How To Pay For A Portable Oxygen Concentrator
Portable oxygen concentrators are great devices for those with a medical need for oxygen who live an active, on-the-go lifestyle. After choosing to buy a portable oxygen concentrator, youll likely have some questions, especially related to how youll pay for the device. There are several options when it comes to getting a portable oxygen concentrator.
The most pressing question might be how to get Medicare to cover the concentrator since theyre not exactly cheap. The answer isnt entirely straightforward or black and white. There are conditions that must be met and some hoops youll need to jump through.
Medicare has always paid for durable medical equipment like wheelchairs. But when it comes to medical oxygen equipment, the rules change a bit. Medicare does cover part of medical oxygen equipment, but not all of it. Theyve always paid a certain amount towards oxygen equipment, but in 2013, their reimbursement rate was slashed by 50 percent. In the past, durable medical equipment providers would cover the cost of the equipment and then bill Medicare later, but this was too costly for suppliers to cover.
Because of this, insurance providers are now likely to cover less expensive oxygen supplies instead.
What Equipment And Accessories Are Covered By Medicare
If you meet all the requirements, Medicare Part B will pay for specific equipment needed to provide oxygen therapy in your home.
Oxygen equipment and supplies Medicare will pay for:
- Medical-grade oxygen
- Systems that provide oxygen
- Containers that store oxygen
- Tubing or mouthpieces
Medicare will also cover equipment and supplies for continuous positive airway pressure therapy. CPAP machines, tubing and face masks are used to treat sleep apnea and similar conditions.
How Much Does It Cost To Rent An Oxygen Concentrator
Costs can vary significantly depending on what kind of oxygen concentrator you want to rent, what kind of insurance coverage you have and whether or not you meet the criteria to have your rental covered by insurance. Generally speaking, renting an oxygen concentrator can cost anywhere from $35 to $225 per week, depending on your individual insurance coverage.
Frequently Asked Questions About Durable Powers of Attorney for Health Care. LawHelp.org , D.C. Bar Pro Bono Center, 11 May 2015, www.lawhelp.org/dc/resource/frequently-asked-questions-about-durable-powe.
Choosing a Health Care Agent. Cigna, Cigna, 8 Dec. 2019, www.cigna.com/individuals-families/health-wellness/hw/medical-topics/choosing-a-health-care-agent-aa114352.
DeGenaro, Steve. O2 Orders 101. Healthcare Quality Association on Accreditation, Healthcare Quality Association on Accreditation, 4 May 2017, info.hqaa.org/hqaa-blog/o2-orders-101.
National Coverage Determination for Home Use of Oxygen . Centers for Medicare and Medicaid Services, United States Department of Health and Human Services, 14 Aug. 2020, www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=169.
Oxygen Equipment & Accessories. Medicare.gov, United States Department of Health and Human Services, 14 Aug. 2020, www.medicare.gov/coverage/oxygen-equipment-accessories.
Recommended Reading: When Can I Get My Medicare Card
Group I Criteria Include Any Of The Following:
Initial coverage for beneficiaries meeting Group I criteria is limited to 12 months or the physician-specified length of need, whichever is shorter.
Overview: Qualifying For Home Oxygen
First, if you want to receive home oxygen treatment youll need to meet the following criteria:
Read on for an in-depth description of this process.
Read Also: Does Kaiser Medicare Cover Dental
What About Portable Oxygen Concentrators
Unfortunately, Medicare will not pay for a portable oxygen concentrator if you are already using Medicares oxygen rental benefit. The reason for this is that Medicare pays the supplier the same amount whether the supplier gives you a portable tank or a portable concentrator.
Since the tanks are considerably less expensive than the concentrators, most DME suppliers will only provide you with tanks because it is cheaper for them to do so.
If this is truly an inconvenience, ask your supplier if they offer smaller liquid tanks that could also be billed to Medicare Part B.
Information provided on the Aeroflow Healthcare blog is not intended as a substitute to medical advice or care. Aeroflow Healthcare recommends consulting a doctor if you are experiencing medical issues or concerns.
TESTIMONIALS
It would be nice if every company had a team as friendly and wanting to help people as yours!
A.S.
is the most compassionate person I have ever worked withIm so thankful shes doing whats important.
R.M.
I really appreciate all of your assistance and prompt service. It has really been a pleasure doing business with your company.
P.W.
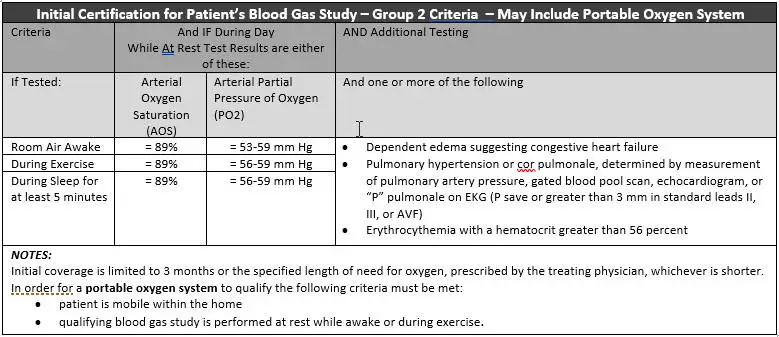
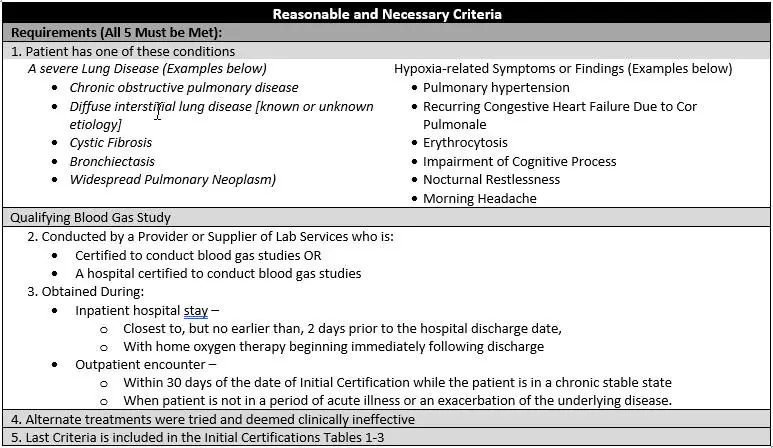
Medicare Home Oxygen Lcd Coverage
Coverage Indications, Limitations, and/or Medical Necessity
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements. For the items addressed in this local coverage determination, the criteria for reasonable and necessary, based on Social Security Act §1862 provisions, are defined by the following coverage indications, limitations and/or medical necessity.
For an item to be covered by Medicare, a detailed written order must be received by the supplier before a claim is submitted. If the supplier bills for an item addressed in this policy without first receiving the completed order, the item will be denied as not reasonable and necessary.
For some items in this policy to be covered by Medicare, a written order prior to delivery is required. Refer to the DOCUMENTATION REQUIREMENTS section of this LCD and to the NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES section of the related Policy Article for information about WOPD prescription requirements
Home oxygen is covered only when both the reasonable and necessary criteria discussed below and the statutory criteria discussed in the Policy Article are met. Refer to the Policy Article for additional information on statutory payment policy requirements.
Also Check: What Does Medicare Part B Include
When Is Oxygen Therapy Used
According to the National Heart, Lung, and Blood Institute , your lungs normally gather enough oxygen for your bodys needs from the air you breathe. The oxygen enters your bloodstream through tiny blood vessels that cover your lungs air sacs , and its carried to the heart to be pumped to organs throughout your body. If structures in your lungs are damaged or compromised from illness or disease, your lungs may not be able to absorb enough oxygen from the air. Oxygen therapy delivers oxygen to the lungs to help your body get the right amount it needs.
According to the NHLBI, doctors use oxygen therapy to treat the following conditions:
- Chronic obstructive pulmonary disease
- Heart failure
- Cystic fibrosis
- Sleep apnea
Your doctor may order tests such as an arterial blood gas test or a pulse oximetry test to measure the amount of oxygen in your blood to determine whether oxygen therapy is right for you. In most cases, people on oxygen therapy may feel less fatigue and shortness of breath it can also increase the lifespan of some people with COPD, according to the NHLBI.
The Inogen One: The Right Choice For Home Oxygen
An Inogen One Medicare rental can help you enjoy the benefits of an innovative portable oxygen concentrator at a reduced cost. The Inogen One can help you discover what it is like to enjoy improved freedom, mobility and independence, all while receiving your oxygen treatments. If you are concerned about how to get an oxygen tank in and out of your home or car, a portable oxygen concentrator is a great choice for you. Small, compact and lightweight, Inogens portable oxygen concentrators allow you to get the oxygen you need at home or on the go. If this sounds like the right choice for you, look into your Medicare oxygen requirements and find out if you can get an Inogen One Medicare rental today. Contact Inogen to find out more.
Don’t Miss: Is Medicare A Social Security Benefit
Does Medicare Cover Portable Oxygen Concentrators
While Medicare covers small liquid portable tanks, oxygen concentrators are not part of the coverage. Oxygen concentrator devices are much more expensive.
This is why suppliers choose to cover the smaller portable oxygen tanks instead since its much more cost-effective. Medicare will only approve one payment for oxygen therapy.
Qualifying For Medical Oxygen
Not everyone who is short of breath needs supplemental oxygen. However, if your oxygen levels show that you are chronically hypoxemic, meaning you have a long-term, insufficient supply of oxygen in your blood, you are probably a good candidate.
In order for Medicare to pay for oxygen and the additional supplies needed to administer it, you must have Medicare Part B coverage.
If your healthcare provider thinks you would benefit from home oxygen, you’ll want to follow the steps as outlined by Medicare. Before calling the oxygen supply company, make sure you have a practitioner for the home oxygen equipment and supplies you’ll need, from the oxygen concentrator all the way down to the tubing. If you don’t have a practitioner’s order, Medicare won’t cover the supplies. Make sure your prescription is signed and dated by your medical professional.
Once that is set, make sure your healthcare provider has documented your need for oxygen in your medical record. Medicare will request your records before approving your home oxygen, and if your condition is not well-documented, they may deny your claim.
Make sure that your oxygen supply company has the order in hand before billing Medicare. They must also keep the order on file.
Your likelihood of being approved increases if you have:
Read Also: Where Can I Get Medicare Information
Are You Eligible For Medicare
Before you ask, Are portable oxygen concentrators covered by Medicare? make sure you qualify for Medicare. If you are 65 or older, you have a documented disability or you have end stage renal disease, you are eligible for Medicare. From there, see your doctor to ensure you meet all the criteria for getting your portable oxygen concentrator covered by Medicare.
What Does Oxygen Equipment Rental Include
Medicare oxygen equipment is rented for 36 months. In addition, medical equipment suppliers must furnish the oxygen equipment and related supplies for an additional 24 months if necessary.
Your monthly rental includes the following oxygen accessories and services:
- Tubing or mouthpiece
- Oxygen contents, including liquid oxygen and oxygen concentrate
- Maintenance of the oxygen machine
Medical suppliers must provide both the equipment and related supplies for up to 5 years, assuming you continue to have a medical need for oxygen.
Also Check: Does Medicare Cover House Calls
Portable Oxygen Concentrator Medicare Insurance
Many Medicare beneficiaries who have needs for oxygen equipment, including POC, have always sought to know the government-controlled healthcare stance on oxygen tanks and concentrators. Some of the common questions asked have been in the following directions are there Medicare Supplement Plans with 100% Portable Oxygen Machine Coverage? If there are, is it on all Portable oxygen concentrators, or are there certain Prices of Portable Oxygen Concentrator Covered by Medicare? We will be answering all of these questions to clear the air on how far Medical care coverage goes and if they cover POCs.
Medicare beneficiaries have always had durable equipment such as wheelchairs covered by the health system, and this was also the case for medical oxygen tanks and concentrators. However, the whole game changed after the healthcare reimbursement rate was cut down by 50 percent in 2013. Medicare still funds the supply of oxygen equipment but only a part of it.
According to Medicare, there are specific criteria that must be satisfied by patients before they can be considered eligible for oxygen equipment, including POCs. If the requirements are met, they will help cover part of the cost. The conditions are outlined below:
Consider Dipping Into Your Ira
For certain things, you can withdraw money from your IRA without facing a harsh financial penalty. Typically, if you withdraw money before age 59.5, you can face an additional 10 percent early-distribution penalty on taxable income. But there are some medical exceptions.
If you are uninsured or your medical expenses total more than your insurance will cover that year you may be able to take penalty-free distributions from your IRA. Its important to remember this only applies if youre paying medical expenses greater than 7.5 percent of your adjusted gross income.
If youre unemployed, you can take penalty-free distributions to pay for medical insurance. But you must meet certain conditions:
- You lost your job.
- You received unemployment compensation for 12 weeks.
- You received the distributions during the year you received the unemployment payment or the following year.
- You received the distributions no later than 60 days after you got another job.
You also wont be penalized if youre disabled and can be for any purpose. However, a physician must determine that you arent able to work due to a physical or mental disability. The disability must be expected to result in your death or be determined to last for an indefinite period.
Related Articles
Recommended Reading: Does Medicare Pay For Entyvio
What Happens After I Rent My Equipment For 36 Months
After renting the suppliers portable oxygen equipment, it is expected that they keep the oxygen concentrator in good working order and carry out continuous maintenance on it as needed. This obligation could take up to a maximum of five years if you need the POC for that long. The supplier will not charge you for any of these services.
The POC supplier must provide everything you will need for all five years and ensure that everything is in top condition. Also, it is important to note that the supplier owns this product throughout the five years.
Your supplier will end the contract of supplying you with the portable oxygen concentrator and all its related services after five years elapse. If you still need oxygen support, you can decide to ask for renewal, repeat the payment terms, or demand a new supplier. The payment process remains unchanged as well.
With the new supplier or renewed contract, a new 36 months obligation will begin, lasting for up to another five years if you need it.
Medicare Part B Provides Coverage For Durable Medical Equipment Like Portable Oxygen Concentrators
Although it helps pay for a variety of oxygen equipment and accessories, Medicare only covers portable oxygen concentrators under specific circumstances.
The difference is in that word, “portable.” Medicare coverage for durable medical equipment specifically states that beneficiaries must require said equipment for use in the home. For Medicare to cover portable oxygen concentrators , your doctor must certify that you have a near-constant need for oxygen AND are mobile within your home. You must also meet all other requirements to qualify for an oxygen system.
You May Like: Does Medicare Cover Ice Therapy Machines
Procure A Medical Record
You must have medical record that contains sufficient documentation of a medical condition to substantiate the need for oxygen therapy in the home.
Included in this medical record:
- Diagnosis
- Clinical course
- Prognosis
- If portable oxygen is needed, an indication that you are mobile within the home
- Nature and extent of functional limitations
- Other therapeutic interventions and results
- Experience with related items
Top Reasons For Denied Claims In Northeast Region Of The Us
According to Medicare, in the Northeast region, where the denial rate for oxygen claims is currently at 76.33%, the primary reasons are:
Read Also: How To Apply For Medicare Through Spouse
Medicare Portable Oxygen Concentrators Payment
It is very important to note that Medicare does not fund the purchase of portable oxygen concentrators or any other oxygen equipment. They only cover the equipments rent, and you will have to pay 20% of the total fee.
You will also be the one to get the supplier. It is advisable you get a recommendation from your doctor as it can be very difficult to get a Medicare-approved supplier due to its competitive bidding. The funding provided will cover up to 36 months of rent. Medicare states that After even after the 36 months elapse, your supplier will continue to provide the portable oxygen concentrator for an additional 24 months, which will also be covered as arranged. Your supplier is expected to provide the POC for up to 5 years and even more than depending on how long you will have the medical need.
The monthly payments will cover the suppliers need and the maintenance of your oxygen Concentrator.
