What Is Medicare Vs Medicaid
Medicare and Medicaid are not the same. Many confuse the benefits of Medicare vs. Medicaid as they are both government-run health insurance programs in the United States. However, Medicare is federal, and Medicaid differs by state.
Medicare benefits are the same across all states and U.S. territories. Typically, Medicare benefits are available to those 65 and over or receiving Social Security Disability benefits under 65. Medicare offers standardized premiums that are consistent for those in the same income bracket.
On the other hand, each states government operates Medicaid. Every state has different qualifications and requirements for enrollment in Medicaid. While there is no age requirement for Medicaid, there is a financial requirement. Your income and resources may not exceed state-specific thresholds to be eligible for Medicaid coverage. Medicaid coverage typically comes at no cost to the beneficiary.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
To differentiate the two, with Medi-care, think of care for those 65 and over or those with disabilities. Then, Medic-aid is an aid to those with a low income.
Q What Documents Will I Need To Provide When I Apply
A. You will need to provide verification of your income. You do not need to provide proof of your assets or resources or come into our offices to be interviewed unless you are applying for one of the Long Term Care Medicaid programs .
If you are pregnant, you will need to provide proof that you are pregnant. If you are not a U.S. citizen, you will need to provide proof of your alien status. For example, you can provide a copy of your green card.
If you apply online using ASSIST, a web page at the end of the application will tell you exactly what documents must be sent by mail to support the application you are submitting, and the appropriate mailing address.
Extra Help To Pay For Medicare Prescription Drug Costs
Extra Help is a Medicare program to help people with limited income and resources pay Medicare prescription drug costs. You may qualify for Extra Help if your yearly income and resources are below these limits in 2022:
- Single person – yearly income less than $20,388 and less than $14,010 in other resources per year
You may qualify even if you have a higher income . Resources include money in a checking or savings account, stocks, bonds, mutual funds, and Individual RetirementAccounts . Resources dont include your home, car, household items, burial plot, up to $1,500 for burial expenses , or life insurance policies.
If you qualify for Extra Help and join a Medicare drug plan, you’ll:
- Get help paying your Medicare drug plan’s costs.
- Have no late enrollment penalty.
You automatically qualify and will receive Extra Help if you have Medicare and meet any of these conditions:
- You have full Medicaid coverage.
- You get help from your state Medicaid program paying your Part B premiums .
- You get Supplemental Security Income benefits.
Drug costs in 2022 for people who qualify for Extra Help will be no more than $3.95 for each generic drug and $9.85 for each brand-name drug.
Recommended Reading: Does Medicare Cover A1c Test
Q If I Have Private Health Insurance Can I Be Eligible For Medicaid
A. It depends. If your income is low, and you have minor children, you and your children can have private health insurance and still be eligible for Medicaid. Certain Medicaid qualifying programs require that you not have any other health insurance in order for you to get Medicaid. If you have both private health insurance and Medicaid, you should show both your Medicaid card and your private health insurance card to your medical provider each time you receive services.
Does Medicaid Pay Secondary To Medicare Advantage Plans
Medicaid is always the secondary payer when it comes to health insurance, says Watts.
Medicaid never pays first for services covered by Medicare. Instead, it pays for whatever isnt covered by Medicare. Medicaid may also cover some drugs and additional services that the Medicare Advantage plan doesnt cover fully or at all.
Medicaid is a great benefit for consumers who are eligible, says Watts. However, if you dont meet the criteria, he recommends looking into other avenues of help that may be available. For instance, if you dont qualify for Medicaid, you may qualify for a Low Income Subsidy . LIS helps cover prescription card costs, and pays for a portion of your drugs as well, says Watts.
Some states like New York may have pharmacy assistance programs, as well as additional help from private drug companies.
Also Check: Do You Need Referrals For Medicare
Can A Person Be Enrolled In Both Medicare And Medicaid
A: In many cases, yes. Some people do qualify for both Medicare and Medicaid, and in those instances, most of the enrollees health care costs are covered. People who are eligible for Medicaid and Medicare are known as dual eligible about 20 percent of Medicare beneficiaries are also eligible for Medicaid.
Who Is Eligible For Medicaid
Medicaid is a health insurance program that is jointly operated by federal and state governments and provides coverage for individuals and families who have low incomes or limited financial resources.
Because each state administers its own Medicaid program, eligibility criteria can vary by state. Medicaid eligibility generally depends on your income, family size and state. You may use this tool from HealthCare.gov to help determine your Medicaid eligibility.
You May Like: Vision Care That Accepts Medicaid
You May Like: Are Audiologists Covered By Medicare
Already Enrolled In Medicare
If you have Medicare, you can get information and services online. Find out how to .
If you are enrolled in Medicare Part A and you want to sign up for Part B, please complete form CMS-40B, Application for Enrollment in Medicare Part B . If you are applying for Medicare Part B due to a loss of employment or group health coverage, you will also need to complete form CMS-L564, Request for Employment Information.
You can use one of the following options to submit your enrollment request under the Special Enrollment Period:
Note: When completing the forms CMS-40B and CMS-L564:
- State I want Part B coverage to begin in the remarks section of the CMS-40B form or online application.
- If possible, your employer should complete Section B.
- If your employer is unable to complete Section B, please complete that portion as best as you can on their behalf and submit one of the following forms of secondary evidence:
- Income tax form that shows health insurance premiums paid.
- W-2s reflecting pre-tax medical contributions.
- Pay stubs that reflect health insurance premium deductions.
- Health insurance cards with a policy effective date.
- Explanations of benefits paid by the GHP or LGHP.
- Statements or receipts that reflect payment of health insurance premiums.
Some people with limited resources and income may also be able to get .
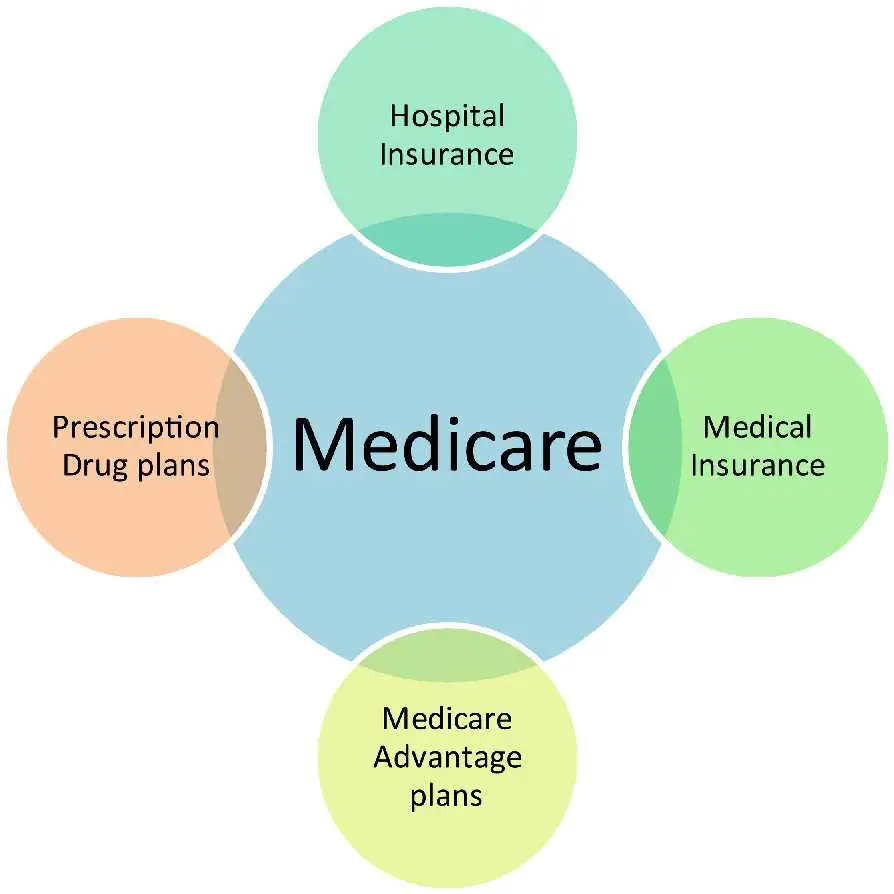
The Parts Of Medicare
Social Security enrolls you in Original Medicare .
- Medicare Part A helps pay for inpatient care in a hospital or limited time at a skilled nursing facility . Part A also pays for some home health care and hospice care.
- Medicare Part B helps pay for services from doctors and other health care providers, outpatient care, home health care, durable medical equipment, and some preventive services.
Other parts of Medicare are run by private insurance companies that follow rules set by Medicare.
- Supplemental policies help pay Medicare out-of-pocket copayments, coinsurance, and deductible expenses.
- Medicare Advantage Plan includes all benefits and services covered under Part A and Part B prescription drugs and additional benefits such as vision, hearing, and dental bundled together in one plan.
- Medicare Part D helps cover the cost of prescription drugs.
Most people age 65 or older are eligible for free Medicare hospital insurance if they have worked and paid Medicare taxes long enough. You can sign up for Medicare medical insurance by paying a monthly premium. Some beneficiaries with higher incomes will pay a higher monthly Part B premium. To learn more, read .
Recommended Reading: What Are The Parts Of Medicare
What Is The General Difference Between Medicaid And Medicare
Medicaid is a government assistance program that typically covers medical costs for low-income individuals, including pregnant individuals and children. Individuals must qualify for Medicaid based on their states requirements. Medicare is a government health insurance program for which most people at least 65 years old qualify.
What Is A D Snp
Like other SNPs, D-SNPs are Medicare Advantage plans available to Americans with qualifying conditions, diseases, or characteristics. In this case, a D-SNP is available to seniors who qualify for both Medicare and Medicaid. While plans may differ by state, most D-SNPs offer a basic level of coverage and coordination between the two programs.
Read Also: Does Medicare Pay For Air Evac
Can I Get Help With My Prescription Drugs
For many people, prescriptions are their number one health care cost. There are several ways that low-income people with both Medicare and Medicaid benefits can get extra help with their prescriptions. The first and most important way is to apply for the Social Security Administrations Extra Help program. This program provides low-income subsidies program helps Medicare beneficiaries pay for their Medicare Part D prescription drugs by paying some of the costs. Also known as Extra Help, beneficiaries who qualify for LIS receive premium) to those who need them. These subsidies can help you pay all or part of the monthly premium for a Medicare Part D plan, and is worth about $5,000 per year. You will need to call Social Security directly at 1-800-772-1213 to check your eligibility.
If you are able to enroll in a Special Needs Plan, your SNP will include prescription drug coverage and pay many of the out-of-pocket costs with regular Medicare Advantage plans. Enrollees pay small copayments, but you dont have an annual deductible. You can use our SNP directory to discover enrollment opportunities in your area.
Can I Change Plans If Im Dual Eligible
Yes. If you have Medicare and full Medicaid coverage, you can change plans once per calendar quarter for the first three quarters. The new plan will take effect the first day of the following month.
Fourth-quarter changes must be made during Medicares Open Enrollment Period. Also known as the Annual Enrollment Period, it runs from October 15 and December 7, and changes will go into effect January 1.
Read Also: Does Medicare Pay For Physical Therapy After Knee Surgery
What Is The Income Range For Beneficiaries Who Are Dual Eligibles
Generally, beneficiaries earning less than 135 percent of the federal poverty level are eligible for the MSP if they also have limited savings . This equates to $17,226 annually for single beneficiaries and $23,274 for married couples. Beneficiaries qualify for full Medicaid benefits if their incomes and assets are even lower .
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances. It is also common for Medicare beneficiaries who are under 65 and live on Social Security Disability Insurance to receive Medicaid benefits.
How To Combine Medicare And Medicaid To Save Money
Many seniors in the United States have dual eligibility for Medicare and Medicaid benefits. Generally, this means that you have enrolled in Medicare, but that you qualify for Medicaid as well due to your income. When you have dual enrollment, Medicare is your primary insurance that covers any costs first. Medicaid is your secondary payer.
You May Like: Do I Need Medicare If I Have Medicaid
If You Have Medicare And Medicaid Ask Us About:
- Free comprehensive physical exams
- Free respite care sessions for members with dementia, including Alzheimers disease*
- Free hearing services including hearing aids*
- A Peoples Health plan ID card thats widely accepted and easy to use
*May not be available with all special needs plans
Many people with Medicaid have faced tremendous hurdles to achieve good health throughout their lives. Weve designed our special needs plans to help lower or remove those hurdles through enhanced benefits and coordinated care.
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Don’t Miss: What Is The Deadline For Medicare Supplemental Insurance
How Dual Eligibility Works
Logically, there is some overlap between these two programs. A significant number of senior Medicare beneficiaries do not have substantial income or retirement savings to fund their health care and long-term care. Once a Medicare beneficiary has nearly exhausted their financial resources and meets strict state-specific income and asset limits, they may apply for full Medicaid benefits. These individuals are known as full-benefit dual-eligibles.
Read:Qualifying for Medicaid to Pay for Long-Term Care
A senior may also become a dually eligible beneficiary by qualifying for one of four Medicare Savings Programs offered by their states Medicaid program to help pay Medicare premiums and sometimes coinsurance and copayments. These benefits are not as comprehensive compared to the combination of Medicare and full Medicaid, but MSPs feature higher asset limits and more flexible income limits. Individuals who qualify for MSPs are known as partial-benefit dual-eligibles.
Read Also: Medicaid For The Aged Blind And Disabled
What Are The Four Medicare Savings Programs
- The Qualified Medicare Beneficiary program helps pay for Part A and B premiums as well as deductibles, coinsurance and copays. If you qualify for this program, you automatically qualify for the Extra Help prescription drug program to help with the out-of-pocket costs of your medicines. This program has the lowest income threshold of the four.
- The Specified Low-Income Medicare Beneficiary program helps pay only for Part B premiums, not the Part A premium or other cost sharing. If your income is too high to qualify for the QMB program, you might qualify for this one. You also automatically qualify for Extra Help for prescription drugs.
- The Qualifying Individual program only helps pay for Part B premiums and no other cost sharing. If your income is too high for you to qualify for the QMB or SLMB programs, you might qualify for the QI program. To get help from this program, you must reapply for benefits every year. Funding is limited, so these benefits are first come, first served. Priority is given to individuals who received help through this program the previous year.
- The Qualified Disabled and Working Individuals program only helps pay for Medicare Part A premiums. This program is designed for individuals with disabilities, under age 65, who are currently working and lost their premium-free Part A benefit when they began to work. To qualify, you cannot be receiving Medicaid in your state, and you must meet the income and resource limits set by your state.
Recommended Reading: What Is The Average Premium For Medicare Advantage Plans
Does Medicaid Qmb Cover Medicare Advantage Plans
The terminology around QMB and Medicare/Medicaid can get confusing and can vary by state, says Watts. A QMB is a Qualified Medicare Beneficiary program, which means that Medicare premiums and coinsurance and copayment for Medicare-covered services are covered by Medicaid.
A QMB Plus program is when someone gets full Medicaid benefits.
Either way, these QMB programs do work with both Original Medicare and Medicare Advantage plans. Because these plans can be confusing, its a wise idea to consult with someone or connect with a plan provider who can clearly explain your options.
Will I Lose My Medicaid If I Get Medicare
En español | You will not lose Medicaid eligibility just because you become entitled to Medicare. As long as your income falls under the limits for Medicaid eligibility in your state, you will receive both types of coverage. More than 8 million people have both Medicare and Medicaid.
How do Medicare and Medicaid fit together?
Medicare and Medicaid Teaming Up for Coverage When youre enrolled in both programs, Medicare will cover your medical service first. When paired with Medicare, Medicaid is considered a payer of last resort, meaning that it will cover things that Medicare doesnt or only partially covers.
What are the requirements for Medicare and Medicaid?
Medicare and Medicaid eligibility
- a person eligible for the Social Security disability program whos also the widow or widower and is age 50 or older.
- the child of a person who worked a minimum length of time at a government job and paid Medicare taxes.
You May Like: What Mental Health Services Does Medicare Cover
Medicaid And Medicare Work Together
Medicare beneficiaries who have limited income and resources may get help paying for their Medicare premiums and out-of-pocket medical expenses from Medicaid. Medicaid also covers some important services not provided under Medicare, such as community-based long-term services and supports, nursing facility care , and a wide array of behavioral health services. As of 2014, more than 10.7 million Americans were enrolled in both Medicare and Medicaid two-thirds were elderly individuals with low incomes, and one-third were under age 65 with disabilities.
When care is provided to Medicare-Medicaid beneficiaries through an integrated care model, the beneficiary can get the full array of Medicaid and Medicare benefits through a single delivery system. This approach can improve care coordination and quality, and reduce administrative burdens. One such model is the Program for All-Inclusive Care for the Elderly, or PACE. PACE provides comprehensive medical and social services to certain frail elderly individuals enabling them to continue living in the community. There are currently 113 PACE programs operating in 32 states.
CMS is offering links/charts for informational purposes only, facts should not be construed as an endorsement of the organization’s programs or activities