Crohns Sufferer Pays $2k A Month For Stelara And Part D Penalty
| Toni King |
When I enrolled in July for a new Medicare Part D plan, Iwas denied because did I not apply on time. I take Stelara which is over $2,000 a month that I now must pay on myown.
I now am 70 years old and have been told that my Part Dpenalty for not enrolling in Medicare Part D will be $.3274 X 60 months sincemy Part A began 5 years ago. I cannot believe that I must pay an extra $19.64per month as a Part D penalty.
Please explain this ridiculous Medicare Part D penalty. I have not purchased my Stelara in the lastfew months. Thank You, Sydney.
_________________________
Sydney,
You are aware you waited too long to apply for a MedicarePart D plan. Once you are past 65 and/orleaving creditable coverage, Medicare gives you 63not 70 or 90 days to applyfor a Medicare Part D or Medicare Advantage plan with prescription drugcoverage. Not needing to order yourprescriptions does not refrain from receiving Part D penalties.
Your late enrollment period does not begin from theday you lose or leave your company health plan, BUT from the month youturned 65 or began your Medicare and is based on when Medicare Part A beginsnot Part B.
This LEP penalty can be because:
You must wait until the next Medicare Annual Enrollmentperiod from October 15-December 7 to enroll in a Medicare Part D prescriptiondrug plan with your effective date to be January 1, 2021.
Basic Drug Information About Stelara
STELARA contains the active ingredient ustekinumab. It is administered by IV or by subcutaneous injection into fatty parts of the skin, such as the upper arms, buttock, thighs or abdomen. The drug treats Crohn’s disease, psoriasis and psoriatic arthritis by binding to and reducing inflammatory substances in the body. Major side effects include weakness, fatigue, headache, vomiting, irritation at the injection site and nose and throat irritation.For treatment of psoriasis or psoriatic arthritis, you receive an initial subcutaneous injection followed by a second dose 4 weeks later. After that, you receive a dose every 3 months. To treat Crohn’s disease or ulcerative colitis, the first dose is administered via injection into a vein. Then, doses are given every 8 weeks as directed by a doctor.
Does Medicare Cover The Cost Of Stelara
What youll play for Stelara depends on your specific Medicare plan. It may also depend on whether you receive your dose at the doctors office or give yourself injections at home. If you have questions about your cost for Stelara with Medicare, talk with your doctor or contact your Medicare plan provider.
Also Check: Does Medicare Cover When Out Of Country
Medicare Costs For Part B Drugs
If you have Original Medicare youll pay 20% for Part B drugs. This may not sound like a lot, but when you consider that a drug like Soliris costs $440,000 a year, your out of pocket costs would be $88,000 just for the drug. Yes, thats an extreme example, and its meant for the treatment of two types of rare blood diseases, but you get the picture. However, if you have any Medigap policy, 8 out of 10 plans will cover this cost completely.
For Medicare Advantage Plans That Do Not Offer Prescription Drug Coverage
Stelara,for the indications listed below:
-
Crohns Disease
Is not covered for new starts, unless the member meets ANY of the following:
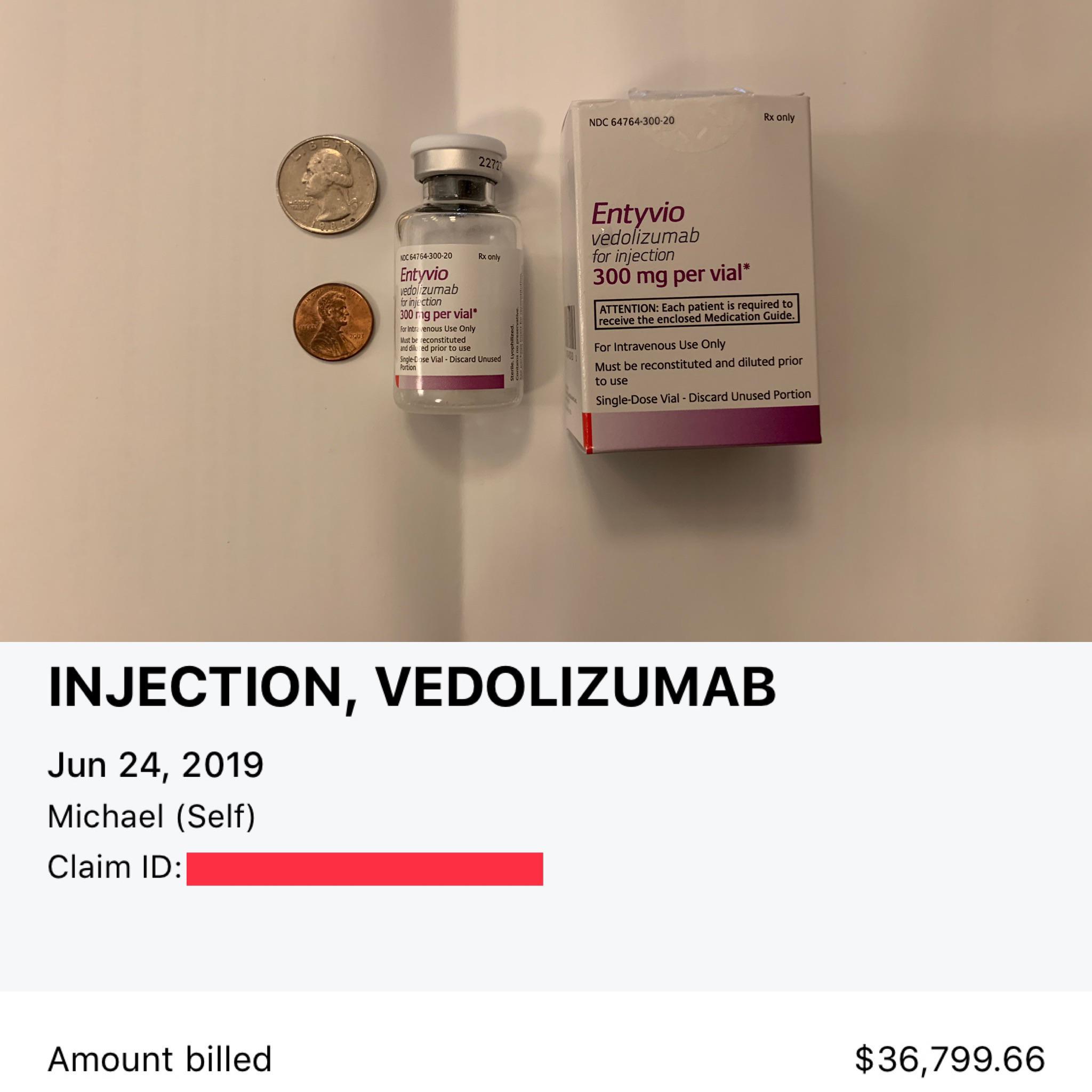
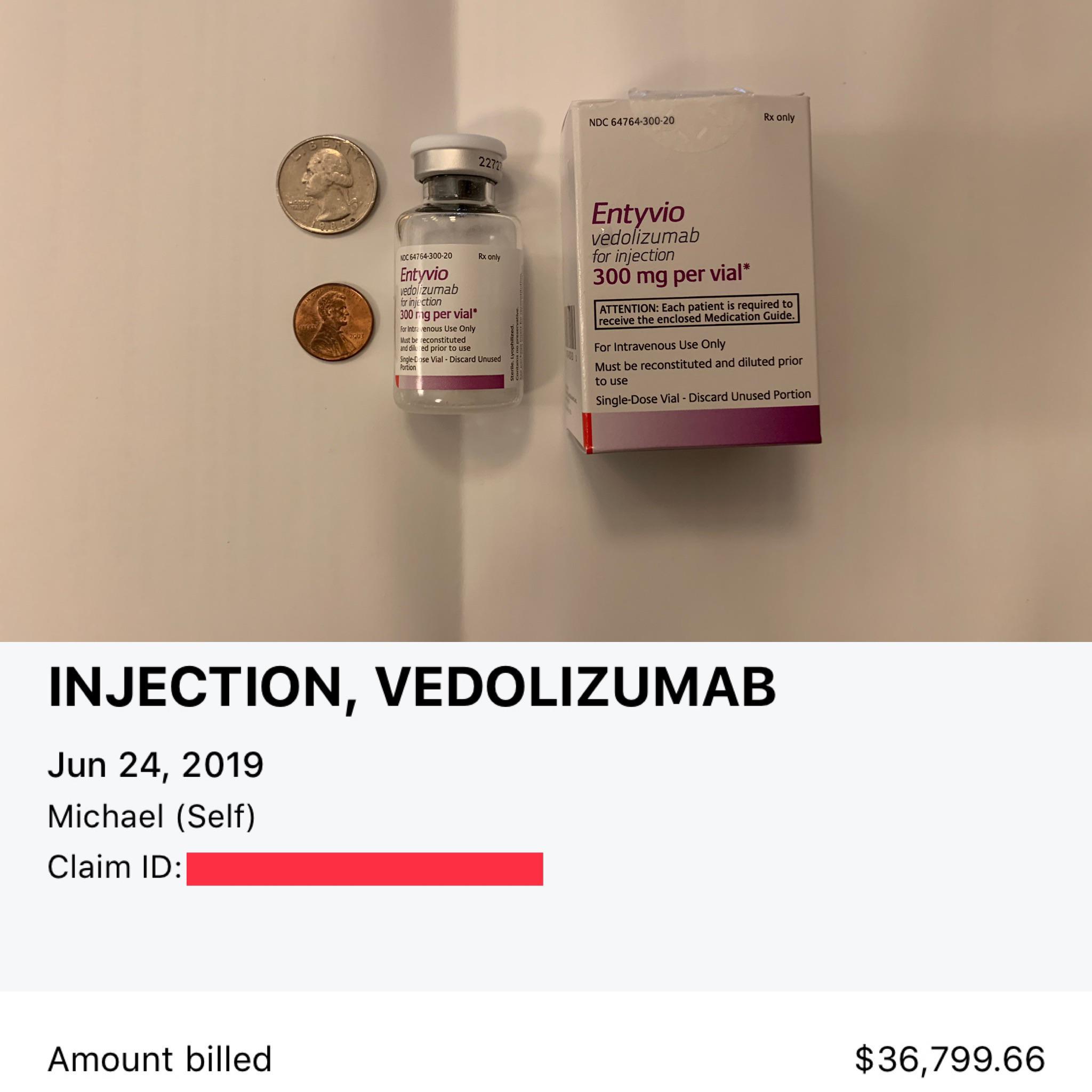
- Inadequate response to a trial of Avsola, Entyvio, or Remicade
- Intolerable adverse event to Avsola, Entyvio, or Remicade
- Avsola, Entyvio, or Remicade is contraindicated for the member
-
Plaque Psoriasis
Is not covered for new starts, unless the member meets ANY of the following:
- Inadequate response to a trial of Avsola or Remicade
- Intolerable adverse event to Avsola or Remicade
- Avsola or Remicade is contraindicated for the member.
-
Adult Psoriatic Arthritis
Is not covered for new starts, unless the member meets ANY of the following:
- Inadequate response to a trial of Avsola, Remicade, or Simponi Aria
- Intolerable adverse event to Avsola, Remicade, or Simponi Aria
- Avsola, Remicade, or Simponi Aria is contraindicated for the member.
Recommended Reading: When Can I Get My Medicare Card
How Do I Apply For The Stelara Patient Assistance Program
Our application process is simple and straightforward. Begin by completing our enrollment application, and tell us about any medications youre taking, including Stelara. Well ask for details about your healthcare provider, insurance, and your household income, as this information is required by the pharmaceutical manufacturers who ship your medication.
If we think you may be eligible for Stelara assistance, well handle the application process on your behalf and help to enroll you in the Stelara patient assistance program. Our service continues once youre enrolled in the program, as well also request your Stelara medication refills on your behalf for up to a full year.
Provider: Johnson & Johnson Patient Assistance Foundation Inc Patient Assistance Program
Elligibility requirements:
Applicable drugs:
- StelaraInjection IV Subcutaneous
More information please phone:800-652-6227Visit Website
Also Check: What Weight Loss Programs Are Covered By Medicare
Stelara Withme Savings Program
Eligible patients using commercial or private insurance can save on out-of-pocket medication costs for STELARA®. Depending on the health insurance plan, savings may apply toward co-pay, co-insurance, or deductible. Eligible patients pay $5 for each dose. Maximum program benefit per calendar year shall apply. Not valid for patients using Medicare, Medicaid, or other government-funded programs to pay for their medications. Terms expire at the end of each calendar year and may change. There is no income requirement. Program does not cover the cost to give you your treatment. The STELARA withMe Savings Program provides a rebate when used with medical/primary insurance and provides instant savings when used with pharmacy/prescription insurance.
We provide cost support directly to patients through the STELARA withMe Savings Program. This benefit is intended to help eligible patients afford their out-of-pocket obligations as set by their health plans. The cost support is meant solely for patientsnot health plans and/or their partners. If you are having any difficulty accessing cost support through the STELARA withMe Savings Program, please contact us at 844-4withMe .
Already enrolled? Create your online account at MyJanssenCarePath.com to manage your program benefits and submit rebate requests.
How to obtain a rebate if you have not created an online account:
Financial And Insurance Assistance
If you need financial support to pay for Stelara, or if you need help understanding your insurance coverage, help is available. For example:
- A program called Janssen CarePath is available for Stelara. For more information and to find out if youre eligible for support, call 877-CAREPATH or visit the program website.
- Some websites provide details about drug assistance programs, ways to make the most of your insurance coverage, and links to savings cards and other services. Two such websites are:
You May Like: Do You Have To Apply For Medicare
What Is Stelaras Price
The price you pay for Stelara can vary. Your cost may depend on your treatment plan and your insurance coverage . It may also depend on how much you have to pay for an office visit with your doctor to receive Stelara.
If you use the form of Stelara that comes in a vial, you may also need to buy needles and syringes.
To find out how much youll pay for Stelara, talk with your doctor or insurance provider.
Note: If you have insurance, you may need to get prior authorization before your insurance provider will cover Stelara. This means your insurer and your doctor will discuss Stelara in regard to your treatment. Then the insurance company will determine whether the drug is covered. If Stelara requires prior authorization and you dont receive it before you start treatment, you could pay the full cost of the drug.
Be sure to ask your insurance company whether Stelara requires prior authorization.
Below are answers to some frequently asked questions about Stelara and cost.
How To Get A Referral For Stelara Sq Injections
Every Stelara referral must be accompanied by a physicians order for treatment.
- Patient information should include:
Supporting clinical documentation from the physician should include:
- Results of a recent tuberculosis skin/lab testing
- Patients current weight and height
- For Crohns patients,include date of induction dose given
- Clinicals to support one or more of the following:
- Patient has moderately to severely active Crohns disease and evidence to support one or more of the following:
- Failed or was intolerant to treatment with immunomodulators or corticosteroids but never failed treatment with a tumor necrosis factor blocker OR
- Failed or was intolerant to treatment with one or more TNF blockers
- Patient has active psoriatic arthritis
- Patient has moderate to severe plaque psoriasis who is a candidate for phototherapy or systemic therapy
Patients chose IVX Health to receive their ongoing Stelara SQ treatments because:
- ALL private suites
Recommended Reading: When Do You Get Medicare When On Disability
Does Medicare Have Any Restrictions On Coverage
Some Medicare plans do place quantity limits on STELARA or require prior authorization. A quantity limit only allows you to fill a prescription for a limited amount of the drug at a time. Prior authorization requires your doctor to contact your plan and show that the drug is medically necessary before you can receive it.
Paying For Stelara With Medicare
Question posted by mullenkathy1 on 21 Aug 2022
Can someone tell me how Medicare pays for this medication? We have Medigap, Medicare, A& B, and a drug plan through AARP. The co pay we have been quoted is 4K every 8 weeks. Im confused I have a Medigap policy no copays. Anyone on Medicare with similar coverage pay less? I appreciate any responses.
No answers have yet been posted. Add your answer to this question.
Don’t Miss: How Do You Get Credentialed With Medicare
If You Have Commercial Or Private Health Insurance But Your Stelara Treatments Are Not Covered:
Make sure your doctors office staff has checked both your pharmacy and medical benefits. If youve confirmed that you are not covered by either your pharmacy or medical benefits, call Janssen CarePath at for information on other financial assistance programs that may be able to help you.
The following programs are not affiliated with Janssen.
Be sure to contact the programs directly to get details on eligibility and application requirements, and to see if they have funding available to help you.
Are There Any Additional Medicare Costs
A person will generally have out-of-pocket costs to pay for a Medicare Part D plan or a Medicare Advantage policy. These costs can include premiums, deductibles, copays, and coinsurance.
The Medicare Part D deductible has a maximum of $445 for 2021. After a person pays the deductible, the policy begins paying benefits.
After both the plan and the person with the plan have paid a total of $4,130 in 2021, the person will enter the coverage gap. During this time, they will pay no more than 25% of the cost of brand-name drugs such as Humira.
After the person and the plan have spent $6,550 in 2021, the person will enter the catastrophic coverage phase. During this time, the person will pay only a small copayment or coinsurance for all their drugs for the rest of the year.
Some Medicare Advantage plans may have a $0 deductible for drug coverage.
If a person gets coverage through Medicare Part B, they will generally pay the monthly premium, which $148.50 per month in 2021. They may also have an annual deductible to pay, which is $203 in 2021.
A person may be able to get some help with drug costs through programs such as Medicaid and Extra Help. Some drug companies also offer assistance programs.
The following sections will look at these options in more detail.
Recommended Reading: Are Lidocaine Patches Covered By Medicare
Is Nicerx A Stelara Coupons Provider
NiceRx is a service provider that helps eligible individuals access the Stelara patient assistance program. We are not a Stelara coupon, a Stelara discount card, or a Stelara copay card. We dont provide printable Stelara manufacturer coupons, Stelara discounts, rebates, Stelara savings cards, trial offers, or free Stelara samples.
If youre looking for coupons for Stelara or cheap Stelara, you will likely save more with NiceRx. Remember, as part of a patient assistance program, you will pay nothing more than the monthly cost of $49.
How Can I Determine Stelaras Cost With Insurance Vs Without Insurance What About With Medicare
Your out-of-pocket cost for a brand-name drug is typically less if you have health insurance. If you have insurance, call your insurance provider to see if they cover Stelara. They can tell you exactly how much your prescription of Stelara will cost.
The drug manufacturer has cost-savings programs for both insured and noninsured people. This can help lower your out-of-pocket cost for Stelara.
If Stelara is not covered by insurance, your pharmacist can provide you with the cost of the drug. The price can vary between pharmacies.
If you are on Medicare, your Stelara prescription may need to go through an approval review to receive coverage. Talk with your Medicare representative about getting a coverage review. They can tell you exactly how much your cost will be for Stelara.
Don’t Miss: What Benefits Do You Get With Medicare
For Medicare Advantage Plans That Do Not Offer Prescription Drug Coverage And Medicare Advantage Plans That Offer Prescription Drug Coverage
Stelara, for the indications listed below:
-
Ulcerative Colitis
Is not covered for new starts, unless the member meets ANY of the following:
- Inadequate response to a trial of Avsola, Entyvio, or Remicade
- Intolerable adverse event to Avsola, Entyvio, or Remicade
- Avsola, Entyvio, or Remicade is contraindicated for the member.
Average Costs For Stelara With Medicare Drug Coverage1
Your copay and deductible costs for any prescription drug can vary depending on what coverage stage youre in.
| Deductible stage | Typical copay stage |
|---|---|
| Your deductible is the amount of money you must spend on covered drugs before your Medicare drug coverage starts paying its share of costs.In the deductible stage, youre responsible for the full cost of your prescription drugs.Some Medicare prescription drug plans have a $0 deductible. Medicare drug plans cannot have a deductible more than $480 in 2022. | After you meet your Part D deductible, you enter the initial coverage period.During this phase , you pay a copayment or coinsurance for your covered medications. |
| $6,326 $25,305 | $6,326 $25,305 |
Read Also: Where Do I Get A Medicare Card
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
| TTY 711, 24/7
The major side effects of Stelara include feeling tired or weak, headache, vomiting, nose and throat irritation, signs of a common cold and irritation where the shot is given.
Appendix A: Examples Of Conventional Therapy Options For Cd
Mild to moderate disease – induction of remission:
Mild to moderate disease – maintenance of remission:
Moderate to severe disease – induction of remission:
Moderate to severe disease – maintenance of remission:
Perianal and fistulizing disease – induction of remission:
Metronidazole ± ciprofloxacin, tacrolimus
Perianal and fistulizing disease – maintenance of remission:
You May Like: Can Doctors Limit The Number Of Medicare Patients
What Parts Of Medicare Cover Humira
Humira is an injectable medication. People can self-administer it at home, though they may require training to do so. However, some people may need to get the injections at their doctors office or as an outpatient.
If a person self-administers Humira, Medicare Part D will cover the prescription drug cost. Many Part C, or Medicare Advantage, plans may also cover the drug, though a person will need to check with their plan provider.
If a person receives their Humira injections as an outpatient or in their doctors office, Medicare Part B may cover the cost.
. The cost of a 20-milligram injection rose from $1,895 in 2010 to $5,300 in 2019.
Johnson & Johnson Patient Assistance Foundation Inc
The Johnson & Johnson Patient Assistance Foundation, Inc. is an independent, nonprofit organization. JJPAF gives eligible patients free prescription medicines donated by Johnson & Johnson companies. You may be eligible if you don’t have insurance, if your medicine is not covered by insurance, or if you have Medicare coverage and can’t pay for your medicine.
Want to see if you qualify? Get an application at JJPAF.org.
Questions? Call 800-652-6227 .
The following programs are not affiliated with Janssen.
Be sure to contact the programs directly to get details on eligibility and application requirements, and to see if they have funding available to help you.
Also Check: What Are The Five Steps In The Medicare Appeals Process
Criteria For Initial Approval
Aetna considers ustekinumab medically necessary for the following indications, where the member has a documented negative TB test , an interferon-release assay , or a chest x-ray) within 6 months of initiating therapy for persons who are naive to biologic DMARDs or targeted synthetic DMARDs associated with an increased risk of TB:
Moderately to severely active Crohn’s disease
Moderate to severe plaque psoriasis or active psoriatic arthritis
When member meets criteria in or
Moderately to severely active ulcerative colitis
Aetna considers all other indications as experimental and investigational .
