Medicare Savings Programs Income And Resource Limits
Your income and resources are some of the factors that Medicaid uses to determine if you qualify for help with Medicare premiums. MSPs have different monthly income limits, and most states have the same limits. Alaska and Hawaii are the only two states that have different income limits. Three of the four MSPs have the same resources limits, and these limits are the same for all states including Alaska and Hawaii. If you earn equal to or less than these limits, then you may qualify for assistance.
| Program Name |
|---|
How Can Medicare Savings Programs Help
Medicare Savings Programs are intended to help individuals with limited income and resources pay their Medicare premiums and other out-of-pocket costs while retaining their Medicare coverage. For the purposes of MSPs, countable resources include financial accounts such as checking and savings, stocks, and bonds. Resources that don’t count include:
- Burial plot and up to $1,500 in funds put aside for burial expenses
- Household and personal items
MSPs are administered by at the state level but are federally funded. There are several programs available, and each one has different income and asset limits that you need to meet in order to qualify. Please note that all limits are slightly higher in Alaska and Hawaii.
A brief summary of programs that pay the Part B premium is as follows:
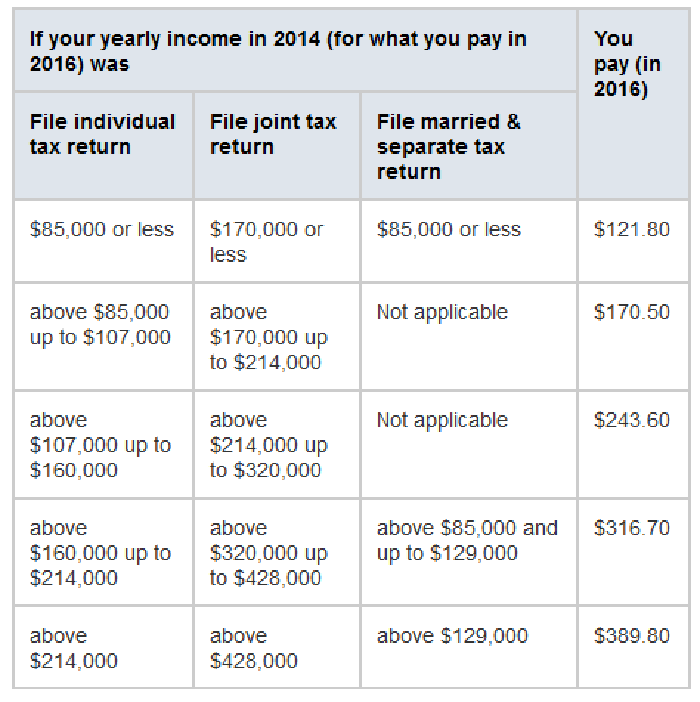
Does My Income Affect My Monthly Premiums For Medicare
If you are what Social Security considers a higher-income beneficiary, you pay more for Medicare Part B, the health-insurance portion of Medicare.
Medicare premiums are based on your modified adjusted gross income, or MAGI. Thats your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS. To set your Medicare cost for 2021, Social Security likely relied on the tax return you filed in 2020 that details your 2019 earnings.
If your MAGI for 2019 was less than or equal to the higher-income threshold $88,000 for an individual taxpayer, $176,000 for a married couple filing jointly you pay the standard Medicare Part B rate for 2021, which is $148.50 a month. At higher incomes, premiums rise, to a maximum of $504.90 a month if your MAGI exceeded $500,000 for an individual, $750,000 for a couple.
You can ask Social Security to adjust your premium if a life-changing event caused significant income reduction or financial disruption in the intervening tax year for example, if your marital status changed, or you lost a job, pension or income-producing property.
Youll find detailed information on the Social Security web page Medicare Premiums: Rules for Higher-Income Beneficiaries.
Read Also: Does Medicare Part D Cover Shingrix Vaccine
What Doesnt Count As Income And Resources
Federal law requires that states exclude certain types of assets. These are some of the main things that dont count:
| Doesnt Count as a Resource |
|---|
| Primary house |
| Items that cannot be easily converted to cash such as furniture and jewelry |
| Burial plot and burial funds valued up to $1,500 for individuals and $3,000 for couples |
| Life insurance that has less than $1,500 in cash value |
Understanding Medicare And Medicaid
Medicare is health and hospitalization insurance for people age 65 and older and those under 65 with certain disabilities or end-stage renal disease. Some portions of Medicare are free and others cost money, with premiums typically deducted from your Social Security benefit checks.
Even if you have private insurance you should apply for Medicare. If you wait until after your 65th birthday to apply, you may end up paying a late penalty or higher premiums. For most people, the initial enrollment period is the seven-month period that begins three months before the month in which they turn 65. If you miss that window, you may enroll between January 1 and March 31 each year, although your coverage wonât begin until July 1.
There are four types of Medicare coverage available.
Read Also: Is Humana Medicaid Or Medicare
What If Im Also Enrolled In Medicaid
If you are enrolled in both Medicare and Medicaid at the same time, then Medicaid will pay your Part B premiums. If you are enrolled in Medicaid and Medicare, you will also automatically be eligible for enrollment in some Medicare Savings Programs.
Medicaid can also provide other forms of assistance aside from the Part B premium, including help with Part D and secondary insurance coverage. To coordinate these benefits and make sure that you are getting as much coverage as you can, you should contact your local Medicaid office.
If you are already enrolled in Medicaid before you enroll in Medicare, you should contact Medicaid as early as you can to make sure that your premiums are covered before you are billed. This also ensures proper billing and payment of your Medicare claims.
When Is The Best Time To Apply For A Medicare Savings Program
You can enroll in a Medicare Savings Program at any time during the year. Enrolling during your Initial Enrollment Period will make things easier because it ensures that you donât have to pay premiums at any point during your Medicare coverage. Initial Enrollment lasts for seven months. It includes three months before your birthday month, your birthday month itself, and three months after. You should try to enroll in a savings program as early as possible during this period.
Also Check: How Do I Get A Second Opinion With Medicare
Medicare Premium Assistance: What Options Are Available
The Centers for Medicare and Medicaid Services provide assistance with premium payments. Medicaid operates four types of Medicare Savings Programs:
- Qualified Medicare Beneficiary
- Qualified Disabled and Working Individual
Most of the help you can get to pay premiums are available through these programs.
Does Medicaid Cover Nursing Homes
Yes, Medicaid covers nursing home costs if you qualify. Medicaid is the largest fund-source for nursing home care. For eligible seniors, Medicaid covers long-term nursing home care in Medicaid-certified facilities4 when medically necessary. Youll have to be under a certain income level and meet other state-specific requirements to qualify.5
All 50 states offer Medicaid, but nursing home services, cost coverage, and eligibility requirements vary widely by state. For example, New York has a Medicaid income limit of $10,600 for individuals age 65+ with a family size of one6 while Mississippis limit is $2,382. Not all nursing homes accept Medicaid, so check with each facility.
Unlike Medicare, Medicaid does not impose an official time limit on nursing home stays as long as theyre in a licensed and certified Medicaid nursing facility.
What Is Covered by Medicaid
- Long-term care covers nursing home stays for qualifying patients needing ongoing care for a chronic mental or physical condition.
- Skilled nursing and related medical care.
- Rehabilitation from illness, injury, or disability.
Don’t Miss: When Is The Next Medicare Open Enrollment
Is There Financial Help For Medicare Part D Coverage
Medicare offers Extra Help for Medicare enrollees who cant afford their Part D prescription drug coverage. If youre a single person earning less than $1,630 per month , with financial resources that dont exceed $14,790 , you may be eligible for Extra Help . The program will reduce or eliminate your Part D plans premium and deductible, and also lower the cost of prescription drugs to a very small amount.
Heres more information about Extra Help, including details about the type of notice you might receive from Medicare or Social Security, that you can then send to your Part D plan.
Cdc Shingles Vaccine Recommendations
The Centers for Disease Control and Prevention recommends Shingrix vaccination for anyone 50 years and older, even if you have already had shingles, if you had another type of shingles vaccine, and if you dont know whether or not youve had chickenpox in the past.
You should not get the vaccine if you are allergic to any of the components, are pregnant or breastfeeding, currently have shingles, or you have lab tests that definitively show that you do not have antibodies against the varicella-zoster virus. In that case, you may be better off getting the varicella vaccine instead.
Also Check: Does Medicare Cover Freestyle Libre Sensors
Medicare Premium Assistance Program
This program helps people eligible for Medicare who have limited income and assets get help in paying the cost of one or more of the following:
- Medicare premium
- Medicare copays
To qualify for MPAP, applicants must be eligible for Medicare and meet basic requirements.
When applying for MPAP, proof of income, resources, age or disability, citizenship or non-citizen status, and other health insurance is required.
No face-to-face interview with the local County Department of Job and Family Services is necessary. Applicants can ask an authorized representative to apply on their behalf.
Qualified Medicare Beneficiary Program
Helps pay for: Part A premiums Part B premiums, deductibles, coinsurance, and copayments .
Monthly income and resource limits for 2022:
| Your situation: |
|---|
* Limits slightly higher in Alaska and Hawaii
If you qualify for the QMB program:
- Medicare providers arent allowed to bill you for services and items Medicare covers, including deductibles, coinsurance, and copayments. What to do if you get a bill
- You may get a bill for a small Medicaid copayment, if one applies.
- You’ll also get Extra Help paying for your prescription drugs. Youll pay no more than $4 in 2022 for each drug covered by your Medicare drug plan.
Don’t Miss: What Is Medicare Part G
How Much Does It Cost Each Month For Me To Have Original Medicare
How much you have to pay for your Medicare coverage each month depends on your work history. Most people with Medicare get their hospital insurance premium free. If you do not have enough work history , you will have to pay a monthly premium for Part A. Everyone has to pay a monthly premium for their medical insurance . Costs generally go up every year.
For Part A, each month you will pay:
- Nothing if you or your spouse worked and paid Medicare taxes for 10 years or more in the U.S.
- $226 if you or your spouse worked and paid Medicare taxes between 7.5 and 10 years in the U.S.
- $411 if you or your spouse worked and paid Medicare taxes for fewer than 7.5 years in the U.S.
For Part B, each month you will pay:
- A $121.80 premium each month if your annual income is below $85,000 .
People with high incomes have a higher Part B premium.
How much you will pay for services each month depends on which services you receive and whether you go to a doctor who accepts the Medicare-approved amount as payment in full .
Paying For A Prescription Drug Plan
If you qualify for theQMB, SLMB or QI Medicare Savings Programs, then you also automatically qualify for a program called Extra Help designed to help with paying for your prescription drugs. Prescription drug coverage is provided through Medicare Part D, which is why Extra Help is also known as the Part D Low-Income Subsidy. Part D coverage generally comes with a premium, a deductible and a copayment or coinsurance. Learn more about Medicare Part D here.
But you dont have to be in a Medicare Savings Program to receive help paying for your prescriptions under Extra Help. If your annual income as an individual is up to $1,698 per month or $2,288 as a couple in 2022, you may be eligible. Asset limits in 2022 are up to $15,510 for an individual or $30,950 for a couple.
Depending on which Medicare Part D plan you choose, the program can reduce or eliminate your plans premium and deductible, and also lower the cost you pay for the prescription drugs covered under your plan.
Don’t Miss: Does Medicare Pay For Glucometer
How To Get A Free Mobility Scooter Through Medicaid
Many states use the Medicare payment rates when they cover mobility scooters. Many Medicaid recipients do not pay any costs for their medical coverage. Medicaid recipients cannot, however, just select a scooter that they want and hand over their Medicaid card for coverage. The provider, supplier, and physician must all accept Medicaid and be properly enrolled in the state program.
Are you a senior that receives Medicaid QMB? You may be able to get your scooter without cost if you do, since you do not pay deductibles, co-pays or other costs. Make sure that you give the physician, supplier and provider your Medicare card and your Medicaid QMB card.
You may qualify for this program if you are on Medicare and are income-eligible. The program, called Medicare Qualified Beneficiary, is administered through Medicaid. Many people that receive Medicare also receive Medicaid QMB benefits, which cover premiums, deductibles, and co-pays.
Contact Medicare to learn more about the program and you may be able to receive extra coverage, meaning that Medicaid pays for the costs of your scooter that is not covered by Medicare. The program does not cover benefits such as dental, vision, and hearing aid costs.
You May Like: Is There A Copay With Medicare Part D
Finding Help With Prescriptions Guide
“Finding Help with Prescriptions” Guide is a free publication. It provides helpful information for lowering your prescription costs including low-income assistance, patient assistance programs, mail order prescription services, veterans pharmacy benefits, and Community Health Centers.
To request a copy, call SHIP free of charge 452-4800 or email
SaveSave
Read Also: Will Medicare Pay For A Transport Wheelchair
Medicare Premium Payment Program
If you have Medicare, the Medicare Premium Payment Program may be able to pay for some of the costs There are three categories depending on a person’s income and resources. See below for more information. To apply, please contact your DHS Office or you can .
|
Medicare Premium Payment Program |
||
|---|---|---|
|
Specified Low-income Medicare Beneficiary Program |
Qualified Individual | |
| People age 65 and older and adults with disabilities may qualify if their income is less than 100% of the Federal Poverty Level and if their resources, such as savings, are less than $7,970 for a person or $11,960 for a married couple. If eligible, Medicaid will pay for Medicare Part A and B. | People 65 and older and adults with disabilities may qualify if their income is between 100% and 120% of the FPL and if their resources, such as savings, are less than $7,970 for a person and $11,960 for a married couple. If eligible, Medicaid will pay for Medicare Part B. | People 65 and older and adults with disabilities may qualify if their income is between 120% and 135% of the FPL and if their resources are less than $7,970 for an individual and $11,960 for a married couple. If eligible, Medicaid will pay the Medicare Part B premium. Funds for this program are limited and eligibility is on a first come, first serve basis. |
Executive Office of Health and Human Services
3 West Road
Helpful Tips For Members
- Use your formal, legal name. No nicknames or initials. Be consistent.
- If you change your name, make sure Social Security updates all three of their databases:
If you have more questions about this program please contact our Customer Contact Center.
Program Contact: , 303-866-5402
Don’t Miss: What Medicare Advantage Plans Cover Dental Implants
What Will Medicaid Cover
- Medicaid covers both routine and comprehensive eye exams which can include a variety of testing such as visual field test, pupil dilation, color blindness, glaucoma, and many others.
- Medicaid covers glaucoma screenings for people at higher risk for glaucoma.
- Medicaid covers eyeglasses that includes the frames, lenses, fittings, repairs and replacements of glasses.
- Medicaid covers bifocal and trifocals, or for two pair of single vision glasses if bifocals dont work. Over-sized lenses, no-line, progressive multi-focal and transitions are not a covered Medicaid benefit. However, if you want to buy these, you can pay for the additional costs.
- Medicaid only covers contact lenses if they are considered medically necessary and if there is no other alternative treatment. If they arent medically necessary, but you want them, you can pay for them separately.
- Medicaid Covers safety frames.
Read Also: Will Medicare Pay For Liposuction
What Are The Medicaid Benefits
Federal Requirements
The federal government requires each state to cover certain health-related benefits. These are known as mandatory benefits and include:
- physician, nurse midwife, and nurse practitioner services
- laboratory and x-ray services
- ipatient and outpatient hospital services
- early and periodic screening, diagnostic, and treatment services for children, teens, and young adults under age 21
- family planning services and supplies
- services provided in community health centers and rural health clinics
- nursing facility services for people age 21 and older
State Options
Your state can provide coverage for additional health-related services that are approved by the federal government. These so-called optional services may include:
- prescription drugs
- eye glasses and vision care
- mental health services
- rehabilitation services such as physical therapy
Also Check: Does Medicare Cover Assisted Living In Michigan
Does Medicare Cover Lung Cancer
Medicare covers many services for lung cancer, but costs can still add up. A 2018 study in Cancer Medicine looked at the amount people on Medicare spent for lung cancer at different stages.
During the screening and diagnostic phase, the average spent was $861. Chemotherapy and radiation costs averaged $4,242 to $8,287 per month over the first six months of care. The average cost of surgery, if pursued, was $30,096. This analysis, again, did not include the cost of more expensive immunotherapies.
Recommended Reading: Can You Use Medicare In Any State
