If Your Care Is Being Decreased
If youre being treated in a skilled nursing facility or a home health agency, the facility may notify you that Medicare wont pay for a portion of your care, and they plan to reduce your services.
If that happens, youll receive one of the following:
- a Skilled Nursing Facility Advance Beneficiary Notice
- a Home Health Advance Beneficiary Notice
- a Notice of Medicare Noncoverage
If you have a Medicare Advantage plan, youll need to contact your plan and follow the guidelines for filing an expedited appeal.
If you have original Medicare, you have three options:
- Ask for demand billing. Thats where you continue to receive care until the healthcare provider bills Medicare and Medicare denies coverage. If Medicare wont cover your care, you can start the appeals process then.
- Pay for your continued care out of pocket.
- End care from your current provider and find another provider to treat you.
A home health agency might deny your request for demand billing if:
- Your doctor thinks you no longer need care.
- They dont have enough staff to continue your treatment.
- It isnt safe for you to be treated in your own home.
Termination Of Rehabilitation Services Through Medicare
Medicare provides rehabilitation and skilled nursing therapies to those who need those services. If you have fallen victim to a crippling disease, whether it be a stroke or Parkinsons, you are eligible. How long is Medicare required to provide those services? In a recent federal district court case, the Centers for Medicare and Medicaid Services agreed to a settlement to clarify the circumstances by which Medicare will continue to pay for rehabilitation even if the patient is not objectively improving. This is a very significant development. Instead of terminating Medicare coverage outright, an attending therapist must do the following:
After assessing a patients clinical condition, the skilled nursing therapist must conclude that his or her advanced services are needed in one of three circumstances:
- To improve the patients condition
- To maintain the patients condition
- To prevent or slow further deterioration of the patients condition
It is critical to be aware of your care, as the financial consequences can be severe. If you or a loved one need assistance fighting an observation status classification or are unsure of how to deal with the hospital and Medicare moving forward, you need an experience Medicare appeal attorney on your side, and we are here to help you.
Fredrick P. Niemann Esq.
Call Fredrick P. Niemann toll-free at 376-5291 or email him at .
He welcomes your calls and inquiries and youll find him easy to talk to about your most sensitive concerns.
How Long Does A Medicare Appeal Take
You can expect a decision on your Medicare appeal within about 60 days. Officially known as a Medicare Redetermination Notice, the decision may come in a letter or an MSN.
Medicare Advantage plans typically decide within 14 days. Prescription plans usually respond within 72 hours.
If you are disputing a hospital discharge, you can file an expedited appeal. An expedited appeal may also be available if Medicare suddenly stops covering services you are currently receiving.
Also Check: Does Medicare Cover Urgent Care Centers
How Do I Appeal If I Have Original Medicare
Original Medicare includes Part A and Part B .
Medicare Part A includes:
-
A limited stay at a skilled nursing facility after hospitalization
-
Some home healthcare
-
Hospice care
Medicare Part B pays for services, vaccines, and medications not covered under other parts of Medicare.
Original Medicare enrollees receive a Medicare summary notice, in the mail every three months. This statement details items and services that suppliers billed to Medicare each quarter, what Medicare paid, and what you may owe. The MSN also shows whether Medicare has approved, fully denied, or partially denied your medical claim. This is an initial determination made by the Medicare Administrative Contractor that processes Medicare claims.
You are entitled to an expedited appeal, or fast appeal, if you think youre being discharged too soon from a Medicare-covered inpatient hospital stay. If you ask for an appeal in writing or by phone no later than the day youre scheduled to be discharged, you can remain in the hospital without paying for the additional time while you wait for a decision from the Beneficiary and Family Centered Care-Quality Improvement Organization . You must ask the BFCC-QIO for a fast appeal by noon the day before the coverage termination date for a Medicare-covered skilled nursing facility, home health agency, comprehensive outpatient rehabilitation facility, or hospice services you think are ending too soon.
Filing An Initial Appeal If You Have A Medicare Part D Prescription Drug Plan
You have the right to receive a written explanation from your Medicare Part D plan about whether a certain drug is covered, whether you have met the requirements to receive that drug and how much youll pay for it.
The benefits booklet provided by your Part D insurer includes step-by-step instructions explaining what you can do if you have problems or complaints related to your drug coverage and costs.
If you believe or your doctor believes you need a medication that isnt on your plan list, you can ask for a special exception. You also can ask to pay a reduced price for an expensive drug if the less expensive options dont work for you and your condition.
Anytime you request a plan exception, your doctor, or a health care provider who is legally allowed to write prescriptions, must provide a statement explaining why you should be given an exception.
Featured AARP Member Benefits
Don’t Miss: Does Medicare Offer Dental And Vision
Seniors Need To Be Tenacious In Appeals To Medicare
This story was produced in collaboration with
Dan Driscoll used to be a smoker. During a regular doctors visit, his primary-care physician suggested that Driscoll be tested to see if he was at risk for an abdominal aortic aneurysm, a life-threatening condition that can be linked to smoking. The doctor said Medicare would cover the procedure. So Driscoll, 68, who lives in Silver Spring, had the test done and was surprised when he got a bill from Medicare for $214.
I didnt accept that, he said, because based on everything he had read from Medicare, he was sure this was a covered service. So Driscoll did something that seniors rarely do: He filed an appeal.
Of the 1.1 billion claims submitted to Medicare in 2010 for hospitalizations, nursing home care, doctors visits, tests and physical therapy, 117 million were denied. Of those, only 2 percent were appealed.
Few seniors have the patience, tenacity or health to question a coverage denial, say advocates and counselors in the Washington area. And those who do appeal but lose on the first try tend to give up too soon, they say.
People lose, and then they lose heart, or they are too sick, too tired or too old, and they give up, said Margaret Murphy, associate director of the Center for Medicare Advocacy, which has offices in Washington and Connecticut. Or their kids are handling the appeal and they are too overwhelmed caring for Mom or Dad.
How To Appeal A Denial Of Medicare
This article was written by Jennifer Mueller, JD. Jennifer Mueller is an in-house legal expert at wikiHow. Jennifer reviews, fact-checks, and evaluates wikiHow’s legal content to ensure thoroughness and accuracy. She received her JD from Indiana University Maurer School of Law in 2006.There are 19 references cited in this article, which can be found at the bottom of the page. This article has been viewed 8,533 times.
There are five levels of Medicare appeals for Medicare Parts A and B . Begin with an initial request to your plan for a redetermination. If you are unhappy with the result, then you can continue to appeal all the way up to a federal district court. To bring a successful appeal, you should gather supporting documentation and seek any assistance provided by a doctor or advocate. The process for appealing a Medicare Prescription Drug Plan is somewhat different at the start of the appeals process.
Also Check: How Do You Qualify For Medicare Part A And B
How Are Medicare Part B Premiums Determined
To determine monthly premiums, Social Security uses a sliding scale called IRMMA: income-related monthly adjustment amount. If you receive Social Security benefits, the premium comes directly from your SSI check. If you do not receive SSI yet, Social Security sends you a bill for the extra amount.
Medicare Part B has a base premium of $135.50 in 2019 . However, if your modified adjusted gross income is above a certain threshold, you likely pay more. Social Security bases IRMMA on your reported income from two years ago. So, in 2019, you need to look at your income tax return for the year 2017.
How To Win An Appeal
In filing an appeal, a person may benefit from gathering information to support their case. This information is generally available from a persons doctor, prescribed drugs supplier, or other healthcare providers.
To prevent lost documents, people can write their Medicare number on each one they include in an appeal request. It may also be helpful for them to keep copies of everything they submit in an appeal.
There are five levels in the appeal process, so if someone disagrees with a decision, they may go on to the next level. The decision at each level includes instructions on proceeding to the next level, up to the fifth and final level.
Also Check: How Much Does Medicare Part B Cost At Age 65
What Is Modified Adjusted Gross Income
Your modified adjusted gross income includes the adjusted gross income you reported to the IRS as well as your income from tax-exempt interest. If you filed your 2017 income taxes under Form 1040, your adjusted gross income is on line 37. Tax-exempt interest is found on line 8b.
Add the amounts on lines 37 and 8b to determine your modified adjusted gross income. You also need to know your filing status. Option 1 includes single, head-of-household, and qualifying widow or widower with a dependent child. Option 2 is married filing jointly and option 3 is married filing separately.
Once you know your filing status and your MAGI, find your premium on the following table. If Social Security decides you owe a higher premium, you will receive notification that includes the amount and the reason. You may appeal this decision.
Medicare And Hospital Coverage: Observation Versus Inpatient Status
One thing a Medicare beneficiary will in their life) experience is a hospitalization. They must be sure they have not been the victim of an improper admission classification by a doctor. It is important because even though a hospital visit may be covered under Medicare, how it is classified will determine any subsequent benefits the patient may receive, including, but not limited to, care received in a skilled nursing facility. So, if you get nothing out of this discussion, always remember to Be Aware of Your Care! Your pocketbook, and your family, will thank you for it.
Don’t Miss: How To Get A Medicare Number As A Provider
Enlist The Help Of Your Medicare Insurance Agent
If you purchased your Medicare-related insurance policy through an insurance agent, reach out to that agent for help. Not all agencies help their policyholders with appeals but some will coach them on best practices.
Finally, remember that even the ones that do, like our agency, cant guarantee that you will always win. You can however give yourself the best chance by following the simple tips outlined here today and using any resources available to you.
If youd like to learn more about our Client Service Team, dont hesitate to contact us. Our agency is happy to coach our existing policyholders with how to file appeals and what things to say or do to give yourself the best chance.
While we cannot assist individuals who did not enroll through us, we hope the tips in this blog post will help non-clients with how to go about appeals on their own.
Things To Know When Filing An Appeal

Read Also: Can Medicare Take Your House
How Do I Appeal If I Have Medicare Advantage
Medicare Advantage plans also known as Part C which bundle Medicare Parts A, B, and, usually, D together, are alternative ways to get Medicare benefits. Medicare Advantage plans are sold by private insurers that Medicare approves. Just like with original Medicare, you have the right to ask these plans to provide or pay for items or services you think should be covered, supplied, or continued. This request begins the appeals process for Medicare Part C. The plans decision is called an organization determination.
In some cases, your treating doctor can begin a dispute by requesting an organization determination or certain pre-service reconsiderations without being appointed as your representative. If the doctor needs to pursue a higher level of appeal, you will need to submit an Appointment of Representative form. There are provisions in the law for a standard or fast appeal.
This appeals process follows five levels that are similar, but not identical, to original Medicare:
Level 1: Reconsideration from the plan
Level 2: Reconsideration determination by an Independent Review Entity
Level 3: Decision by the Office of Medicare Hearings and Appeals
Level 4: Review by the Medicare Appeals Council
Level 5: Judicial review by a federal district court
Level 5 Appeal: Federal District Court Civil Lawsuit
If you disagree with the MAC’s Level 4 Decision and the amount in controversy is at least $1,350 , you can file a civil action in your local federal district court. Your lawsuit must be filed within 60 days of receiving the unfavorable MAC Decision. This is the last level of appeal available to you. The MAC’s Notice of Decision will give you information about filing a lawsuit, but as this is a formal court proceeding, you should probably hire a Medicare lawyer to help you file the lawsuit.
Also Check: What Age Do You Draw Medicare
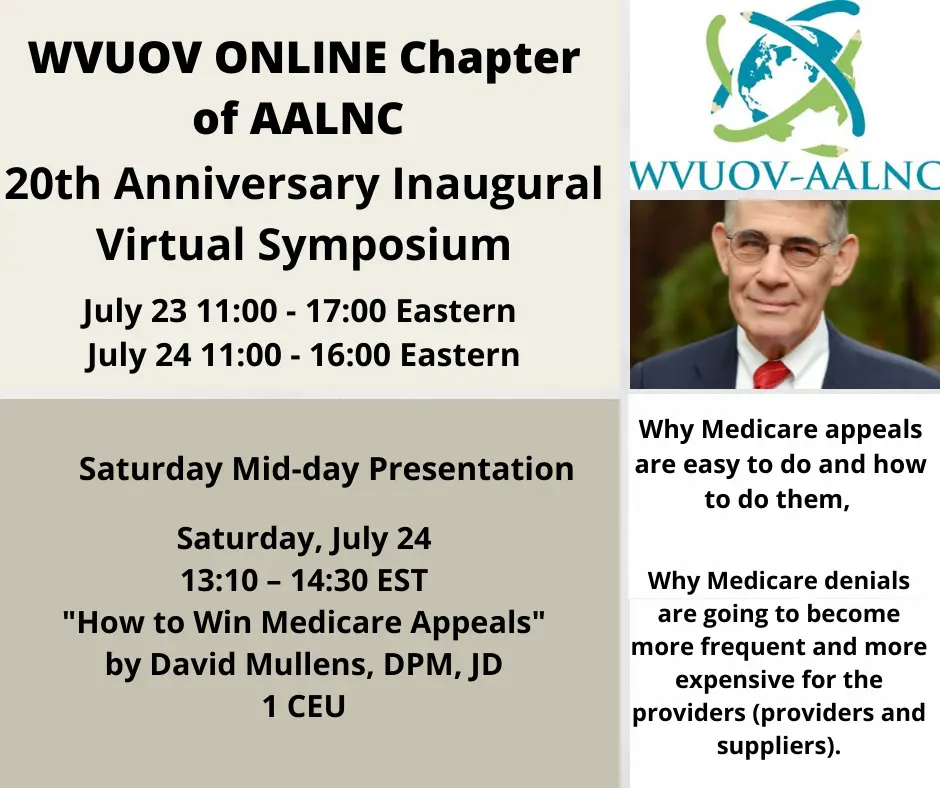
How Can Podiatrists Win Medicare Appeals
The fact is getting denied payment on a service by Medicare is a very stressful incident for a Podiatrist. Medicare for most Podiatrists is their lifeline for staying in business and earning a living. How do you appeal Medicare as a Podiatrist? Medicare already treats Podiatrists as second class citizens. Needless to say there is not a single article or 2,000 words that can teach a Podiatrist how to fight and win a Medicare appeal.
Finally someone that has gone through the process and is a lawyer has written how to file a Medicare appeal. So if you are a Podiatrist who is fighting and hoping to win a Medicare Appeal this is by far the best book you can read and learn from.
Why Joes Bills Got Denied
In this case, our 90-year-old client, had been discharged from the hospital into a Skilled Nursing Facility. Weakened from a prolonged illness, Joe was unable to attempt therapy. The Medicare Advantage carrier then denied payment for the Skilled Nursing Facility . Their denial stated that Joe had refused to participate in therapy that would begin his rehabilitation.
Medicare generally does not provide skilled nursing facility care for beneficiaries who are not expected to recover. It will cover up to 100 days in a SNF, with the goal being that the beneficiary can then resume normal self-care. Medicare Advantage plans follow these same rules.
It appeared Joe was refusing to try to get well, so the carrier actually did have grounds to deny the claim. However, the physical therapists notes upon which the carrier based their denial did not tell the whole story.
When Joes daughter lets call her Mrs. P called to tell us what happened, our Client Service Team stepped in. We gathered all the necessary data to launch an appeal. We directed Mrs. P to obtain copies of all the physical therapy notes from her fathers sessions. We then asked for copies of the carriers denial letter.
Read Also: Does Plan N Cover Medicare Deductible
Level 3 Appeal: Administrative Law Judge Hearing
If the Level 2 decision was not in your favor and you still disagree with the denial, you may file a Level 3 Request for Hearing with the Office of Medicare Hearings & Appeals before an administrative law judge, also called an “ALJ”. The minimum amount in controversy for a Level 3 appeal is at least $130 . The amount in controversy requirement changes annually, but it will always be indicated in your Level 2 decision.
You must file your Request for Hearing within 60 days of receiving the Level 2 Decision. OMHA and its ALJs are independent of Medicare and are part of the U.S. Department of Health & Human Services. Most hearings are held by telephone or videoconference from one of numerous remote sites. You may also have an in-person hearing at one of the four field offices if you can show the ALJ that “good cause” exists for you to appear in person. In some cases, the ALJ may decide to forgo a hearing altogether and may decide the case “on-the-record” when the evidence in the claim file supports a decision in your favor.
You should consider whether to obtain legal advice before requesting an ALJ hearing. The hearings are informal proceedings and you are not required to know the rules of evidence to present your case, so attorneys aren’t required, but having an attorney represent you can increase your chances of winning the appeal. You may also appoint a personal representative, such as a spouse, friend, caregiver, or patient advocate to appear on your behalf.
