-inlay shoes because of a foot deformity, and two addition pairs of inserts.
In order for Medicare to cover the cost of your therapeutic shoes, the doctor treating your diabetes must verify that you meet three conditions:
Medicare also requires that:
- Your doctor confirms your need for therapeutic shoes or inserts.
- A podiatrist or other qualified doctor prescribes them.
- Your items are provided by a podiatrist, orthotist, prosthetist or pedorthist
Contact Us
Also Check: How Much Does It Cost To Ship Shoes Ups
Who Qualifies For A Continuous Glucose Monitor
Medicare will cover CGMs for people who:
- Have an established diagnosis of Type 1 or Type 2 diabetes
- Are currently using a traditional blood glucose monitor
- Must check their blood sugar a minimum of four times daily
- Use insulin to treat diabetes and require frequent adjustments to their regimens or have a subcutaneous insulin infusion pump
- Receive training from their doctors on how to use CGMs
You May Like: How To Fill Out Medicare Part B Application
What Does Medicare Cover For People With Diabetes
Medicare covers 80% of the below products. Insurance holders by an annual deductible as well as the remaining 20% of all expenses. Some individuals may have private insurance to supplement this remaining 20%, making many of these items free of charge for insurance and Medicare holders.
The information listed below is subject to change at any time. Please check directly with Medicare to confirm coverage.
Will Medicare Cover My Diabetic Shoes And Inserts
If you have certain medical conditions related to your diabetes, such as severe diabetic foot disease, Part B might cover one pair of depth-inlay or custom-molded shoes each year and up to three pairs of inserts each year. You generally pay 20% of allowable charges plus any applicable deductibles.
Part B may also cover the professional fees of the podiatrist or other doctor who prescribes the shoes and of the health-care provider who fits them, up to allowable amounts, less your coinsurance and applicable deductibles.
Read Also: How To Get Bleach Stains Out Of White Shoes
You May Like: How To Sign Up For Medicare Advantage
What Are Continuous Glucose Monitors
Continuous glucose monitors are devices that let you check your blood sugar without having to collect a blood sample each time. To use one, you insert a patch into the skin on the back of your arm. Sensors in the device track your blood sugar levels continuously. When you want to see your number, you hold a receiver up to the patch. Some CGMs have an app that turns your smartphone into a receiver. The app also stores your readings and can send them to your doctor if you wish.
CGMs offer many benefits, including:
- Reduced need for finger sticks
- Greater accuracy, as the devices are not typically affected by over-the-counter medications
- Easier tracking with mobile app
- Fewer low blood glucose emergencies because many devices warn you of out-of-range readings with alarms
How To Get Your Diabetic Shoes Through Insurance
HOW TO GET YOUR DIABETIC SHOES THROUGH YOUR INSURANCE:
If you are diabetic and have Medicare and Medicaid, you could be eligible for a pair of shoes and 3 pairs of moldable insoles. It is that easy! All you have to do is bring in your insurance cards and a prescription from your doctor. We will contact your doctor for any additional information we need for billing.
The process for getting shoes is very simple. First our diabetic shoe fitter will take a measurement of both feet for a personalized fit. Then you pick out the shoes you would like. After we place your order, your shoes will arrive in 7-10 days.
If you are not diabetic, do not have Medicare, or your doctor does not approve you for these shoes, the price ranges from $115-$145 a pair. Our moldable insoles cost $50.00 per pair. However, we often run specials on our insoles and shoes. Please call us for our current specials.
For more information about diabetic shoes call us at573-442-0194 or stop by today!
Recommended Reading: Does Medicare Part B Cover Home Health Care Services
What Diabetic Supplies Are Covered By Original Medicare
Original Medicare Part B covers some diabetic supplies, including:
- Blood sugar test strips
- Blood glucose monitors, lancet devices, and lancets
- Glucose control solutions for checking the accuracy of test strips and monitors
- Insulin if you are using a medically necessary insulin pump
- Therapeutic shoes or inserts
There may be coverage limits on the quantity and frequency you can get these supplies.
Original Medicare Part B does not cover these diabetic supplies:
- Insulin
- Insulin pens, syringes, or needles
- Alcohol swabs or gauze
Verify: Does Medicare Only Cover One Diabetic Test Strip A Day For Non
Viewer Betty Fischer said she took her doctor’s prescription to get four diabetic test strips a day to a CVS Pharmacy in White Plains, Maryland.
But CVS pharmacists told her they would only supply her one strip a day. So she asked the Verify team: does Medicare only cover one test strip a day if you are not on insulin?
First we checked with the Centers for Medicare & Medicaid Services about their coverage policy.
Medicare Part B patients are covered for 100 strips a month. If you’re not on insulin, you’re covered for 100 strips every three months.
But you can get more with the right kind of medical documentation.
We then spoke with a CVS Health spokesperson who said the pharmacy follows those Medicare guidelines, but they won’t hand out those extra strips.
CVS sent the following statement to Verify researchers:
CVS Pharmacy is committed to supporting the health needs of patients who have diabetes while also complying with applicable requirements and guidelines. We abide by Medicares standard utilization guidelines for diabetic testing supplies dispensed to Medicare Part B patients in order to meet Medicare’s medical necessity requirements: once per day for non-insulin dependent Medicare Part B patients and up to three times per day for insulin dependent Medicare Part B patients. Failure to abide by these requirements jeopardizes our ability to continue to service the hundreds of thousands of seniors who rely on our pharmacy services through Medicare.
Read Also: Does Mayo Clinic Take Medicare Patients
About The Supplier And Assignment
You must make sure that the supplier, who will be from one of the listed professions above, is Medicare-enrolled, and that they are a participating supplier.
If they are not Medicare-enrolled you will not receive coverage.
If they are not a participating supplier this means they do not accept assignment, which is the Medicare-approved price, and can charge much more than a participating supplier who accepts assignment, so do verify that with them.
Dont Miss: How To Get Bleach Stains Out Of White Shoes
Medigap Plans Can Help Cover Diabetes Test Strips Medicare Costs
If Medicare covers your test strips and other diabetes supplies, you will typically be responsible for a number of out-of-pocket costs.
One way to get some help covering these costs is to apply for a Medicare Supplement Insurance plan.
For example, each of the 10 standardized Medigap plans available in most states provide coverage for the Medicare Part B coinsurance or copayments you might face when you receive covered diabetes supplies, test strips and other services.
A licensed agent can help you decide on a Medicare option that works for you. Call today to speak with a licensed agent and compare the Medigap plans that are available where you live.
Don’t Miss: What Medicare Premiums Are Deducted From Social Security
Medicare Diabetes Prevention Program
Medicare offers a health behavior change program called the Medicare Diabetes Prevention Program. The idea is to help you prevent the onset of type 2 diabetes. Part B covers the entire cost when you meet the program requirements.
The following must apply for Part B to pay for the Medicare Diabetes Prevention Program:
- A BMI of or above 25 or 23+ if youre Asian
- Never diagnosed with type 1 or 2 diabetes
- Never participated in the program before
- Received a test result between 5.7 and 6.4%
- Never diagnosed with End-Stage Renal Disease
After joining, the program starts with 16 core sessions that you receive for six months. Each session is in a group setting. The benefits of the program are to help change long-lasting behaviors. The program teaches tips on how to exercise more and managing your weight. Get support from people with like-minds and goals.
Get A Free Quote
Find the most affordable Medicare Plan in your area
Does Medicare Cover Shoes For Diabetics

Does Medicare Cover Shoes for Diabetics?
Proper footcare is essential for people with diabetes. In many cases, proper foot care means wearing special shoes for diabetics.
These shoes are often covered by Medicare, which will cover the cost of one pair of diabetic shoes per customer each year.
However, this option expires at the end of the calendar year, so now is the time to act. But before we discuss Medicares criteria for diabetic footwear coverage, lets address why these shoes are necessary in the first place.
Recommended Reading: A Medicare Supplement Policy Must Not Contain Benefits Which
How Do I Get My Medicare Diabetes Supplies
You can order and pick up supplies from your pharmacy, or you can order them from a DME supplier.
If you order from a supplier, you must place the order yourself, meaning a doctor cannot call it in for you. However, you will still need a prescription from your doctor to place the order.
When you go to the pharmacy or supplier, show your red, white and blue Medicare card and your prescription.
You can also order supplies through the Medicare National Mail-Order Program, including test strips, lancets and lancet devices. If you want your supplies mailed to your home, you must use a Medicare national mail-order contract supplier. You can visit www.Medicare.gov or call Medicare for a list of contracted suppliers.
You need a new prescription from your doctor for lancets and test strips every 12 months, so dont forget to ask for refills for your supplies every year.
How Much Do Testing Supplies Cost
If youve met your Part B deductible , you will pay 20 percent of the Medicare-approved amount for diabetic testing supplies. Medicare pays the other 80 percent.
Depending on the type of equipment or supplies you need, you may need to:
- rent the equipment.
- buy the equipment.
- choose whether to rent or buy the equipment.
Additionally, your durable medical equipment will only be covered if your doctors and DME suppliers are enrolled in Medicare. You must also purchase your testing supplies from a supplier who accepts assignment. In this case, they can only charge you the coinsurance and Part B deductible.
Accepting assignment means the supplier agrees to be paid directly by Medicare and accepts the payment amount Medicare approves for the service. The Medicare-approved amount is the amount a supplier can be paid by Medicare, and you pay the rest.
To ensure your supplier is enrolled in Medicare, ask if they participate in Medicare before you order the supplies.
How much you will specifically pay for supplies depends on a variety of factors such as:
- Other insurance you may have.
- How much your doctor charges.
- Where you get your supplies.
- Whether your doctor and supplier accept assignment.
Recommended Reading: How Do Zero Premium Medicare Plans Work
Are Diabetic Supplies Covered By Medicare Part B
Diabetes At-a-Glance Generally, Part B covers the services that may affect people who have diabetes. Part B also covers some preventive services for people who are at risk for diabetes. You must have Part B to get services and supplies it covers. Part D covers diabetes supplies used to inject or inhale insulin.
Does Medicare Cover Continuous Glucose Monitors
- Get the facts about Medicare coverage of continuous glucose monitors . Find out who qualifies for CGMs and how much you can expect to pay out of pocket.
The U.S. Centers for Disease Control and Prevention advises that regular blood sugar monitoring can improve the effectiveness of treatments for Type 1 and Type 2 diabetes and lower the risk of serious complications like blindness, heart attack and stroke. Continuous glucose monitors make it easier to keep tabs on your blood sugar levels throughout the day, and the most popular models are often covered by Medicare.
Recommended Reading: Is Medicare A Form Of Socialism
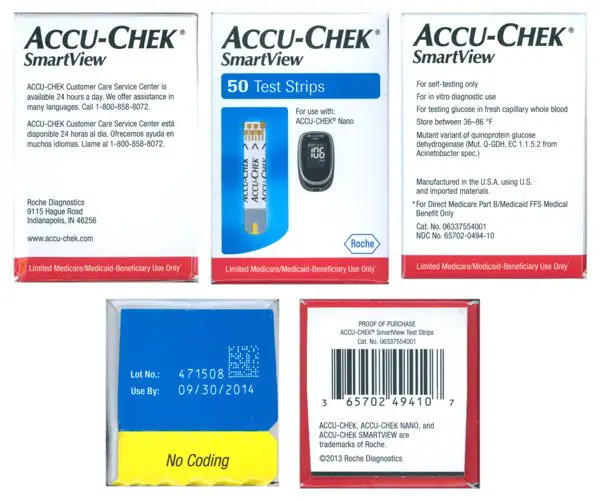
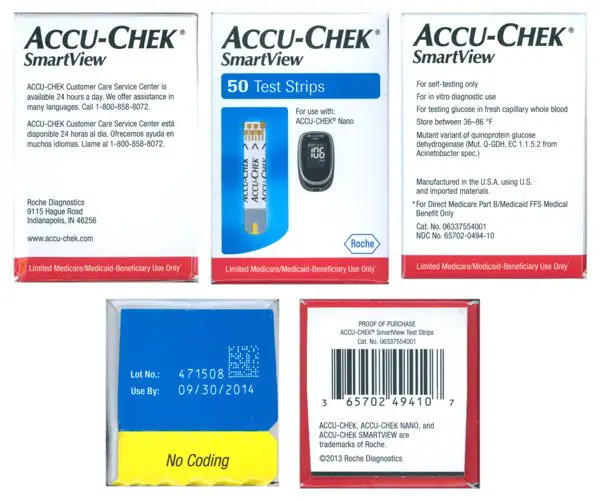
What Brand Of Diabetic Test Strips Does Medicare Cover
Medicare covers a number of common blood glucose monitors and their test strips. Examples include OneTouch and Accu-Chek. If you prefer a particular brand, your doctor can write the prescription saying Do Not Substitute.
If you have Medicare Advantage, your plan may have preferred vendors or dictate what diabetes testing brands are covered. You should contact your insurance company to determine what brands your insurance company covers. This will ensure youll be reimbursed for your blood glucose monitor and testing strips.
Under Medicares rules for mail-order suppliers, the suppliers must provide the same options for blood glucose monitors to those with Medicare as they do for customers with other insurance types.
Medicare Reimbursement: An Explanation Of Benefits
Nearly 30 million Americans have diabetes, according to the Center for Disease Control. In fact, studies suggest prescription diabetic footwear can help prevent serious foot health complications that can arise because of diabetes.
Medicare and supplemental insurance may reimburse part or all the cost of Dr. Comfort shoes and prescription inserts for diabetics who meet certain criteria. A qualified health professional can determine if eligible. If diabetic or have any foot health concerns, we strongly encourage the patient to see a foot health professional to address all foot health needs.
Also Check: Are Naot Shoes Good For Plantar Fasciitis
You May Like: How To Get Your Medicare Number
How Much Does Medicare Pay For Diabetic Supplies
Medicare alone doesnt pay in full for most medical services, including diabetic supplies. Medicare Part B covers about 80% of the costs of a variety of supplies that are used to treat diabetes. Part B will typically cover these services and supplies up to 80%, leaving you responsible for the other 20% as well as any deductibles or copays. In order to help with the expenses, most people have a Medicare Supplement plan or a Medicare Advantage plan.
Its important to note that Medicare Supplement plans rangein coverage, and theyll all pay their portion as long as Medicare pays first. Thecost of your supplies may differ depending on which Medicare Supplement planyou choose.
If you have aMedicare Advantage plan, its your primary coverage instead of Medicare. Forinformation on what your Advantage plan covers, you should contact yourprovider directly.
Does Medicare Cover Diabetic Test Strips
- Medical supplies, such as diabetic test strips, are typically covered by Medicare Part B. However, limitations on quantity, providers and brand may apply.
Medicare Part B covers some forms of durable medical equipment , a category under which diabetic test strips may fall. The variances in coverage come in the form of quantity, provider type and manufacturer.
Read Also: How To Compare Medicare Drug Plans
How Many Diabetic Test Strips Will Medicare Pay For
Medicare will pay for up to 300 test strips and 300 lancets every month when you use insulin to manage your diabetes. If you dont use insulin to control your diabetes, you may still be able to qualify for 100 test strips per month.
If you test your blood sugar more frequently, you may be able to get more test strips. Your doctor will have to write a prescription stating that receiving more test strips is medically necessary. Your doctor may ask you to keep a log of how often you test your blood sugar levels to further support that you need more than the allotted amount of test strips.
What extra benefits and savings do you qualify for?
Treatment For Foot Ulcers
People with diabetes are more susceptible to foot ulcers. Foot ulcers can get infected and spread throughout the entire body if not treated. One of the side effects of diabetes is reduced blood flow to the legs. If severe enough, reduced blood flow can result in neuropathy, which makes people lose feeling in their feet. This means that they might not realize they have painful injuries on their feet, and what started as a callus or sore can evolve into an ulcer.
AtPerformance Foot and Ankle, we provide treatment for diabetic foot ulcers. Even if an ulcer develops, there is still time to have it removed before it spreads the infection to the bone. We also participate in the Medicare Diabetic Shoe Program to help patients reduce their risk of developing a foot ulcer.
If you believe you have a foot ulcer, have it examined by a professional right away. Call 380-3152 to contact our podiatrists in Thousand Oaks.
Read Also: How To Get A Medicare Number As A Provider
