Does Medicare Advantage Cover Mental Health Care
Medicare Advantage does cover mental health care. While Medicare Advantage plans replace Original Medicare with a smaller, local network, they must cover what Medicare covers however, the costs for each service may vary. You will want to check with each plan to see how much Medicare Advantage will cost you for mental health services.
To learn more call a Senior65 agent at 800-930-7956.
Related Articles:
- New to Medicare: Everything you need to know. Medicare is the United States federal health insurance program for Americans 65 and older, as well as people with certain disabilities or End Stage Renal Disease .
- Pros and Cons of Medicare Advantage Finding the right Medicare insurance can be rather confusing for seniors – especially when parsing through the 150-page “Medicare and You” booklet that the government sends out as you approach age 65. We have made a list of the advantages and disadvantages of choosing a MA plan that should help
- Medicare Insurance Switching: Ultimate Guide With so many different plans, carriers, deductibles and what not, picking the wrong plan happens. A lot. Check out your options.
More Difficult To Bill Insurance Companies For Mental Health Providers:
The following links go to each companys credentialing website:
- EAPs
- Molina
Many Medicaid polices are subcontracted out to lower paying organizations. This can skew data downward in comparison to brands that to not facilitate a Medicaid plan in that State.
Likewise, EAP sessions have far more hoops, billing nuance, and prior-to-session manual labor involved in billing. Other EAP plans require their own unique form.
Simplify Your Practice Tip: If you are busy enough, consider dropping new EAPs.
Its worth noting that none of these are impossible to bill but each company has particularities about their claims filing process, operational speed, and subcontracting policy, which can lead to a higher likelihood of problems and a longer claims and revenue cycle.
Mental Health Professional Services
Medicare Part B helps cover mental health services and visits with health care providers who accept assignment, or the approved amount. The term assignment means that the provider of the mental health services agrees to charge the amount that Medicare has approved for services. You should ask the provider if they accept assignment before agreeing to services. It is in the best interest of the mental health service provider to notify you if they do not accept assignment, however, you should confirm this before signing any agreements with the provider.
You may want to visit the Centers for Medicare and Medicaid Services Physician Compare, to find a doctor who accepts Medicare services. A list of professionals or group practices in the specialty and geographic area you specify, along with detailed profiles, maps, and driving directions are available.
Health professional types covered include:
- medical doctors
Read Also: Is Coolief Covered By Medicare
How Do You Know If They Take Medicare
Since March of 2020, Medicare covers online therapy for all Medicare members. The tricky part can be finding a telehealth provider that accepts Medicare. Online telehealth platforms usually state on their website whether they accept Medicare, or list all the various insurance providers they accept. If not, you should speak to one of their agents.
For a private therapist or practice, you should be able to contact the office directly in order to get an answer on whether they provide remote consultations and accept Medicare. Once you have found the ideal private care provider, you can ensure they accept Medicare through the Health Resources and Services Administration . HRSA has a website that allows you to type in the address of your preferred telehealth specialist and it will verify whether or not they accept Medicare.
If you want to utilize online medical service platforms that specialize in telehealth, there are a variety of them that accept Medicare. One of the most popular providers is Doctor On Demand. Even better, Doctor On Demand is currently waiving co-pays for Medicare Part B enrollees during the ongoing public health emergency.
Another telehealth provider, Amwell, accepts Medicare. However, they only take Medicare Advantage, so if you are only enrolled in Original Medicare, it may be best to go with Doctor On Demand. These are just a couple of the many telehealth providers that accept Medicare.
Coverage Amounts And Co
While some services are covered fully, such as depression screenings, others may require the beneficiary to pay 20% of the Medicare-approved amount. That includes visits to a healthcare provider to diagnose mental health conditions. Services that are provided by hospital outpatient services may be subject to additional co-pays.
Co-pays can be reduced by combining Medicare with other insurance plans.
Read Also: Who To Talk To About Medicare
About The Current State Of Medicaid & Mental Health Services
If you have Medicaid, know that you have access to an array of mental health services you need for yourself and your children. In fact, Medicaid is the largest national single-payer for mental health services in the United States, so rest assured. After all, many others who use Medicaid have found mental health services that are covered, which means you can too its all about knowing where to look.
Theres even more good news: Thanks to the Affordable Care Act, Medicaid is currently expanding its role in the reimbursement of substance use disorder services and behavioral health disorder services to provide more help to more Americans. Congress enacted these laws to improve mental health and substance use disorder services for those with Medicaid, making it easier for you to find a mental healthcare provider without having to pay out of pocket.
The most recent law, the Mental Health Parity and Addiction Equity Act extended coverage for mental health services to millions of Medicaid beneficiaries who participate in Managed Care Organizations, State alternative benefit plans, and Medicaid for children .
Medicaid has greatly expanded its mental health service coverage, which is good news for those seeking therapy, rehabilitation, or other assistance. This coverage has been updated to reflect the current key mental health priority access across the nation for the next several years including:
What Original Medicare Doesnt Cover
Your health care provider may recommend you receive services more frequently than Medicare covers, or services that Medicare doesnt cover, and you may end up paying some or all of these costs. Ask your provider why they are recommending such services and whether Medicare will cover them.
You will have to pay for private duty nursing or a private room, unless its medically necessary. Other limits may apply.
Also Check: Can I Cancel My Medicare Part D Plan Anytime
Does Medicare Cover Mental Health Coverage Advice For Medicare Plans
Discover what common mental health treatments various Medicare health insurance plans cover, including therapy and prescription medication for depression and anxiety.
by Zia Sherrell | Published March 31, 2021 | Reviewed by John Krahnert
Mental health is an increasing concern for older adults, according to the American Psychological Association. It notes that in 1970, 4 million older Americans had mental and behavioral problems, but experts predict that number will nearly quadruple to 15 million by 2030.1
Just like physical ailments, mental health problems like depression and anxiety are treatable under your Medicare coverage. Thankfully, Medicare covers many common mental health treatment options. In this article, we outline how each part of Medicare covers mental health, including what you can expect it to cost and how you may be able to use a Medicare Supplement plan to help pay for your Medicare costs.
Compare Medicare Advantage Plans That Cover Counseling
For California residents, CA-Do Not Sell My Personal Info, .
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
Recommended Reading: When Can I Get My Medicare Card
Medicare Part D Prescription Drug Coverage And Mental Health Care
Medicare Part D prescription drug plans are not required to cover all drugs, but with limited exceptions, they are required to cover all antidepressant, anticonvulsant and antipsychotic medicines.
Part D plans are sold by private insurers and other companies that Medicare approves. Almost all plans have a formulary a list of drugs the plan covers. This list can change each year, but the company has to notify you at least 30 days before the change takes effect.
Its important to review your plans formulary changes when you receive this information.
Medigap Medsup And Mental Health Care
For starters, both Medigap and MedSup are terms for a product normally called Medicare supplement insurance.
As implied, this policy supplements the costs related to Original Medicare. To put it another way, it helps people pay for some of the expenses Medicare doesn’t cover.
Learn more about this type of plan in our “Medicare Supplement Insurance Policy FAQ.”
That’s true whether you’re talking about general health care or mental health care. For example, most Medigap plans cover the costs Medicare Parts A and B won’t pay for if you’re hospitalized for mental illness.
A few examples:
- All Medigap policies cover your Part A hospitalization copays and coinsurance
- They also cover all or part of your psychiatrists copays and coinsurance
- Most of these plans cover your Part A hospitalization deductible, too
MedSup and Medigap plans help if you’re ever get outpatient treatment for mental illness as well. Specifically, they usually cover some or all of your Part B out-of-pocket costs.
Read Also: Does Medicare Part D Cover Shingrix Vaccine
What Medicare Covers For Outpatient Mental Health Services
Medicare Part B, which pays doctor bills and related health care expenses, covers many mental health services rendered to patients not admitted to a hospital. Covered costs include:
-
A Welcome to Medicare visit that includes a review of your risk factors for depression.
-
One depression screening per year, performed in the office of a primary care doctor or in a primary care clinic that provides follow-up treatment and referrals.
-
Psychiatric evaluation to diagnose mental illness and prepare a care plan.
-
Diagnostic testing.
-
Individual and group psychotherapy or counseling provided by physicians or certain other professionals licensed to do so in your state. Covered providers may include psychiatrists or other doctors, clinical psychologists or social workers, nurse practitioners and physician assistants.
-
Family counseling that aids in your mental health treatment.
-
Medication management and some prescription drugs that are not self-administered.
-
Partial hospitalization, which typically includes many hours of treatment per week without admission to a hospital.
-
Testing to find out if youre getting the services you need and if your current treatment is helping you.
-
An annual wellness visit with a doctor or other provider to discuss any mental health changes.
How Much Does Medicare Pay For Mental Health Care Services
An annual depression screening is free if the doctor accepts Medicare assignment. Otherwise, Medicare Part B pays 80 percent of the Medicare-approved amount for most covered mental health care services. You are responsible for the remaining 20 percent, and the Part B deductible applies.
Medicare Advantage plans also help pay for mental health care services and may cover additional mental health services or items. Check with your plan provider to get coverage and cost details.
Recommended Reading: Does Medicare Pay For Drug Rehab
What Doesnt Medicare Cover For Counseling
Medicare only covers counseling services provided by a certified mental health care provider. Medicare will not cover counseling from a religious professional, such as a priest or pastor. Medicare also does not provide coverage for these mental health care services:cms.gov, Medicare Mental Health, Accessed November 15, 2021
- Environmental intervention or modifications
- Results or data interpretation or explanation
- Hemodialysis specifically for treating schizophrenia
- Transportation or outpatient meals
- Phone services, or apps
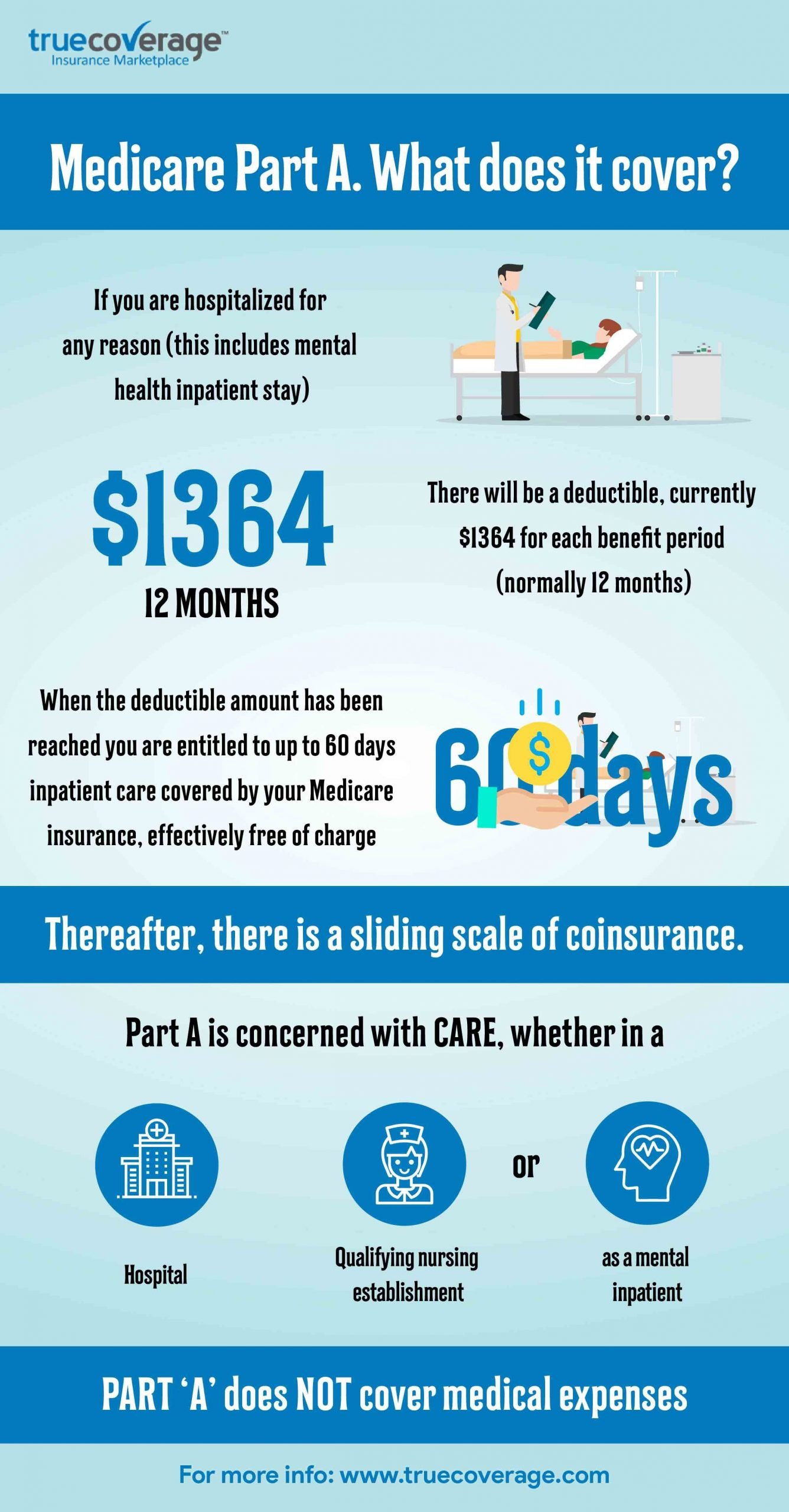
Does Medicare Cover Inpatient Psychiatric Care
Inpatient psychiatric mental health care falls under Part A benefits. Further, Part A will cover a portion of the cost for the room, meals, nursing, and other services. You can obtain care in a hospital or psychiatric hospital.
But, the lifetime limit of inpatient psychiatric hospital care is 190 days. Also, you may incur costs for Part B while an inpatient in the hospital, this could be from doctor services.
Also Check: What Is Medicare Part A B C And D
Q: What If My Doctor Or Specialist Recommends A Mental Health Service Or Treatment That Medicare Doesn’t Cover
A: Unfortunately, you’ll probably have to pay for some or all of that service or treatment.
The same is true, by the way, if you have a test, treatment, or service done more often than Medicare allows.
In cases like these, talk to your doctor or other specialist about why he or she thinks you should do them so frequently. And then use that information to decide if you should agree to it or not.
Outpatient Drug Coverage Under Medicare
Any medications that you fill at a local pharmacy will fall under Part D. You join a Part D drug plan by applying directly with the insurance company or through one of its agents. There is often a dozen or more plans offered in each state.
Each plan has a drug formulary, so its important that you check the formulary before you enroll to make sure that your needed medications are covered by the plan. Fortunately, there are some basic minimum guidelines for all drug plans, and one of those guidelines is that all drug plans must carry antidepressants and antipsychotics. In fact, the plans must cover at least two medications in every therapeutic class.
When you go to the pharmacy, youll present your Part D insurance card. The pharmacist will bill the drug plan and you are only responsible for the copay that is designated in the plans summary of benefits. In most cases, the insurance company pays the larger share of the cByost of the medication.
Part D drug plans also all have catastrophic coverage limits. If you have expensive medications which require a lot of out of pocket costs, you are protected by this cap. Once you reach it, you only owe 5% of the cost of your medications for the rest of the year.
You May Like: How To Get Dental With Medicare
Medicare Outpatient Mental Health Services
Medicare Part B covers outpatient mental health services, such as care youd get in a health clinic or doctors office. Youll generally pay 20% of the Medicare-approved cost for outpatient care delivered by providers that accept Medicare assignment.
Medicare covers the following types of psychotherapy :
- Psychiatric assessment
- Family counseling, when the primary goal is to treat your condition
- Alcohol misuse counseling, up to four sessions
You may need to meet other criteria to be eligible for therapy coverage, and the doctor, psychologist, or other health-care professional must accept Medicare assignment. Medicare doesnt cover certain types of therapy, such as pastoral counseling or marriage counseling.
If you need more structured or frequent treatment, Medicare Part B also covers partial hospitalization programs, which are outpatient mental health programs where treatment is provided throughout the day and doesnt require an overnight, inpatient stay. The programs are usually run through a community mental health center or a hospitals outpatient department. Services may include therapy with a mental health professional, diagnostic services, and occupational therapy . These programs dont cover meals or transportation to the facility.
Medicare Part D And Prescription Drug Coverage
Medicare Part D are plans run by private companies approved by Medicare. Since each plan can vary by coverage and cost, its important to know the details of your plan and how it applies to medication for mental health care.
Most plans have a list of drugs the plan covers. Although these plans are not required to cover all medications, most are required to cover medications which may be used for mental health care, such as:
- anticonvulsants
- antipsychotics
If your doctor prescribes a drug that yourplan doesnt cover, you canask for coverage determination and/or an exception.
Mental health care services typically not included under Medicare parts A and B are:
- private room
Don’t Miss: When Does Medicare Coverage Start
Does Medicare Pay For Psychotherapy
Psychotherapy, sometimes called talk therapy, involves talking to a licensed and trained mental health care professional typically a psychologist to help the patient understand and identify problems contributing to his or her mental illness.
Coverage: Medicare Part B helps pay for individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Q: What If I Need A Drug My Medicare Part D Plan Doesnt Cover

A: According to medicare.gov, if you have a Medicare drug plan, you can ask for a coverage exception.
Basically, this means you can ask your plan to provide or pay for a drug you think should be covered.
You also can appeal your plan’s decision about whether or not to provide or pay for a drug.
Before you take either of these steps, though, talk with your doctor or the health care provider who wrote the prescription. He or she should be able to tell you if your plan has special coverage rules. They also can tell you if any generic or over-the-counter drugs could work as well as the ones they prescribed.
If that doesn’t help, go to cms.gov for more on how to request a coverage determination or exception.
Read Also: How To Find Out Your Medicare Number
