What Is The Income Range For Beneficiaries Who Are Dual Eligibles
Generally, beneficiaries earning less than 135 percent of the federal poverty level are eligible for the MSP if they also have limited savings . This equates to $17,226 annually for single beneficiaries and $23,274 for married couples. Beneficiaries qualify for full Medicaid benefits if their incomes and assets are even lower .
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances. It is also common for Medicare beneficiaries who are under 65 and live on Social Security Disability Insurance to receive Medicaid benefits.
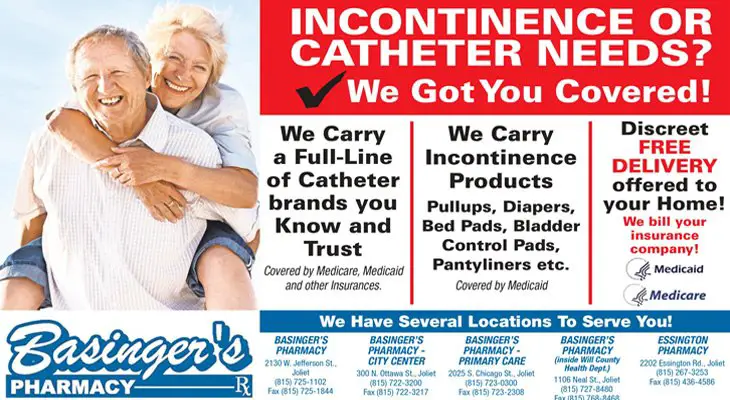
Medicare Coverage Of Related Supplies
While Medicare does not cover incontinence supplies, it does help cover external catheters for beneficiaries with urinary incontinence or urinary retention. Medicare coverage can also extend to related supplies such as drain bags, irrigation kits, leg bags and extension tubing.
Because Medicare Advantage plans are required by law to cover all of the same services and items included in Original Medicare, Humana Medicare Advantage plans will also provide coverage for catheters and related supplies that would otherwise be covered by Original Medicare.
Contact a licensed insurance agent for more information about Humana Medicares coverage of incontinence supplies and how to enroll in a plan available where you live.
Insurance Coverage For Incontinence Supplies
Are incontinence supplies covered by Medicaid? What type of incontinence supplies will my insurance reimburse for? Does my insurance cover incontinence supplies? Does Medicare cover diapers or underpads?
Its common to have questions like this. After all, you want to make sure youre using your insurance benefits to the fullest.
The good news is that many plans do cover incontinence supplies. Find out more with our handy insurance guide below. Plus, we provide some helpful alternate options for getting your supplies when your insurance doesnt cover the products you need.
Don’t Miss: Does Medicare Pay For Foot Care
What Other Pain Management Do Humana Plans Cover
Acupuncture is just one of the pain treatments that may be covered by a Humana Medicare Advantage plan. Many plans also cover:
- Prescription pain relieving drugs
- Memberships to health and fitness programs such as SilverSneakers that may help manage pain
Humana may also offer Medicare Advantage Special Needs Plans where you live, which are plans that are specifically tailored to a particular chronic health condition and may offer more focused coverage for pain or other symptoms of chronic diseases.
Why Do I Need Inr Regularly
No doubt, the INR test can be used for other several purposes. However, it is specially designed to help monitor if a particular prescribed anticoagulant drug is active. Most prescribed anticoagulant is Warfarin, commonly known as Coumadin. The prescription is meant to tackle abnormalities in blood clotting, which usually forms in the legs and lungs. The drug thins the blood, leading to reduced risk of stroke, heart attack, and other severe cardiovascular complications.
Therefore, it is crucial that you regularly check the effect of this drug to avoid any health issues due to the intake of the medication. The INR test monitors your wellness, ensuring you take the right dosage without leading to excessive bleeding.
Don’t Miss: Does Medicare Cover Companion Care
How Do I Use The Otc Allowance
1. See if your Humana plan offers an OTC allowance
If your plan includes the OTC benefit allowance, youll see an OTC credit in the top-right corner of the page when you . This is the amount you can spend in one month or quarter
Depending on your plan, your allowance may expire at the end of each month or quarter or roll over to the next month or quarter through the end of your plan year.
2. Order your OTC products in a few easy steps
Ordering online in the OTC store or shopping in the Humana Pharmacy Mobile app is the fastest way to buy OTC products.
3. Enjoy free shipping on every order
Once your order is processed, your items will ship and should arrive in 1014 days.
Veterans Administration Health Care
The VA is one 3rd party that provides help. While the VA does pay for adult diapers, many veterans advise caution with regards to the quality. Specifically, the standard issued brand of adult diapers is not considered to be of high quality. However, if a veteran has a preferred brand, such as Attends, Depend, Prevail, Tena or Tranquility, it is possible to have those paid for by the VA. However, a physician prescription or statement of medical justification that explains the medical reasons for which a particular brand of adult diaper is required is necessary.
You May Like: Does Medicare Cover The Cost Of A Shingles Shot
Medicare Advantage Plans May Cover Catheters
Medicare Advantage plans are sold by private insurance companies and are required by law to cover everything that Part A and Part B cover.
If your catheter is covered by Original Medicare, it will also be covered by a Medicare Advantage plan.
Most Medicare Advantage plans offer prescription drug coverage. Some Medicare Advantage plans also offer additional benefits, such as:
Is There Any Help With These Costs
There are several programs that may help with costs.
The Medicaid waiver program can help community-based services provide help to people who might otherwise be in a long-term care facility. Each state may operate the program differently. People can contact their states Medicaid office to check their eligibility.
Some communities also have diaper banks that provide diapers and other supplies to people with limited incomes. In many cases, adult diapers are free, though each group has specific policies about products, services, and distribution.
Also, some families may qualify for a National Family Caregiver Support Program grant, which helps families caring for older adults. The Department of Health and Human Resources in a persons state will set the eligibility requirements.
Discount prescription drug cards may also cover medical supplies.
People who shop for adult diapers online could also buy in bulk to help lower the cost.
You May Like: How Can I Get My Medicare Card Number
Gaining And Reclaiming Confidence And Comfort
Though incontinence represents a change in lifestyle, it doesnt have to be a stumbling block for you and your loved one. By shopping smart, you can introduce products and tools to help you and your loved one continue to lead a happy and active life. Youre not alone, and there are plenty of products available to help your loved one take control of incontinence and continue to live life to the fullest.
How Do I Know If I Should Be Dual Eligible
Beneficiaries can find out if theyre eligible for Medicaid by contacting their Medicaid office. An Internet search for Medicaid offices in a beneficiarys state should provide the number to call but beneficiaries should make sure they are contacting a government office before sharing any personal information.
The Centers for Medicare and Medicaid Services also maintains a list of state agencies that oversee Medicaid. Beneficiaries can see if they already have Medicaid by contacting 1-800-MEDICARE and asking whether they receive Extra Help with their prescription drug costs .
Read Also: How To Change Primary Doctor On Medicare
Bariatric Surgery For The Treatment Of Urinary Incontinence In Obese Women
In a meta-analysis, Zhang and colleagues examined the effectiveness of bariatric surgery in obese women with UI. Searches of PubMed, the Cochrane Library, and Embase databases were performed using “weight loss surgery/bariatric surgery/gastric bypass surgery” and “incontinentia urinae/uracratia/urinary incontinence/uroclepsia” in the title/abstract before January 2018. Then, meta-analysis was analyzed by Review Manager 5.3 . The SMD and OR were used to describe results of continuous variables and dichotomous variables, respectively. Pooled data showed that bariatric surgery reduced the incidence of UI in obese women at the follow-up of 6 months and 12 months and significantly reduced the BMI at 6 months and 12 months . In addition, bariatric surgery could also significantly increase the QOL and improve the function of pelvic floor disorders based on QOL questionnaires and Pelvic Floor Distress Inventory 20, respectively. The authors concluded that this meta-analysis demonstrated that bariatric surgery is an effective choice for obese women with UI however, more RCTs are needed to confirm these findings.
Furthermore, UpToDate reviews on Treatment of urinary incontinence in women and Treatment of urgency incontinence/overactive bladder in women do not mention bariatric surgery as a therapeutic option.
Medicare Coverage For Incontinence Supplies

Medicare is a health insurance program provided through the United States federal government by the Centers for Medicare and Medicaid Services . They cover millions of people who qualify for coverage every year.
In order to qualify for Medicare, you must be an American citizen or a permanent legal resident who is 65 years or older or under 65 and living with a disability or receiving Social Security benefits.
Medicare has 4 parts of insurance coverage:
- Hospital insurance coverage under Medicare Part A
- Medical insurance coverage under Medicare Part B
- Medicare Advantage plan options, known as Medicare Part C
- Prescription drug coverage under Medicare Part D
Does Medicare cover adult diapers and/or other incontinence supplies?
No. While Medicare covers intermittent catheters and ostomy supplies, they typically do not cover incontinence supplies. For example, non-covered items include diapers, mattress-protecting underpads, and bladder control pads or liners.
However, you may have options through a private insurance companys Medicare Advantage plan.
Recommended Reading: Is A Walk In Tub Covered By Medicare
Does Medicare Cover Catheters
Medicare Part B may cover catheters, but usually only if it is due to a permanent condition and under certain circumstances, such as during hospice care.
A catheter can be used to relieve symptoms related to urinary retention, urinary incontinence, prostate or genital surgery and various other medical conditions.
Medicare Advantage plans may also cover catheters that are deemed medically necessary by your doctor.
Does Medicare Cover Nursing Homes And Long
Medicare generally doesnt cover the cost of a nursing home, assisted living or long-term care facility. Medicare Part A does cover care provided in a skilled nursing facility with certain conditions and time limitations.
If you qualify for it, Medicaid, which is administered by states under federal guidelines, may cover nursing home care. You may need to exhaust your personal resources on medical care before you are eligible.
You May Like: When Does Medicare Coverage Start
Screening For Urinary Incontinence In Women
Despite the lack of studies determining the benefits and harms of UI screening, the Women’s Preventive Services Initiative recommended that doctors screen women of all ages, including adolescents, for UI yearly by using a questionnaire. The WPSI recommended referring women with UI for further evaluation if it affects their activities and QOL. These recommendations were based on indirect evidence that UI is common, treatment may be effective, and the harms of screening are unlikely to be serious. The recommendations might change if studies directly evaluating the benefits and harms of screening for UI become available. There are no data to support that the correct frequency of screening is yearly .
How Does The Bladder Work
The bladder stores urine until it gets a signal from the brain to empty. Sphincter muscles control whether the bladder is closed or open. When the bladder is closed, the sphincter muscles are also closed around the tube, called the urethra, that allows urine to exit the body.
When a person is ready to urinate, a signal goes from the brain to the bladder, which contracts and allows the urine out through the urethra.
People may be able to control urine leakage with medication or physical therapy.
Recommended Reading: What Age Does Medicare Eligibility Start
Humana Walmart Value Rx Plan
Under the Humana Walmart Value Rx Plan, Humana teams up with Walmart, Walmart Neighborhood Markets, and Sams Club pharmacies as its preferred cost-sharing partners.
This lets Humana offer additional prescription savings to people who purchase their medications at Walmart.
The Humana Walmart Value Rx Plans benefits include:
- $17.20 monthly plan premium nationwide
- $0 deductible on tier 1 and 2 medications
- $445 annual deductible on tiers 3 through 5 medications
- in-store copays as low as $1 on a 30-day supply of certain generic drugs at Walmart, Walmart Neighborhood Markets, and Sams Club
- copays as low as $3 on a 90-day supply of tier 1 preferred generics through Humanas mail-delivery pharmacy
- more than 3,500 medications on the plans list of covered drugs
Before choosing the Humana Walmart Value Rx Plan, make sure you live near a Walmart location that features pharmacy services. While you are able to use other pharmacies under this plan, you wont get additional discounts if you dont use Humanas preferred cost-sharing partners.
Medicare And Incontinence Supplies
For most adults, going to the bathroom is something that can be easily postponed. But for the millions of Senior Americans suffering from incontinence, delaying that trip to the bathroom can be difficult if not impossible.
One in five people over the age of 40 suffer from an overactive bladder and sometimes leak urine even before reaching the bathroom, this according to the National Association for Continence. This number rises significantly in the senior population.
At least 50 percent of residents in a nursing home suffer from incontinence. The cost of purchasing adult diapers can prove to be a heavy burden with incontinence supplies estimated to reach $900 to $4,000 per year.
Having coverage for incontinence supplies can be a very attractive option for those with Medicare. The next question is, does Medicare cover incontinence supplies?
The disappointing news is traditionalMedicare does not cover incontinence supplies or adult diapers. This includes products such as adult briefs, underpads, adult diapers, bladder control pads, and guards. However, these supplies can be covered under a different medical insurance plan or at least be considered a tax-deductible expense depending on a persons financial circumstances.
Also Check: What Is Retirement Age For Medicare
The Above Policy Is Based On The Following References:
What Changes Should I Expect

As your infant grows, feeding will change. Babies will start drinking more milk during each feeding, so they won’t need to feed as often and will sleep longer at night.
Your baby’s appetite will increase during growth spurts. Continue to feed on demand and increase the number of feedings as needed.
Your infant also will become more alert as the weeks go by, cooing and smiling. So there probably will be more interaction between you and your baby during feedings.
The following are general guidelines, and your baby may be hungrier more or less often than this. That’s why it’s important to pay attention to your baby’s signals of being hungry or full. A baby who is getting enough might slow down, stop, or turn away from the breast or bottle.
Also Check: When Can I Get My Medicare
Billing Protections For Qmbs
Federal law forbids Medicare providers and suppliers, including pharmacies, from billing people in the QMB program for Medicare cost sharing. Medicare beneficiaries enrolled in the QMB program have no legal obligation to pay Medicare Part A or Part B deductibles, coinsurance, or copays for any Medicare-covered items and services.
Despite the federal law, our July 2015 study found that those in the QMB program were still being wrongly billed and that confusion about billing rules continued. We have taken several steps since to help Medicare providers and beneficiaries better understand the QMB protections, including through many of the resources below.
How Are My Health Care Costs Reimbursed If I Have Medicare And Medicaid
When dual eligible beneficiaries have healthcare expenses, Medicare pays first and Medicaid pays last. But this is not the case for things Medicare doesnt cover, like long-term care. If Medicaid is covering a beneficiarys long-term care, Medicare will still be the primary payer for any Medicare-covered services like skilled nursing care or physical therapy.
Although it is less common, if a dual eligible individual has additional coverage then Medicare pays first, Medigap will pay second, and Medicaid is the last payer for their claims .
Also Check: Will Medicare Pay For A Roho Cushion
When Do Humana Medicare Plans Pay For Acupuncture
Medicare Part B covers 12 acupuncture visits within a 90-day period for chronic lower back pain. If improvement is shown at the conclusion of the 12 visits, Medicare may cover an additional 8 sessions. No more than 20 visits may be covered within the same calendar year.
Humana Medicare Advantage plans are required to cover at least the same level of acupuncture care as Medicare Part B covers. Some Humana plans may cover even more acupuncture visits for a longer period of time, but you should check with your plan directly to learn more.
For example, some Humana Medicare plans may cover up to 25 acupuncture sessions per year with a $0 copay, which is more than the maximum of 20 covered by Original Medicare. This is just one example of a Humana Medicare Advantage plan that goes above and beyond the acupuncture coverage offered by Original Medicare.
Medicare Part B does not cover acupuncture for any other condition besides chronic lower back pain. Medicare defines chronic pain as pain that:
- Persists for at least 12 weeks
- Has no known cause and is not related to inflammation, cancer or infectious disease
- Is not associated with surgery or pregnancy
A Humana Medicare Advantage plan may feature a lower deductible or coinsurance amount, so be sure to check with your plan provider or call to speak with a licensed insurance agent to find out more about how much acupuncture costs with a Humana Medicare plan.
