Does Insurance Cover Weight Loss Surgery
Making major changes is never simple, and with weight loss surgery, one of the greatest burdens is the cost. For the average individual, bariatric surgery isnt something they can afford to pay for out of pocket.
At the same time, for many people, it is the only solution left to their battle against obesity and an essential tool in ensuring their overall health and wellness. This leads to a brand-new battle: affording weight loss surgery.
Does insurance cover weight loss surgery? Yes and no. Lets dig into the topic to get a better understanding of the relationship between insurance providers and bariatric procedures.
What Is Biliopancreatic Diversion With Duodenal Switch
Biliopancreatic diversion with duodenal switch is similar to gastric bypass, in that it creates a smaller stomach and bypasses most of the small intestine. However, instead of creating a small, pouch-like stomach, BPD/DS uses sleeve gastrectomy to remove 80 percent of the stomach. The gastric sleeve leaves a tube-shaped stomach that resembles a banana. The patient gets the same benefits feeling full more quickly thanks to a smaller stomach and malabsorption of calories. Unfortunately, this also leads to the same nutrition deficiencies seen in gastric bypass. The procedure is extremely effective, although it has more risks than either gastric bypass or LAP-BAND. Typically, your doctor will only recommend BPD/DS if your body mass index is over 50.
Recommended Reading: What Is Bernie Sanders Plan For Medicare For All
Other Cpt Codes Related To The Cpb:
43659 Cholecystectomy 74240 Radiologic examination, upper gastrointestinal tract, including scout abdominal radiograph and delayed image, when performed single-contrast study 74246 Radiologic examination, upper gastrointestinal tract, including scout abdominal radiograph and delayed image, when performed double-contrast study, including glucagon, when administered
Don’t Miss: Is Healthfirst Medicaid Or Medicare
How Long From Consultation To Bariatric Surgery
Answer: Weight loss surgery requires a commitment to lifestyle changes, including what you eat and how often you exercise. Your surgeon will help you set the groundwork, so youre mentally and physically prepared for life after bariatric surgery. The entire process, from consultation to surgery, generally takes about six months to complete. Weight loss surgery is a tool that can help you kick start a healthier lifestyle and maintain your weight loss.
Conversion Of Sleeve Gastrectomy To Roux
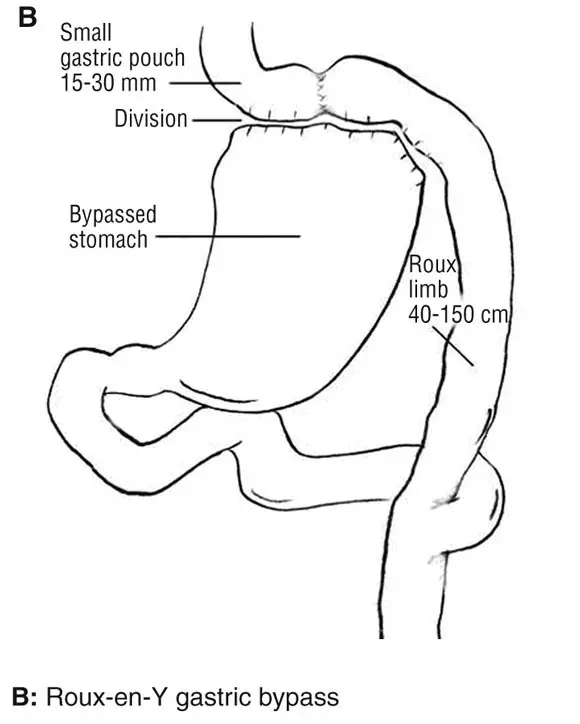
Langer and colleagues noted that due to excellent weight loss success in the short-time follow-up, sleeve gastrectomy has gained popularity as the sole and definitive bariatric procedure. In the long-term follow-up, WL failure and intractable severe reflux can necessitate further surgical intervention. These investigators carried out a retrospective analysis of laparoscopic conversions from SG to Roux-en-Y gastric bypass to assess the efficacy for reflux relief and WL success 8 out of 73 patients underwent conversion to RYGB for severe reflux or weight regain after a median interval of 33 months following laparoscopic SG . In 1 of the patients, a banded gastric bypass was performed. In both groups, conversion to RYGB was successful, as proton pump inhibitor medication could be discontinued in all patients presenting with severe reflux, and a significant WL could be achieved in the patients with WR within a median follow-up of 33 months. Post-operative complications were observed in only 1 patient as leakage at the gastrojejunostomy was successfully treated by temporary stent placement. The authors concluded that conversion to RYGB was an effective treatment for WR or intractable reflux symptoms following SG. Therefore, SG could be performed, intended as the sole and definitive bariatric intervention, with conversion from SG to RYGB as an exit strategy for these complications.
Also Check: Should I Get Medicare Part C
What Is The Safest Form Of Weight Loss Surgery What Types Of Surgery Are There
Answer: Weight loss surgery, also known as bariatric surgery, is a tool to produce significant weight loss for morbidly obese people. If you have unsuccessfully battled a serious weight problem, Baylor Frisco can help you take control of your health and change your life. We have devoted the necessary resources to provide you with comprehensive care, including patient education, pre-surgical counseling, advanced surgical options, and long-term post-surgical care. Baylor Frisco offers several different kinds of weight loss surgery designed to help patients manage their weight including:
Lap Band Surgery: Medicare Coverage
Medicare may cover lap band surgery if your Medicare-assigned doctor determines that you meet certain criteria related to obesity. To be covered, you generally must meet all of the following criteria:
- Have a body mass index greater than or equal to 35.
- Have at least one co-morbidity related to obesity.
- Have previously received unsuccessful medical treatment for obesity.
Also Check: Where Can I Sign Up For Medicare
You May Like: Can You Get Medicare Insurance At 62
Medicaid And Bariatric Surgery
Following bariatric surgery, you may need to make adjustments to your lifestyle, such as dietary changes or limits on specific foods. You may be able to take some drugs to help you adjust to the changes brought on by the operation, at least initially. Medicaid patients are covered for post-operative care and follow-up consultations. To avoid further harm, you must follow the directions of your doctor and the surgical rescue team. Any form of bariatric surgery has the potential for complications. However, with proper care, you should be able to fully recover. Examine the Medicaid Requirements
The patient must fulfill the following conditions to be eligible for weight loss surgery while on Medicaid:
You have a BMI of 35 or above and at least one comorbidity such as hypertension, sleep apnea, high cholesterol, or diabetes.
If you are under the age of 21, you must have a Body Mass Index of greater than 40. You must have at least one of the above-mentioned comorbidities.
The initial step is critical. Your doctor should write you a note suggesting weight reduction surgery as a medical necessity.
They must have a mental health evaluation that indicates their capacity to make the required lifestyle changes for weight loss.
You must show that you are attempting to manage your weight and comorbidities with conventional therapy. You must, however, be able to produce documents proving that you failed.
Gastric Balloon Cost Insurance & Discounts
The average gastric balloon cost is $8,150. It is usually not covered by insurance, although your doctor may be able to get some of the costs covered.
The price can often be reduced through tax deductions and special doctor-specific discounts.
This page covers everything you need to know about paying for the gastric balloon procedure.
Don’t Miss: What Is The Best Medicare Supplement Insurance Company
Will Medicare Pay For Skin Removal After Weight Loss Surgery
Medicare doesnt cover cosmetic surgery, but it may cover cosmetic procedures if they are medically necessary for a particular situation.
Medicare lists a panniculectomy, defined as surgery to remove excess skin and tissue from the lower abdomen, among a list of outpatient services that may be covered because of accidental injury or to improve the function of a malformed body part.
As with bariatric surgery and other surgical procedures, you should work with your healthcare provider to determine if Medicare will cover the procedure.
You May Like: How Much Does Medicare Pay For Inpatient Psychiatric Care
Who Is Not Eligible For Bariatric Surgery
An extensive pre-surgery screening process is required in most cases, which would involve a consultation with a team of professionals, including a doctor, dietician, psychologist, and surgeon, according to Mayo Clinic.
These experts will look further into your weight history, diet attempts, eating habits, exercise, stress, and other factors. They will also evaluate your health history, such as blood clots, heart problems, kidney stones, or nutritional deficiencies. Any of these may deem a person ineligible for bariatric surgery
Other factors include your mental health conditions, or whether or not you have a history of a binge-eating disorder, substance abuse, anxiety, major depression, schizophrenia, severe bipolar disorder, or issues related to childhood sexual abuse.
Even if you are approved for bariatric surgery, it could potentially be delayed or canceled if your team of doctors finds:
- You are not psychologically or medically ready for surgery
- You have not made appropriate diet or exercise changes
- You have gained weight during the evaluation
Read Also: Does Part B Medicare Cover Dental
Prophylactic Mesh Placement For Prevention Of Incisional Hernia After Open Bariatric Surgery
In a systematic review and meta-analysis, Dasari and colleagues examined if mesh prevents post-operative incisional hernia in open and laparoscopic bariatric surgery patients. A total of 7 studies met inclusion criteria. These investigators abstracted data regarding post-operative IH development, surgical site infection, and seroma or wound leakage and performed a meta-analysis. The prophylactic mesh group had significantly decreased odds of developing IH than the standard closure group . No included studies evaluated outcomes after prophylactic mesh during laparoscopic bariatric surgery. The authors concluded that prophylactic mesh during open bariatric surgery appeared to be beneficial in reducing post-operative IH without significant increasing the odds of surgical site infection or seroma or wound leakage. Moreover, they stated that higher quality studies, including those in laparoscopic patients, and cost-utility analysis, are needed to support routine use of this intervention.
Will A Medicare Advantage Plan Cover Weight Loss Surgery
Coverage for any procedure with a Medicare Advantage plan can change depending on a range of circumstances. UnitedHealthcare has an Advantage plan that covers weight loss surgery after meeting the plans guidelines.
Advantage plans determine the level of benefits and costs of service based on the service area, health condition, and medical necessity.
Medicare Advantage beneficiaries should contact their policy directly if unsure about coverage and benefits.
Also Check: Does Medicare Cover Diabetic Shoes
Does Medicare Cover Weight Loss Surgery
Weight loss surgery is the last option for many people that are overweight or rather considered obese. These individuals have tried other types of weight loss programs and been unsuccessful in reaching the right weight for them. Being overweight is not only about the way a person looks and the quality of living, but it also comes with medical conditions that can be a detriment to the health of the individual. Some of the problems associated with obesity include heart disease, diabetes, high blood pressure, sleep apnea, and digestive issues.
Paying for weight loss surgery can be a challenge for many patients that seek the help. The average cost of bariatric surgery can range from $17,000 to $30,000 depending on the surgery type and the location of the surgical facility. Medicare does cover some weight loss surgery types such as gastric bypass, lap gastric band, and gastric sleeve surgery. There are several requirements that must be met in order for the surgery to be paid for by the healthcare plan. Not only must the patient fit the requirements set by Medicare coverage, but the facility must also be an accredited Bariatric Center of Excellence. You will need to find a Medicare-approved center from the Centers for Medicare and Medicaid Services.
*** Thanksgiving Recipes ***
These roasted brussels sprouts get a fair amount of spice from the crushed red pepper flakes, which cuts
After trying every turkey-roasting method under the sun, Ive finally settled on this as absolutely the
We love how the cinnamon-scented streusel topping lets the juicy berries peek through.
Italian sausage and a heap of Parmesan cheese lend signature flair to the easy Thanksgiving dressing
Its all about the layers and ruffles in this dramatic seasonal pie.
Poach quince in rosé with a dash of cocktail bitters and a few warm spices, then assemble into a tart
Leave the sausage, nuts, dried fruit behind in favor of this easy, vegetarian-friendly stuffing recipe
Alton Browns turkey brine recipe from Good Eats will give you a flavorful Thanksgiving turkey with juicy
Bone-in turkey breasts are easy to find, and as impressive as a whole bird when you roast them in butter
This recipe was handed down by my great-grandmother. It is a family favorite that we make every Thanksgiving.
Cutting leeks into large pieces gives them a presence equal
This crunchy crumble is the perfect topping for an ice cream sundae, easy apple crumble, or our Build-Your-Own
You May Like: Do Any Medicare Supplement Plans Cover Dental And Vision
Does Insurance Cover Weight Loss Surgery And How Do I Get Weight Loss Surgery Approved
Answer: Insurance coverage varies for weight loss surgery procedures between insurance carriers. It is important that you call your insurance provider to determine if your policy covers surgical weight loss. Insurance companies often require medically supervised diets that can span up to 6 months. The length of time for insurance approval depends on each insurance plan and its qualifications.
Important Questions to Ask Your Insurance Provider:
- Do I have coverage for weight loss/bariatric surgery? Provide them with the diagnosis code E66.01.
- What are the criteria for surgery?
- Co-morbidities how many and which medical conditions qualify
Medicare Part B Costs
Your out-of-pocket costs with Medicare Part B include monthly premiums, coinsurance, and the annual deductible. In 2022, the Part B annual deductible is $233. You must pay this amount out-of-pocket before Medicare begins paying its share.
You also have a monthly premium of $170.10 even if you join a Medicare Advantage plan. Finally, there is the standard Part B coinsurance of 20 percent of the Medicare-approved cost. So, if your surgery is an outpatient procedure and costs $20,000 , your co-insurance would be $4,000. That is in addition to any other costs accrued prior to your surgery.
You may also have Part B costs if you have inpatient surgery, as doctor services received while in the hospital still fall under Part B. Outpatient surgery performed in a hospital setting may also have a copayment. It is always a good idea to talk to your healthcare providers to form a better idea of your costs for any procedure.
Recommended Reading: What Is Magi For Medicare
Body Mass Index As A Criterion For Candidacy For Obesity Surgery
Surgery for severe obesity is usually considered an intervention of last resort with patients having attempted other forms of medical management but without achieving permanent weight loss . Surgery is indicated for persons with severe obesity or for persons with a BMI of 35 kg/m2 or more and serious co-morbidities such as diabetes, coronary heart disease, or obstructive sleep apnea. Ideally patients selected for surgery should have no major perioperative risk factors, a stable personality, no eating disorders, and have lost some weight prior to surgery. The patient’s ability to lose weight prior to surgery makes surgical intervention easier and also provides an indication of the likelihood of compliance with the severe dietary restriction imposed on patients following surgery.
Rationale For Intensive Multicomponent Behavioral Intervention
The U.S. Preventive Services Task Force recommends that clinicians offer or refer obese adults to intensive, multicomponent behavioral interventions . The USPSTF found adequate evidence that behavior-based weight loss interventions in adults with obesity can lead to clinically significant improvements in weight status and reduced incidence of type 2 diabetes among adults with obesity and elevated plasma glucose levels. The USPSTF found adequate evidence to bound the harms of intensive, multicomponent behavioral interventions in adults with obesity as small to none, based on the absence of reported harms in the evidence and the noninvasive nature of the interventions.
Most of the intensive behavioral weight loss interventions considered by the USPSTF lasted for 1 to 2 years, and the majority had 12 or more sessions in the first year . Most behavioral interventions encouraged self-monitoring of weight and provided tools to support weight loss or weight loss maintenance .
Among technology-based interventions, intervention components included computer- or web-based intervention modules, web-based self-monitoring, mobile phonebased text messages, smartphone applications, social networking platforms, or DVD learning . Only 1 trial delivered its intervention through print-based tailored materials.
You May Like: Are Lidocaine Patches Covered By Medicare
Read Also: Can I Sign Up For Medicare Before I Turn 65
Reasons To Be Denied Weight Loss Surgery
Although weight loss surgery is a highly safe procedure with exceptionally good success rates, a conscientious bariatric surgeon will only accept you as a candidate if they believe that the benefits significantly outweigh the risks. The surgeons foremost priority will be your safety, and you could be denied this procedure if the surgeon is convinced that you are not eligible for it. Heres why some patients may fail to qualify for this surgery:
- Your BMI is low enough to be corrected with diet and exercise.
- You are under 18 years of age and your physiology is still developing.
- You have been diagnosed with a certain health condition that could pose threat to your safety during or after the surgery.
- You have been a regular smoker and are unwilling or unable to quit the habit for at least a few weeks before and after the surgery.
- You are taking blood thinners, NSAIDs, or other medications that increase your risk of surgery, and your physician cannot take you off them temporarily.
- You are not willing to commit to a pre- and post-operative weight loss surgery diet plan as recommended by your surgeon.
Dont Miss: Apply For Medicaid Insurance Online
Private Health Coverage For Weight Loss Surgery
Furthermore, Private Health Funds will cover the hospital fees associated with any procedure that has an Item Number, including weight loss surgery.
Private Health Funds usually offer different levels of cover depending on your monthly premium or plan.
As is common with most procedures, there is usually an out-of-pocket gap that the patient must pay as the rebates from Medicare and Private Health Funds are not sufficient to cover all the associated costs with our complete
Read Also: What Is The Cost Of Medicare B
Medicare Part A Costs
Your out-of-pocket costs under Medicare Part A may include monthly premiums, deductibles, and coinsurance. Most people get premium-free Part A, because they or their spouse paid Medicare taxes for the required 10 years to qualify. Around 1 percent, though, pay the Medicare Part A premium, which is $499 per month in 2022.
The Medicare Part A deductible is $1,566 per benefit period, which begins when you’re admitted as an inpatient and ends once you go 60 consecutive days without receiving inpatient care.
Finally, coinsurance under Part A is $0 per day for the first 60 days. After that, you’ll pay $389 per day for days 61 through 90 and $778 per day for days 91 through your 60 lifetime reserve days.