Will Medicare Or Medicaid Cover Incontinence Products
This post is also a podcast! Click below to listen, and check out all our podcast episodes by
If youre incontinent, one major concern that you may have is how to pay for your incontinence products. To be sure, these products are expensive. Depending on the severity of your incontinence and the number and type of product you use, you may see costs between $50, or up to even $400 per month to cover incontinence supplies.
These costs can really add up and can have a huge impact on a persons finances over time, especially if you are older and living on a fixed income, or are in a low-income situation. At best, you may be depleting your savings by paying for incontinence supplies. At worst, you may be forced to choose between food & shelter or incontinence products. This may become even more dire if your incontinence is the result of an underlying condition that requires even more medical expenses.
Does Medicare Pay For Incontinence Supplies
Medicare doesnt cover any incontinence supplies. But, there are some Medicare Part C plans available throughout the country that will offer benefits for products like adult diapers. Yet, these plans are only in specific service areas.
So, in some cases, no plans with this benefit exist in your location. If there are Medicare Advantage plans in your area, youll want to review the summary of benefits to identify if coverage extends to adult diapers.
Further, in some states, Medicaid will cover incontinence supplies. But, Medicaid is a state-run program, so not all states will offer these benefits. Since Medicare wont cover incontinence supplies, Medigap wont cover adult diapers or pads either.
Do Veterans Health Benefits Cover Incontinence Supplies
If youre a veteran and your doctor has diagnosed you with incontinence, you can get coverage for adult diapers and related incontinence supplies for seniors through your VA health benefits. The VA typically handles medical supplies through the veterans Pharmacy Service.
However, the standard-issue brand might not be adequate for managing your incontinence symptoms. If thats the case, your doctor can write a prescription for your preferred brand that provides the absorbency and other features that better meet your needs. They might need to include reasons why a specific brand is better for you.
Recommended Reading: Does Medicare Pay For Oral Surgery
Q: Does An Fsa Cover Incontinence Supplies Are Incontinence Supplies Fsa Eligible
A: An FSA is a flexible spending account an account in which you can put money monthly out of pocket to use on medical expenses including supplies, deductibles, copays, etc. This money is not taxed if it is designated to be put aside. Generally incontinence products, such as pads, briefs, etc., can be reimbursed with your FSA. It is true that an FSA often will cover medical costs that private insurance will not, including a larger selection of incontinence supplies. You are more likely to qualify for reimbursement if you can prove that your incontinence supplies are for a diagnosed condition by way of a Letter of Medical Necessity from a doctor. You may be denied reimbursement for products such as briefs due to the fact that they treat only general health needs. However, it does depend on your specific program. Be sure to keep your receipts when you buy your incontinence supplies as you may be asked for proof of purchase in order to get reimbursement.
Are Incontinence Supplies Covered By Medicaid
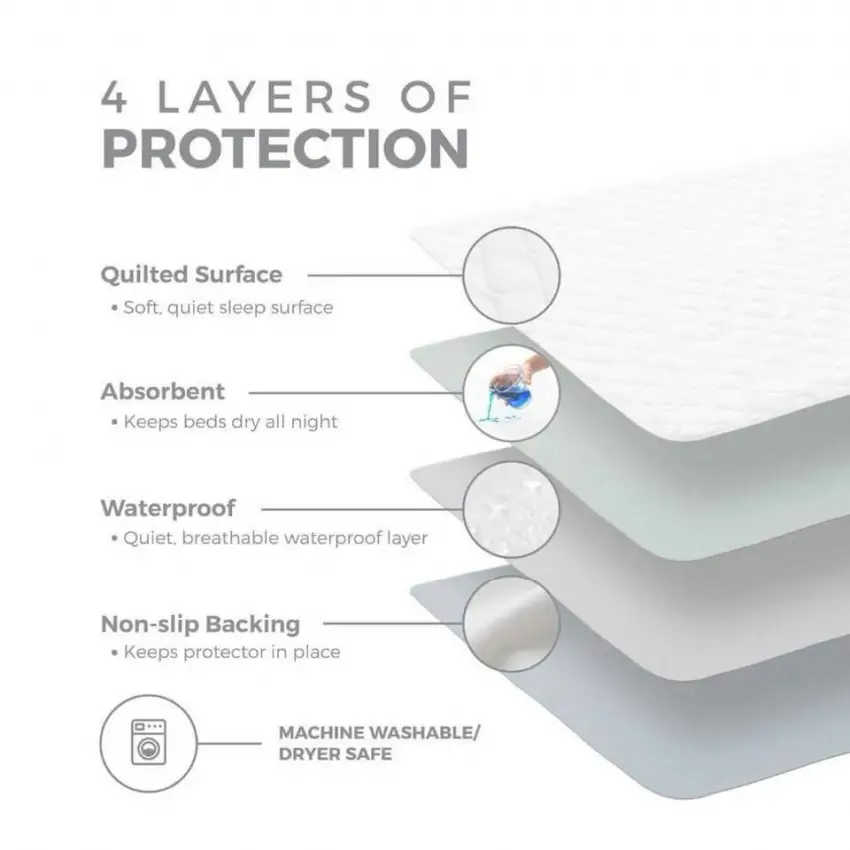
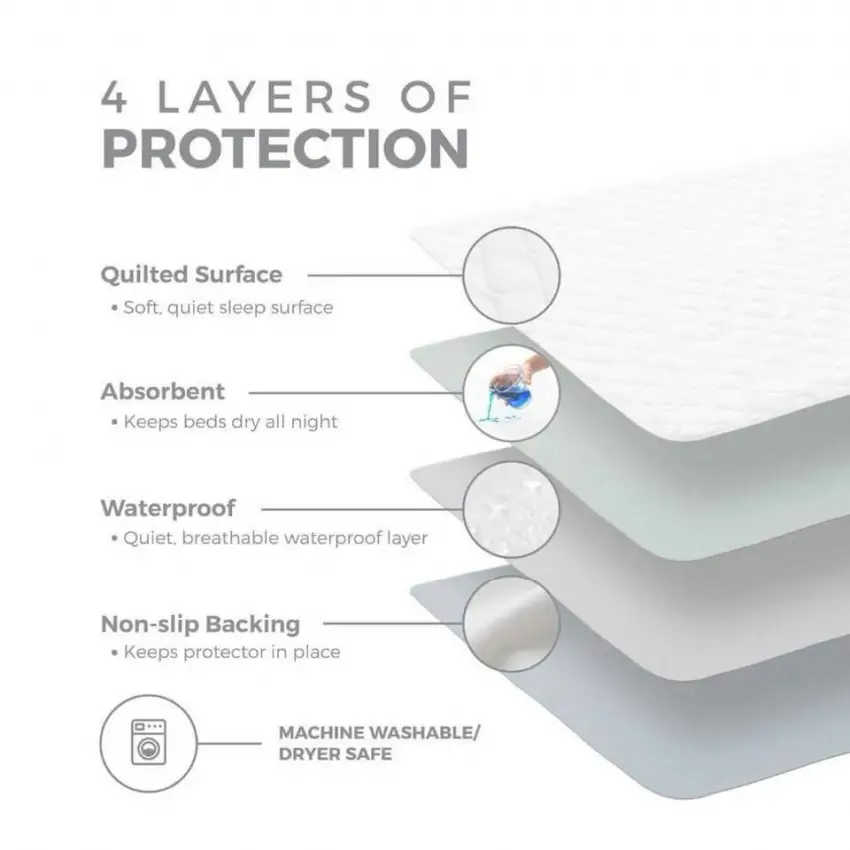
Most state Medicaid plans will cover incontinence products when prescribed by a physician for use in chronic pathologic conditions that cause incontinence to the insured individual. These incontinence supplies include disposable underpads, reusable incontinence underwear, andbladder control pads. This is an affordable way for individuals or caregivers to receive low-cost or free incontinence supplies for seniors.
Don’t Miss: Does Medicare Cover Ambulance Fees
Purchasing Incontinence Supplies Out
Can I buy my incontinence supplies out of pocket?
If your insurance plan doesnt cover incontinence supplies, you may wonder, Can I just buy my incontinence products myself? Yes, you definitely have options to buy your own supplies independent of your insurance coverage. Sometimes, it makes the most financial sense to cover the cost of your incontinence products without using insurance benefits.
Because 180 Medical is an insurance-based provider, it may make more financial sense to purchase your supplies directly from a supplier that can offer you cash-based low costs. In cases like these, were glad to offer you a solution through one of our trusted partners at Personally Delivered.
Personally Delivered offers a wide array of medical supplies, including incontinence products, skincare supplies, food and nutritional products, catheters, ostomy supplies, and more. You can purchase these supplies with your own money rather than trying to file through insurance.
You have more opportunities to save by choosing Personally Delivered when your insurance does not cover your incontinence supplies, including lower prices and their Triple Protection PLUS Program, which automatically credits you 3% on all your annual purchases.
Find out more at Personally Delivered.
How Can I Get Diapers Covered By Insurance
Some states Medicaid programs may provide coverage for these items. Medicaid requires a doctors order that adult diapers are medically necessary.
Each state has its plan for administering Medicaid, a federal/state program founded alongside Medicare in 1965 that helps those facing a financial need and/or disability regardless of age.
You May Like: Do I Have Medicare Or Medicaid
Does Medicare Cover Depends Undergarments
Depends is a well-known brand name of Adult diapers. If you need a special brand of incontinence supplies, its unlikely youll have coverage. Since insurance doesnt cover disposable supplies, these are your responsibility.
Youll pay the full cost of depends underwear unless you have a Medicare Advantage plan that covers this benefit. Also, those with Medicaid may have coverage for adult diapers, but there are most likely brand limitations.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
While Medicare wont help you pay for your Depends, some state Medicaid programs help cover the cost incontinence supplies.
Youll want to contact your state Medicaid office or the Medicare Advantage plan to identify your options. Those with Medicare and Medicaid can select a Dual-Eligible policy to increase benefits.
How Do I Get Assistance For Incontinence Supplies
While you cant make Medicare cover incontinence supplies, there are a few ways to save money. There are organizations across the United States that help with the cost of adult diapers. Further, shopping online is a great way to buy in bulk and get a discount.
Plus, shipping means you save time and gas money. Other options include couponing and free samples. The internet is your best friend when looking for deals on incontinence supplies.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
Also, some discount prescription drug cards cover medical supplies.
Recommended Reading: Do I Have To Have Part D Medicare
Q: Does Medicaid Cover Incontinence Supplies Does Florida Medicaid Cover Incontinence Supplies
A: Yes, frequently Medicaid does cover incontinence supplies. While most medicaid plans will cover incontinence supplies, it does ultimately depend on your state. However odds are good that your state is accommodating as 45 out of the 50 states cover incontinence products. This includes Texas, Florida, New York, Massachusetts, and California, to name a few. You can look at each states coverage guide, which is generally easy to find online, in order to determine if your incontinence supplies will be covered. Though there are varying requirements by state, for example the requirement for a doctor recommendation to be eligible for reimbursement.
Some Medicare Advantage Plans May Cover Incontinence Supplies
Medicare Advantage plans are alternatives to Original Medicare that are managed by private insurance companies rather than the federal government.
These extra benefits can include things like:
Medicare Advantage plan availability and benefits can vary based on your location. More than 20 million Medicare beneficiaries were enrolled in a Medicare Advantage plan in 2019. Thats equal to 34 percent of all Medicare beneficiaries!1
You May Like: Does Medicare Require A Referral For A Colonoscopy
Us Department Of Veterans Affairs
The Department of Veterans Affairs does provide adult diapers as part of its VA health benefits. But it typically provides a standard issue type of adult diaper.
If you want a brand-name product such as Depend or Attends your doctor will have to provide the VA with a prescription or a statement of medical justification explaining the medical necessity as to why you need a particular brand.
Veteran-Directed Care also called Home and Community Based Services is a VA program that provides financial assistance to veterans. Its designed to give vets the flexibility to determine how to best spend the aid on their particular needs. If you qualify, you can use the assistance toward incontinence supplies.
Challenges Of Medicaid Benefits For Getting Incontinence Supplies
One of the challenges with Medicaid is determining what is and what is not covered under a Medicaid plan, such as incontinence supplies. Due to differences by state, there is a lack of clear documentation on covered medical services and support, including incontinence supply coverage. Also, regular changes to coverage/benefits can create a headache for those receiving Medicaid, who often struggle to know all that is covered and how to make the most of their benefits. Generally, Medicaid covers medically necessary treatments, services or products for individuals who may be low-income, elderly, disabled or blind.
A common question we receive is does Medicaid cover adult diapers, pull-on underwear, bladder control products or other incontinence supplies?
The short answer is yes state Medicaid programs typically cover medically necessary incontinence supplies, such as boosters, adult diapers , pull-on underwear and underpads, including youth products, for specific Medicaid recipients. But there are some important insurance provider rules and requirements you need to know.
Read Also: What Are The Different Parts Of Medicare Plans
Are Incontinence Supplies Covered By Medicare
Incontinence Supplies and Medicare Coverage is limited, but not impossible.Despite the number of people who live with incontinence, traditional Medicare does not cover any incontinence supplies like diapers and pads. However, depending on your financial circumstances and the type of medical insurance you choose, the cost of incontinence essentials may be reimbursed or at least be a tax-deductible expense. Here are the options that may be available to you.
Childrens Health Insurance Program
CHIP is an insurance program that provides low-cost health coverage to children in families that earn too much money to qualify for Medicaid but not enough to buy private insurance. In some states, CHIP covers pregnant women. Each state offers CHIP coverage and works closely with its state Medicaid program.
CHIP generally covers incontinence products for children above the age of 3 or 4 years old with special needs. In many states, the QuickChange® Incontinence Wrap is available under CHIP. Since most state Medicaid programs administer CHIP side by side, the general Medicaid rules apply for coverage.
If you are covered under CHIP, you can see the coverage status of the QuickChange® Incontinence Wrap in your state.
Please feel free to contact us at and we can provide you with our general guidance for your particular state.
Don’t Miss: Is Eye Care Covered Under Medicare
Does Medicare Cover Incontinence Supplies
Medicare Advantage plans can offer benefits that Original Medicare doesnt cover. This means that some Medicare Advantage plans might cover incontinence supplies for qualified plan beneficiaries.
Original Medicare does not cover incontinence supplies such as adult diapers and pads, however. This means that with Original Medicare, you must pay 100 percent of the costs for your incontinence supplies.
Is There Any Help With These Costs
There are several programs that may help with costs.
The Medicaid waiver program can help community-based services provide help to people who might otherwise be in a long-term care facility. Each state may operate the program differently. People can contact their states Medicaid office to check their eligibility.
Some communities also have diaper banks that provide diapers and other supplies to people with limited incomes. In many cases, adult diapers are free, though each group has specific policies about products, services, and distribution.
Also, some families may qualify for a National Family Caregiver Support Program grant, which helps families caring for older adults. The Department of Health and Human Resources in a persons state will set the eligibility requirements.
Discount prescription drug cards may also cover medical supplies.
People who shop for adult diapers online could also buy in bulk to help lower the cost.
You May Like: Does Medicare Cover Hospice Room And Board
Letter Of Medical Necessity/prior Authorization Form
To get covered, please have your doctor complete the following form.
A Prior Authorization Form/Letter of Medical Necessity is required by most insurance providers and can be approved by any doctor or provider that is aware of your medical condition. Please bring this form to your doctor.
Prior Authorization Form
Can You Get Free Incontinence Pads
While Medicare doesn’t cover incontinence supplies except for very specific circumstances, there are ways to get these products for free or to save a lot of money on your purchases. You can do the following if you are unable to receive coverage through your Medicare Advantage plan as well.
While Medicare doesn’t cover incontinence supplies in most cases, you may be able to receive coverage through a Medicare Advantage plan or reduce your costs significantly through other assistance programs. Your doctor can help you determine if you are eligible to receive any of these benefits and provide the documentation you need for approval. It is certainly possible for you to reduce the cost of your supplies to be able to afford them.
Read Also: How To Get Prescription Coverage With Medicare
What Medicare Plans Cover Incontinence Supplies
There are some supplies that are an exception to the above. Supplies such as catheters might be covered if you provide the proper documentation. These rules apply only to traditional Medicare, so if you have a Medicare Advantage plan, you may be able to receive coverage. Some Advantage plans do provide coverage for incontinence supplies, and if yours does, you will be able to work with your doctor to gain approval.
Medicare Supplement plans won’t cover this expense. If you’re enrolled with a traditional Medicare plan or a Medicare Advantage plan that doesn’t provide coverage, you need to consider other ways to reduce the cost of your incontinence supplies.
Does Medicaid Cover Incontinence Supplies
Medicaid is a state-specific program, meaning that benefits vary between states. Its a program available to all Americans who meet state requirements and have limited financial resources. If you or your loved one qualify for Medicaid, youll receive coverage for home care products like incontinence supplies for seniors.
But keep in mind that many state Medicaid programs restrict coverage for incontinence supplies based on the brand and limit the maximum number of products covered each month. The quality brand you prefer might not be covered, and you might still need to purchase additional incontinence products yourself.
Also Check: What Is A P10 Number For Medicare
How Many Incontinence Products Can I Receive
The number of continence care products available to you through insurance will depend on both your insurance plan as well as the needs determined by your healthcare provider. Your doctor or urologist will recommend a maximum quantity of products needed based on your level of incontinence as well as your estimated frequency of changes.
Based on that recommendation, companies such asAeroflow Urologywill work with your insurance to help you receive the maximum number of allowable products based on your needs. This number will often vary based on the product type that you will be utilizing.
What Is Urinary Incontinence
Urinary incontinence is the accidental loss of urine. It can happen at any age but is most common in women over age 50. In some cases, its a temporary condition that results from an underlying medical condition, and in other cases it can be permanent. Severity can range from slight loss of urine to severe, frequent wetting.
While incontinence is not an inevitable result of aging, it is often caused by specific changes in body function resulting from diseases, use of certain medications, and/or the onset of an illness.
Some examples of incontinence products one may purchase include protective pads, shields, diapers, and specifically designed absorbent underclothing.
You May Like: Which Medicare Plans Cover Silver Sneakers
Does Medicare Cover Incontinence Supplies In Nursing Homes
If you reside in a nursing facility and your health care provider is able to document a need for incontinence treatment, Medicare Part A may cover your incontinence supplies. This is because Medicare Part A covers inpatient care, and those supplies are considered a necessity for your ongoing treatment. Medicare Advantage plans are required to provide coverage for anything covered under Medicare Part A or B, which means your Medicare Advantage plan should also provide coverage.
Does Medicare Help Pay For Incontinence Supplies
While Original Medicare doesnt cover incontinence supplies, some Medicare Advantage plans provide a monthly or quarterly stipend to purchase over-the-counter supplies like adult diapers. Your plan determines if you must order through the Medicare supply catalog.
Medicare Advantage combines the benefits of Original Medicare . Along with including Part A and B benefits, Medicare Part C often bundles additional services like dental, hearing, vision and prescription drug coverage.
Recommended Reading: Is Balloon Sinuplasty Covered By Medicare
Medicare And Adult Diapers
Does Medicare pay for adult diapers? This seems to be the first question most seniors ask. Unfortunately, for the vast majority of seniors living outside of nursing homes, Medicare does not pay for adult diapers. There are a few other incontinence supplies that are covered, such as catheters. But disposable absorbent products are largely, if not entirely, the financial responsible of the individual. Unfortunately, Medicare Supplemental Insurance, sometimes called Medigap policies, also do not cover these supplies.
In Europe, there are long duration adult diapers that last 8 hours, 3x longer than normal. There are also diaper liners that can double the duration. Both can be purchased online.
