What Should Caregivers Know About Medicare
Medicare is a federal government health insurance program primarily for people age 65 and older. It may also cover younger adults with disabilities.
There are different plans and coverage options within Medicare.
Your loved one or family member may be enrolled in Original Medicare, which includes two components: Part A for hospital insurance and Part B for medical coverage.
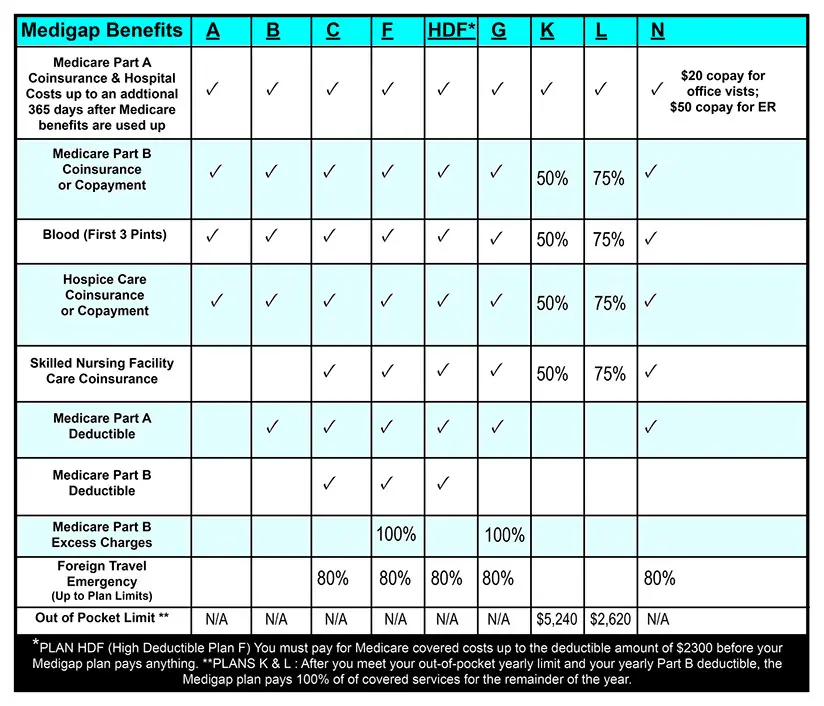
In this case, your loved one may also have a stand-alone Part D prescription drug plan. Some Original Medicare beneficiaries also have a supplemental insurance plan, also known as Medigap, which helps cover deductibles and other costs.
Part D and Medigap plans are administered by private companies that Medicare reimburses.
Alternatively, your friend or family member may be enrolled in a Medicare Advantage, or Part C, plan.
This option is also administered by a private company. Medicare Advantage plans must provide the same basic coverage as Original Medicare but may also bundle other benefits such as drug coverage, vision, hearing and dental into a single plan.
All Medicare enrollees are issued a red, white and blue Medicare card. They may also have a separate Medicare Advantage or Part D card, if theyre enrolled in these programs.
If you cant locate these cards, you and your loved one can call the Medicare helpline together. Or, your loved one can complete a form authorizing Medicare to release information to you.
To learn more, call Medicare at 1-800-MEDICARE .
Cost Of Nursing Homes Vs In
Options for in-home care providers include homemaking service providers, which can help older people with activities of daily living and household tasks like cleaning, cooking, and running errands. Home health aides are another option aides are trained to provide more extensive care, while also serving as companions. In some cases, individuals and families may choose skilled in-home nursing care, which is typically provided by a registered nurse or certified therapist who can administer medication and monitor their vitals regularly.
However, the more intense the medical care required, the more expensive it will be. For example, typical homemaker services cost about $163 per day, home health aides cost $169 per day, and for a 10-hour work day, a typical registered nurse would make $387. Though, in most cases, these types of services are not needed all day, or even every day.
Does Medicare Cover Living In A Nursing Home
The simple answer is no. Just like most health insurance plans, Medicare does not pay for long-term care stays. That means Medicare will not pay for any type of long-term residenceincluding assisted living and memory care facilities. However, it can help pay for the necessary doctors services and medical supplies a person might need while staying at such a facility.
In a situation where someone is admitted to the hospital and then needs further oversight to recover, Medicare will cover part of the short-term rehab stay, which could take place in a nursing home.
Medicare covers a portion of the short-term stay up to 100 days, as long as the patient continues to get better. If the patients health is not deemed to be improving, coverage will be terminated. But if the patient is making progress and needs to exceed the 100-day limit, an appeal for a longer stay can be submitted.
Read Also: Does Everyone Get Medicare When They Turn 65
Also Check: Does Medicare Cover Aba Therapy
Medicaid Eligibility For Nursing Home Care
Medicaid coverage, like many other financial assistance programs, is dependent on a variety of factors such as age, financial status, assets, and level of care. If you need assistance for long-term nursing home care, you should check to see if you meet the Medicaid eligibility requirements in the state that youre currently residing in. Typically, one of the requirements of eligibility is that a majority of your income needs to be used to pay for the cost of your nursing home.
How Much Do I Pay If Im In A Skilled Nursing Facility
The portion of the costs that you pay depends on the duration of your eligible stay in a skilled nursing facility. Youll have the following copayments for each benefit period:
- $0 for days 1 to 20
- $194.50 a day in 2022 for days 21 to 100
- All costs days 101 and beyond
A Medicare supplemental policy, better known as Medigap retiree coverage or other insurance may cover the copay for days 21 to 100 or add more coverage.
Keep in mind
Medicare doesnt pay for the considerable cost of long-term care in a nursing home or other facility. But you may have other options to help cover long-term care costs.
Private pay. Many individuals and families pay out of pocket or tap assets such as property or investments to pay for long-term care. If they use up those resources, Medicaid may become an option.
Long-term care insurance. Some people buy long-term care insurance that may pay for custodial care in a nursing home or assisted living facility or for a caregiver to come to their home. To qualify for payouts, you generally must need help with at least two activities of daily living or provide evidence of cognitive impairment.
Veterans benefits. Military veterans may have access to long-term care benefits from the U.S. Department of Veterans Affairs .
Recommended Reading: Does Medicare Pay For Custom Foot Orthotics
What Does Medicare Cover
It is important to understand what your Medicare does and does not cover. Medicare Part A covers hospital costs and Medicare Part B covers outpatient medical costs for preventive and medically necessary care. If you have a Part D prescription drug plan, your prescription drugs are covered. Medicare Advantage plans cover the same healthcare expenses as Medicare Part A and Part B, with the option for additional packages including prescription drug coverage. Medicare Supplements help cover the out-of-pocket expenses left over from Medicare Part A and Part B.
Long term care is not the only thing left out of Medicare coverage. Medicare does not cover routine dental, vision, hearing, or podiatry care, nor does it cover chiropractic care, acupuncture, or cosmetic procedures. If you wear glasses or contacts, go to the dentist, wear hearing aids, or regularly visit non-medically necessary care practices, you will want to find supplemental coverage to help cover your expenses.
Medicare Nursing Home Coverage Eligibility
For your nursing home costs to be covered by Medicare, you must meet the following criteria:
- Your doctor must determine that your condition requires skilled nursing care
- You must have first had a qualifying hospital stay of at least 3-day-consecutive inpatient hospitalization
- You must receive care at a Medicare-approved skilled nursing facility
Recommended Reading: How To Get Medicare Number Without Card
Paying For Hospice Care
Medicare, Medicaid, the VA, and most private insurance companies cover hospice care. Insurance starts as soon as you are admitted into the hospice program.
Keep in mind VA benefits vary. In general, benefits for combat or wartime vets are not based on income. Eligibility or peacetime vets may be income-based. Vets must have received an honorable, other than honorable, or medical discharge to qualify. They usually must have been on active duty for at least 24 months.
In New York State, insurers are required by law to cover hospice care. But private insurance companies may limit benefits and coverage. If you have private insurance, check with your plan.
What Skilled Nursing Facility Costs Does Medicare Cover
Medicare can cover many of the services you receive in a skilled nursing facility, such as:
- A semiprivate room and meals
- Skilled nursing care
- Medical social services and dietary counseling
- Medications, medical equipment and supplies used in the facility
- Occupational therapy, physical therapy or speech and language pathology services if needed to meet your health goal
- Ambulance transportation if needed to receive necessary services that arent available in the facility
Don’t Miss: Does Medicare Cover Life Alert Cost
Medicare Coverage Requirements For Skilled Nursing Facility Care
SNF care is nursing and therapy that can only be performed or supervised by professionals or technical personnel. Medicare Part A may help cover SNF care in certain conditions for a limited time if all of these conditions are met:11
- You have Part A and have days left to use in your Medicare
- You have a qualifying hospital stay
- Your doctor decided that you need daily skilled care
- The SNF where you get skilled services is certified by Medicare
- You need these skilled services for a medical condition thats either:
- A hospital-related medical condition treated during your qualifying 3-day inpatient hospital stay, even if it wasn’t the reason you were admitted to the hospital
- A condition that started while receiving care in the SNF for a hospital-related medical condition
Q: Can You Give Some Examples Of How A Palliative Care Program Might Help A Person With Parkinsons
A: Patients who attend our programs Multi-Disciplinary Clinic are able to address multiple needs by seeing all of their specialists and therapists in one day. For example a patient may see their neurologist, social worker, and even their physical, occupational and speech therapists in back-to-back visits that minimizes travel and maximizes communication between the specialists. Pre-pandemic, another great benefit of this program was that we were able to provide home visits to address the medical and social needs of a patient and their family. Now, we are using technology and helping patients and families with telemedicine visits that utilize software, such as Zoom.
Don’t Miss: When You Have Medicare And Medicaid Which Is Primary
How Much Will I Pay For Home Health Care With Medicare
For the home health services they cover, Medicare coverage is quite complete. You will pay nothing out of pocket for covered home health care services.
However, you may require durable medical equipment as part of your care. This includes, but is not limited to, such items as:
- Blood sugar monitor
Under Original Medicare, you will pay 20 percent of the full cost for any durable medical equipment you need. If you have Medicare Advantage or a Medigap plan, contact your plan providers for details.
Pro Tip: Deciding between assisted living or home care? Our experts have taken a deep dive into the difference between assisted living and home care so you can decide what is best for you or your loved one.
Recommended Reading: Dentist That Take Medicaid In Michigan
Medicare Home Health Care
Intermittent or short-term home health services are covered under Medicare Part A and Part B. These services must be provided by a Medicare-certified home health agency that works with your doctor to manage your care.
To be eligible for Medicare coverage:
- Your doctor must order it medically necessary that you receive intermittent skilled nursing care or outpatient therapy services at home. Medicare defines âintermittentâ care as care given less than seven days a week or less than eight hours a day, for no longer than 21 days. If you need more than intermittent nursing care, Medicare will generally not cover it except in special circumstances.
- Your doctor must determine that your condition will improve, and that your need for home health services is temporary.
- You must be homebound, meaning you canât leave your home without assistance, or it might be dangerous to leave due to your health condition. Homebound doesnât necessary mean bed-bound. Youâre still considered homebound if you leave your home occasionally, for short periods of time, even for non-medical purposes like attending religious services.
Medicare covers your home health services over a 60-day period, after which the doctor must review your plan of care. However, there is no limit to the number of times your doctor can reorder this care for you, as long as it remains medically necessary to treat your condition.
Medicare-covered home health care may include:
Read Also: Does Medicare Cover Outpatient Services
Texas Medicaid Will Pay For A Nursing Home Assisted Living Or Home Health Care When A Patient Needs Skilled Nursing Care
In Texas, long-term care is expensive, whether in a nursing home, assisted living facility, or home health care. Medicare coverage for long-term care is very limited, private health insurance policies generally do not cover long-term care, and few people have purchased private long-term care insurance policies. For Texans needing long-term care, Medicaid is the most common source of funding.
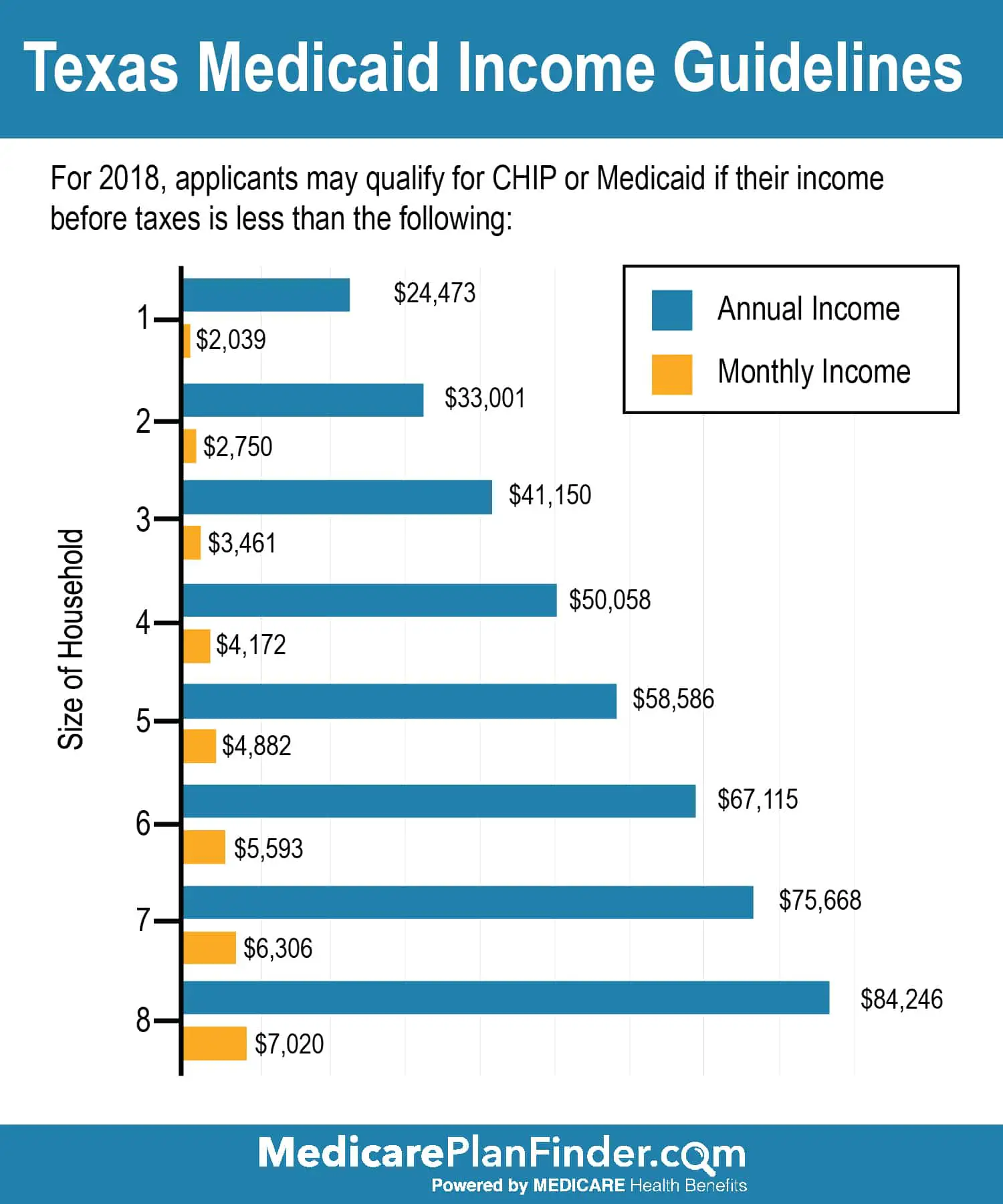
Medicaid is funded by both federal and state resources, and it provides health coverage to over four million Texans. There are many different ways to become eligible for Medicaid in Texas, and Texas has specific eligibility rules for long-term care services like nursing homes, assisted living facilities, and home health care services.
When A Nursing Home Is Medically Necessary
Medicaid will pay for a nursing home only when it is “medically necessary.” In Texas, for a nursing home to be considered medically necessary, you must have a medical condition that is so serious that you need the level of nursing care that is only available in an institution. Your doctor must document your medical condition and must prescribe skilled nursing services to be provided to you on a regular basis in an institutional setting. Nursing care includes things like giving shots, inserting a feeding tube or catheter, treating bed sores, and changing wound dressings.
For Medicaid to keep paying for your nursing home stay, a doctor has to certify at least every six months that you meet the standard for medical necessity.
If you need only custodial care , for instance, because you fall often or because you have dementia and tend to wander, then Medicaid may find that a nursing home stay is not medically necessary because you do not need a skilled nurse.
Recommended Reading: What Preventive Services Are Covered By Medicare
Nursing Home Costs By State And Region
When considering applying for Medicaid, many individuals want to know the cost of nursing home care in their geographic area. At the time of writing , the nationwide average daily cost for a shared room is $260. A shared room is important because typically Medicaid will only pay for shared rooms, not private rooms.
The range across the country goes from a low of $180 / day in parts of Texas and Louisiana to over $1,000 / day in parts of Alaska. The table below specifies costs for 480 geographic areas across 50 states and Washington, DC. The data contained in the table is the average cost for private pay. Private pay means were an individual to cover the full cost of nursing home care without any public assistance , this is the amount they would pay.
Medicare and MedicaidMedicare will pay 100% of the cost of nursing home care for the first 20 days in which a beneficiary resides in a nursing home. For days 21 100, Medicare will continue to pay a portion of the cost, but in 2022, the nursing home resident will have a copayment of $194.50 / day. After 100 days, Medicare does not pay for nursing home care.
Medicaid will pay 100% of the cost of nursing home care for its beneficiaries. However, to be eligible for Medicaid nursing home care, the patient must have very limited income and very few financial assets . Medicaid eligibility criteria is state-specific. See eligibility data for all 50 states.
| Nursing Home Costs by State and Region 2021 |
|---|
| State |
Does Medicare Cover Home Health Care For Dementia Patients
Dementia is not a specific disease but a general term for the impaired ability to remember, think, or make decisions that interferes with everyday activities, according to the Centers for Disease Control and Prevention . The Alzheimerâs Association reports that approximately 6.2 million people in the United States are currently living with some form of dementia, and Medicare can be a financial resource for those who have been diagnosed.
Also Check: Can I Change Medicare Plans Anytime
How Do I Use The Provider Name Search
Level Of Care Eligibility
Medicaid eligibility differs on a state-by-state basis, depending on the level of care that is medically necessary and needed. In order to qualify for Medicaid, individuals must be able to prove that they require a level of care that meets certain criteria or requires a level of personal care assistance.
The definition of level of care varies from state to state, but in general, it refers to assistance to those who lack cognitive function, the inability to engage in activities of daily living, and mental and behavioral health issues. These factors are just some tools that are used to assess the level of care at nursing homes for older adults, according to the American Council on Aging. Keep in mind that the level of care varies depending on the state youre in, so the criteria that might make one eligible in one state, may not apply to the other.
Also Check: Is Estring Covered By Medicare
Does Medicare Pay For A Nursing Home
Unfortunately, Original Medicare doesnt cover the cost of a long-term stay at a nursing home, but certain parts of Medicare can pay for medically necessary or essential services at nursing homes. Some of these services include meal preparation, prescription drugs, durable medical equipment, counseling, and other services. Overall, Original Medicare covers short-term visits, but not long-term stays.
What Parts Of Nursing Home Care Does Medicare Not Cover
Medicare doesnt cover most aspects of nursing home care. This includes custodial needs, such as bathing, eating or moving around. It also doesnt cover room and board for any long-term nursing home stay, including hospice care or the cost of a private room. Lastly, Medicare wont cover your skilled nursing facility stay if its not in an approved facility, so its important to know what institutions it has approved in your area.
Read Also: Does Medicare Pay Anything For Nursing Home Care