Foreign Travel Outside The United States Including Canada And Mexico
Usually, Medicare does not pay for services when a person is out of the U.S., which includes anywhere other than the 50 states, the District of Columbia, the U.S. Virgin Islands, American Samoa, Guam, the Northern Mariana Islands, and Puerto Rico.
There are some exceptions, such as:
- If a person is going through Canada by the most direct route and is between Alaska and another state when a medical emergency occurs, then Medicare may cover services. However, the hospital in Canada must be closer than the U.S. hospital for a person to get coverage.
- A person may also file a claim if they are in the U.S. and require care for a medical emergency, but the foreign hospital is closer than the hospital in the U.S. Foreign hospitals do not have to file a Medicare claim, so it may be up to the person to do so.
Mail Completed Form And Supporting Documents To Medicare
Submit your completed Patients Request for Medical Payment form, itemized medical bill or bills, and any supporting documents to your states Medicare contractor. All claims must be submitted by mail you cant file a Medicare claim online. You can find the mailing address for your states contractor in a number of ways:
- View the second page of the Medicare instructions for your Medicare claim type
- View your Medicare Summary Notice. If you dont have a hard copy on hand, you can view an electronic version when you log in to MyMedicare.gov
- Visit the CMS.gov website
The Medicare website can also answer many questions about filing a Medicare claim before you submit your paperwork. If you still have questions, contact Medicare and speak to a representative.
As a beneficiary, you have one calendar year after receiving medical services to file your Medicare claim. If you file your claim after 12 months has elapsed, it will probably be rejected.
Following the right steps will make sure your claim is approved in a timely fashion. We invite you to share this post with your social media contacts so they know how to correctly file a Medicare claim.
Claim Status Request And Response
Providers have a number of options to obtain claim status information from Medicare Administrative Contractors :
Providers can enter data via the Interactive Voice Response telephone systems operated by the MACs.
Providers can submit claim status inquiries via the Medicare Administrative Contractors provider Internet-based portals.
Some providers can enter claim status queries via direct data entry screens.
Providers can send a Health Care Claim Status Request electronically and receive a Health Care Claim Status Response back from Medicare.
The electronic 276/277 process is recommended since many providers are able to automatically generate and submit 276 queries as needed, eliminating the need for manual entry of individual queries or calls to a contractor to obtain this information. Submission of 276 queries and issuance of 276 responses should be less expensive for both providers and for Medicare. In addition, the 277 response is designed to enable automatic posting of the status information to patient accounts, again eliminating the need for manual data entry by provider staff members. If unsure whether your software is able to automatically generate 276 queries or to automatically post 277 responses, you should contact your software vendor or billing service.
You May Like: Do Medicare Advantage Plans Cover Dentures
If Your Provider Doesnt File In A Timely Manner
If the 12-month deadline to file a Medicare claim is approaching and your doctor hasnt filed a claim for your care, you may have to file a Medicare claim yourself.
First you should contact the doctor or supplier and ask them to file a claim. If still they dont, and the deadline is approaching, you should go ahead and file the claim yourself.
How To File A Medicare Claim

Home / FAQs / General Medicare / How to File a Medicare Claim
Most of the time, you wont need to worry about filing your own Medicare claims. Since most providers accept assignment, they file the claim for you. But, knowing how to do it will come in handy in case you need to file your own claim. If you need to file a claim, its possible the provider you saw doesnt accept the assignment. Your claim goes according to Medicare reimbursement rates, even if the bill was more than Medicares amount. Claims must be sent in no later than 12 months after the service.
You May Like: How To Change Primary Doctor On Medicare
Who Files Medicare Claims
Your healthcare provider will usually file claims for you. You should never have to submit claims for Part A services such as hospital, skilled nursing facility or hospice care. When it comes to outpatient care, some providers will not file claims. This can happen if you have Original Medicare and see a non-participating provider, or if you have Medicare Advantage and visit an out-of-network doctor.
Beneficiaries can submit their own claims for certain services when a provider wont file a claim. However, you cannot file a claim with Original Medicare for diabetic test strips, Part B drugs, or equipment paid for under the DMEPOS Competitive Bidding Program. Your pharmacy or medical supplier must bill Medicare directly for these items.
Point And Click License For Use Of Current Dental Terminology
End User License Agreement
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED “I ACCEPT”, YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED “I DO NOT ACCEPT” AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, “YOU” AND “YOUR” REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
Recommended Reading: Is Obamacare Medicare Or Medicaid
Submitting Medicare Part D Claims
For Processing Medicare Part D Vaccine & Administration Claims
Univera Healthcare now offers you an online option for processing Medicare Part D vaccine and administration claims with TransactRx Part D Vaccine Manager. TransactRx, a product of Dispensing Solutions, Inc. , is a Web portal that provides physicians with real-time claims processing for all in-office administered Medicare Part D vaccines. For example, with TransactRx, a physician’s office can bill Univera Healthcare online when administering the shingles vaccine, Zostavax, to Medicare Part D members.
Enroll in Transact Rx at no cost for a simple and convenient way to submit Medicare Part D vaccine and administration claims.This new online option gives you a faster, more efficient way to submit these claims by having the ability to:
- Verify members’ eligibility and benefits in real-time
- Advise patients of their appropriate out-of-pocket expense
- Submit vaccine claims electronically
Is My Doctor Required To File My Medicare Claims Or Do I File Them With Medicare Directly
En español | Medicare providers are required by law to submit directly to Medicare any claims for covered services that they have provided to Medicare patients.
However, there are situations in which you may be asked to pay a physician who does not accept assignment and then submit your own claim for reimbursement to Medicare, using form CMS-1490S. You can download the English version of this form from . For the Spanish version, go to .
Don’t Miss: How Much Do I Have To Pay For Medicare
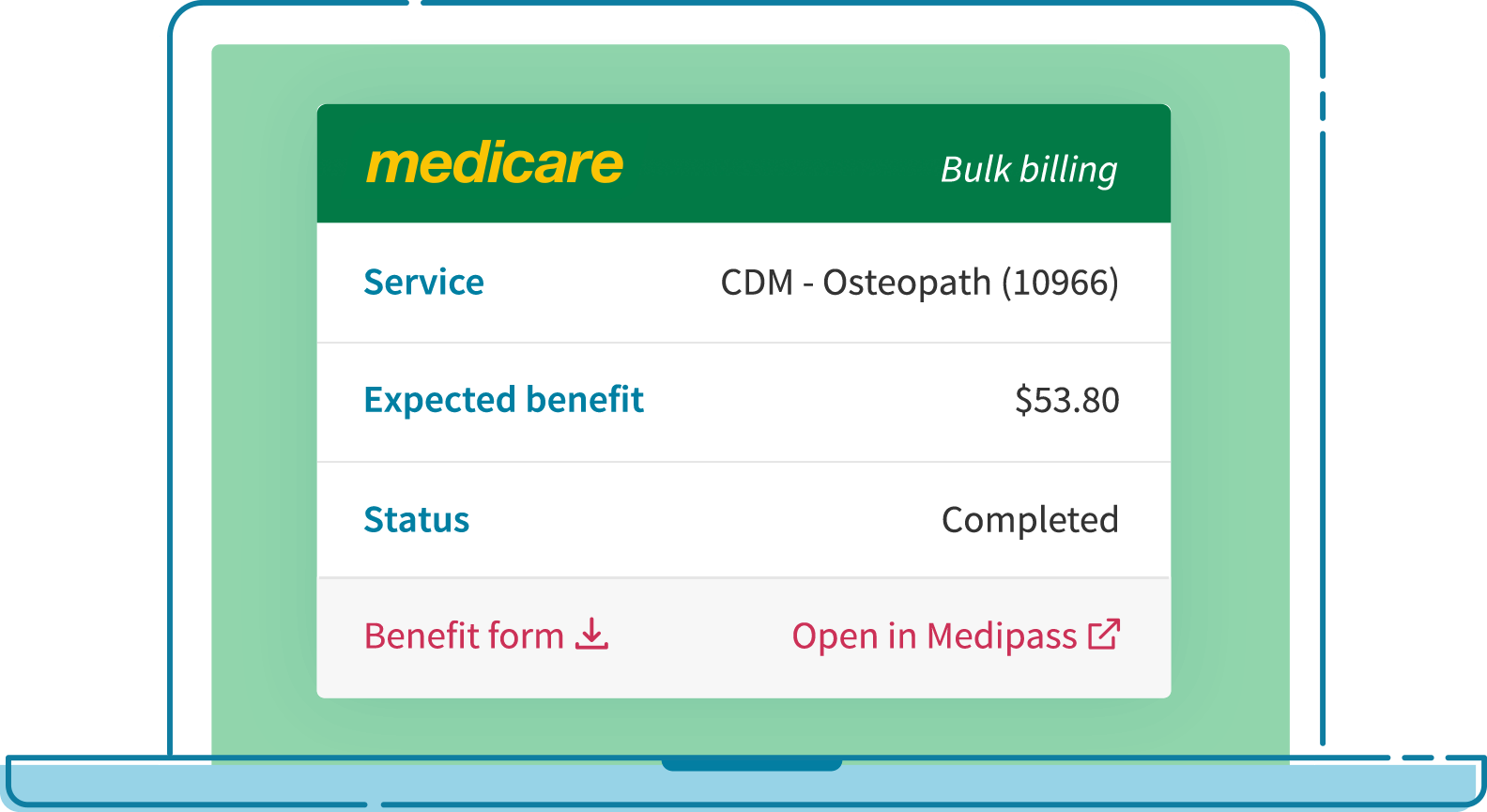
Add Provider And Item Details
Tell us the doctors Provider number.
You can find this on the account or receipt. Its a combination of letters and numbers up to 8 characters long.
Add the Provider number, then select Next.
You need to tell us about the treatment you got. You can find the item number on the account or receipt. Its a set of numbers and can be up to 8 numbers long.
Enter the:
To tell us if the services were in hospital items, select either:
- Yes
- No.
Select the item numbers provided in hospital or in a day surgery from the list of item numbers.
What To Include In Your Written Request For A Claim Denial Appeal Or Payment Dispute
Claim denial appeal
First-level appeal
Initial appeal requests for a claim denial must be submitted within 60 days from the date the provider receives the initial denial notice. Be sure to include the following information with your written appeal:
- Provider or supplier contact information including name and address
- Reason for dispute a description of the specific issue
- Copy of the providers submitted claim with disputed portion identified
- Copy of the plans original claim determination
- Documentation and any correspondence that supports your position that the plans original claim determination was incorrect, including any applicable medical notes and/or medical records , Medicare guidance, NCD or LCD when appropriate
- Appointment of provider or supplier representative authorization statement, if applicable
- Name and signature of the provider or providers representative
Second-level appeal
If you believe that we have reached an incorrect decision regarding your first-level appeal, you may file a request for a secondary review of this determination. A request for secondary review must be submitted in writing within 60 days of written notice of the first-level decision from Medicare Plus Blue. Decisions from this secondary review will be final and binding. Be sure to include the following information with your written appeal:
Medical payment dispute
First-level dispute
Second- level dispute
Dental payment dispute
Write to the following address:
Second-level dispute
You May Like: Does Medicare Cover Laser Surgery
State Health Insurance Assistance Program
SHIPs offer local, personalized counseling to people with Medicare and their families. They provide free information and counseling to help you with your Medicare questions. This includes your benefits, coverage, premiums, deductibles, and coinsurance. They will help you find information regarding filing of claims and complaints . You can locate information for your local SHIP office here.
Before You Submit A Claim
Payment of claims for MNT provided in the outpatient environment is dependent on several factors, including an individual’s benefits for MNT for their condition or reason , approved settings, and the network status of the RDN with the client/patient’s payer. Claims can be submitted to payers electronically through many vehicles, including practice management systems, provider portals, and claims clearinghouses. There may be some instances where paper claims are still used.
Also Check: Does Medicare Pay For Custom Foot Orthotics
Providers Have Access To Claims Details 24/7
The View Claims Details Online section of the site contains related features as well as information about patient history, copayments, physicians of record, plan summaries, and more. To view claim status by member, claim number, date of service, or provider tax identification number, simply log in and follow the prompts within the Claims Details section. Each claim summary includes the claim number, date of claim, patient ID number, patient name, billed amount, paid amount, claim status, and a link to HIPAA Status codes and other details.
To access this information, register now. All you need is your tax ID number or Social Security number, license number, and relevant personal and/or organization information. Most individual physicians may automatically register online and can log in to begin working on a case within minutes. Other providers may log in once they receive email verification, generally within two business days.
How To Bill Medicare Secondary Claims
Medicare isnt always primary. In this instance where Medicare is secondary, youll bill the primary insurance company before Medicare. Then, you can submit an Explanation of Benefits from the primary payor with the claim. The primary payer must process the claim first, and if they dont, your doctor may bill Medicare.
Recommended Reading: How To Pay For Medicare Without Social Security
Professional Paper Claim Form
Electronic claims must meet the requirements in the following claim implementation guides adopted as national standard under HIPAA:Providers billing a A/B MAC must comply with the ASC X12 837 Institutional Guide .Providers billing a Carrier or DMEMAC must comply with the ASC X12 837 Professional guide .Providers billing a B DMEMAC for prescription drugs furnished by a retail pharmacy must comply with the National Council for Prescription Drug Programs Telecommunications Standard D.0 and Batch Standard Version 1.2.
For more information please contact your local Carrier, DME MAC or A/B MAC or refer to the Medicare Claims Processing Manual , Chapter 24.
Help Is Available For Claims Reimbursements Complaints And Appeals
Need help with a Medicare claim? Know where to start.
- If youre covered by a Medicare Advantage Plan or Medigap, contact your carrier as directed in your Explanation of Benefits.
- For those covered by Original Medicare Parts A and B, call Medicare directly at 1-800-633-4227.
Other resources available to you to make sure your claims are satisfied, and your rights are protected, include:
Recommended Reading: Must I Take Medicare At 65
Obtain An Itemized Bill For Your Medical Treatment
Your itemized bill or bills for medical treatment proves your claims validity. Make sure your itemized bill contains the following information to ensure your claim is processed smoothly:
- The date of your treatment
- The place you received treatment
- Your doctor or medical suppliers name and address
- Description of each surgical or medical treatment or supply received
- Itemized charge for each treatment or medical supply
- Your specific diagnosis. This may not be necessary on the itemized bill if your Patients Request for Medical Payment form contains a thorough illness or injury description
If the bill you received from your health care supplier doesnt contain these details, contact your physician and request a new one with all the information Medicare requires.
When Do You Need To File A Medicare Claim
You generally shouldnt have to worry about filing a Medicare claim yourself. But in some rare cases, you may have to file one on your own.
In those cases, you must file a claim within 12 months of receiving medical care. If you miss that deadline, you may have to pay all the costs yourself.
You may have to file a claim yourself if you receive care from a nonparticipating Medicare provider or an opt-out provider.
Types of Providers Defined by Medicare
- Participating Providers
- Health care providers that accept Medicare and also accept the Medicare-approved amount for particular medical services or supplies.
- Nonparticipating Providers
- Health care providers who accept Medicare patients but dont agree to Medicare-approved prices. They may charge you up to 15 percent more than the approved cost.
- Opt-out Providers
- Health care providers who simply do not accept Medicare.
If you receive health care services from a provider who opts out of Medicare, you can file a claim for a Medicare reimbursement. It will cover only the approved amount Medicare pays for the service, so you may have to pay out-of-pocket costs.
You May Like: Does Medicare Cover One Touch Test Strips
Ama Disclaimer Of Warranties And Liabilities
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
How Medicare Claims Are Filed
Original Medicare includes Part A and Part B . Under this program, your Medicare providers typically send your claims directly to Medicare and you wont see a bill. In most cases, you pay a coinsurance or copayment and dont have to pay for the entire medical service up front. Medicare providers and suppliers must send their claims to Medicare for reimbursement.
There may be occasions when you need to pay for medical services at the time of service and file for reimbursement. For example, if your health-care provider isnt Medicare-assigned, you might have to pay for the service or supply and file for reimbursement.
Don’t Miss: How Do I Know What Medicare Coverage I Have
Cigna True Choice Medicare
Cigna True Choice Medicare H7849-038-000 is a 2022 Medicare Advantage plan without drug coverage provided by Cigna. It has a premium of $0.00.
More details on this plan are provided below. If you have questions, donât hesitate to use our site to reach out to a licensed Medicare agent for help today. Alternatively, if you know what plan you want, you can enroll online yourself using our site as well.
Plan Basics
