Qualified Medicare Beneficiary Program
This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
Eligibility requires:
- Income of no more than $1,094 per month for an individual in 2021, or $1,472 per month for a married couple
- Resources of no more than $7,970 for an individual in 2021, or $11,960 for a married couple
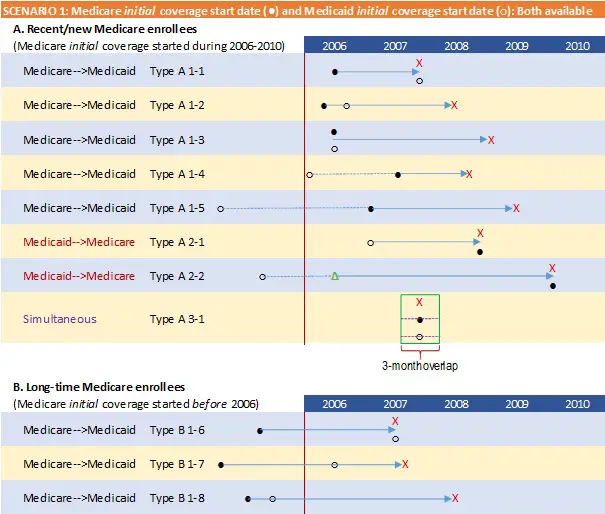
Change In Prescription Drug Coverage For Dual
With the advent of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, these dual eligibles have automatically been enrolled to a random Medicare Part D plan, effective January 1 of 2006. As a result of this auto assignment, participants who were already enrolled in a Medicare AdvantageHMO, may have been automatically disenrolled from their medical plan to allow for part D enrollment. Medicaid will still cover drugs for dual-eligible patients that are not covered by Medicare Part D, including certain controlled substances.
What Is A Dual Eligible Special Needs Plan
A Medicare Special Needs Plan is a type of Medicare Advantage plan that provides extended Medicare coverage. These private plans help coordinate care and benefits between Medicare, which is a federal program, and Medicaid, which is a state program.
D-SNPs are the most complex of the different SNPs in terms of both coverage and eligibility requirements. However, they also offer the most comprehensive benefits because those who qualify have the highest need.
You May Like: Does Aarp Cover Medicare Deductible
What Does Medicare And Medicaid Pay For
Medicaid is known as the payer of last resort. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid. For full dual eligible beneficiaries, Medicaid will cover the cost of care of services that Medicare does not cover or only partially covers . Such services may include but are not limited to:
- Nursing home care
- Dental services
- Eye examinations for prescription glasses
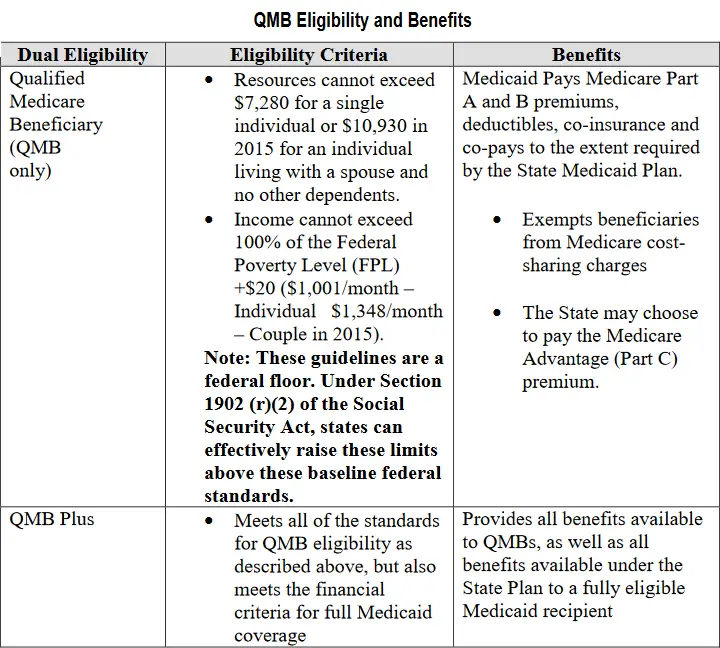
The financial assistance provided to partial dual eligible beneficiaries is outlined in the table above.
What Is Medicare Dual Eligible And How Do I Qualify
Most Americans understand that when they turn 65, Medicare will become their main health insurance plan. However, many Americans are less familiar with another health care program, Medicaid, and what it means if they are eligible for both Medicare and Medicaid. If you are dual eligible, Medicaid may pay for your Medicare out-of-pocket costs and certain medical services that arent covered by Medicare.
Read Also: Does Medicare Cover Palliative Care For Dementia
What Is A Dual
Dual-eligible beneficiaries are also eligible for a certain type of Medicare Advantage plan called a Dual-Eligible Special Needs Plan .
Medicare Advantage plans, also known as Medicare Part C, are sold by private insurers. By law, they must provide all of the same basic coverage as Medicare Part A and Part B. Medicare Advantage plans may also offer additional benefits that Original Medicare doesnt cover, such as coverage for dental, vision, hearing aids, prescription drugs and more.
A Special Needs Plan is a specific type of Medicare Advantage plan that is designed for beneficiaries who have certain health conditions or financial circumstances. A Dual-Eligible Special Needs Plan contains coverage that is tailored for someone with low income and resources. Prescription drug coverage is automatically a part of D-SNPs.
You can browse Medicare plans online and compare any Medicare-Medicaid D-SNP plans that may be available where you live.
Having Dual Eligibility For Medicaid & Medicare: Who Is Eligible And Benefits
SummaryMedicaid is a health insurance program run by each individual state for people who are low-income, and Medicare is a national health insurance program for all Americans over 65. People who are eligible for both Medicaid and Medicare are considered dual eligibles. While some benefits are available through both programs, there are also differences in coverage that make dual eligibility a good way for many seniors to pay for their care needs. Only Medicaid, for example, pays for long-term nursing home care.
Also Check: What Is Special Enrollment Period For Medicare
How Many Dual Eligibles Are There
There are 12.2 million people nationwide who are simultaneously enrolled in Medicare and Medicaid, a population often referred to as dual-eligible beneficiaries. This group represents a key opportunity for policymakers who care about government spending and improving care delivery for vulnerable populations.
What Is Pace For Medicare And Medicaid
Another Medicare and Medicaid program is PACE, or Programs of All-Inclusive Care for the Elderly.
PACE helps older Medicare beneficiaries to seek health care within their community, in their home and at PACE facilities.
Some of the things that can be covered by PACE include:
- Adult day primary care
- Caregiver training
- Transportation to a PACE facility when medically necessary
PACE is not strictly restricted to Medicare dual eligible beneficiaries. You may be eligible for PACE with only Medicare or only Medicaid .
However, you must meet all of the following conditions:
- Be at least 55 years old
- Live in the service area of a PACE organization
- Require a nursing home-level of care
- Be able to live safely in the community with help from PACE
Don’t Miss: How To Find Your Medicare Number
What Type Of Coverage Do You Get If You Are Dual Eligible For Medicare And Medicaid
There are two levels of coverage for beneficiaries who are dual eligible:
- Full dual eligibleFull dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income benefits, which provide cash assistance for basic food and housing needs. Qualifying as full dual eligible is based on your assets, which include checking and savings accounts, stocks, real estate and vehicles .
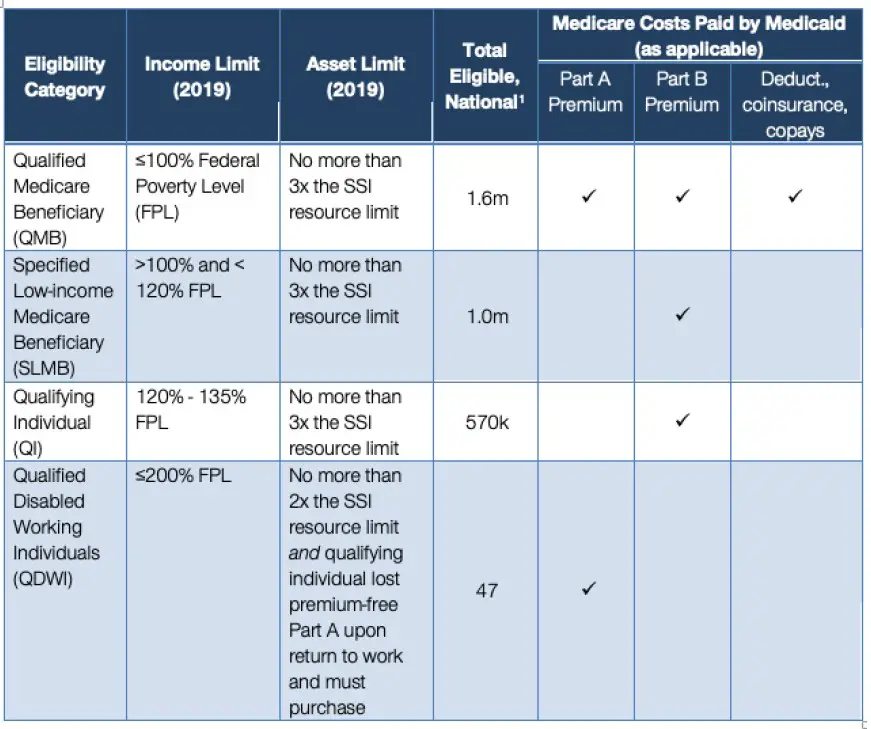
- Partial dual eligiblePartial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
A Medicare Savings Program is a federally funded program administered within each state that helps lower income people pay for Medicare premiums, deductibles, copayments and coinsurance.
The four Medicare Savings Programs are outlined below.
Explaining Medicaid Medicare & Dual Eligibility
There are two key differences between the governmental health insurance programs Medicaid and Medicare:
Medicaid is run by ones state of residence, and Medicare is run by the federal government. Medicaid is for financially needy people who have monthly income and assets below a certain amount, while Medicare is for all Americans who are 65 or more years old and/or disabled.
Some benefits overlap, while others do not. Both programs pay for medical costs including doctor appointments and hospital care, but only Medicaid will cover all the costs of living in a nursing home for more than 100 days. Medicaid is also the program for receiving long-term care services at home or in assisted living, as Medicare does not pay for long-term care .
To be dual-eligible, one must meet the income requirements of their states Medicaid program, meaning having income and assets below a certain amount, and meet the age requirement for Medicare, meaning 65 and over. Put simply, dual eligibles will be low-income and above the age of 64.
Dual eligibles receive a combination of benefits from both programs.
Medicare Benefits
Medicare is broken into types: Medicare Part A provides hospital insurance . Medicare Part B is medical insurance . Medicare Part C is also called Medicare Advantage, and it provides benefits through a private insurer . Medicare Part D covers prescription drugs.
Medicaid Benefits
Recommended Reading: What Is Statement Of Understanding Medicare
Dual Eligible Special Needs Plans
In some states, dual eligible beneficiaries may have the option of enrolling in a D-SNP, which is different from a traditional SNP or Special Needs Plan. These plans are specially designed to coordinate the care of dual eligible enrollees. Some plans may also be designed to focus on a specific chronic condition, such as chronic heart failure, diabetes, dementia, or End-Stage Renal Disease. These plans often include access to a network of providers who specialize in treating the specified condition. They may also include a prescription drug benefit that is tailored to the condition.
Understanding Medicare Dual Eligible Special Needs Plans
- A Medicare Dual Eligible Special Needs Plan is a Medicare Advantage plan designed to provide special coverage for people who are enrolled in both Medicare and Medicaid.
- These plans help people with the highest needs cover out-of-pocket costs they may otherwise be responsible for under traditional Medicare programs.
If you are age 65 and over or have certain health conditions and have limited finances to pay for your care, you may fall into a select group thats qualified for both federal and state public health insurance programs. In fact, nearly 12 million Americans are entitled to both Medicare and Medicaid coverage based on their age and health conditions. If youre one of them, you may qualify for a D-SNP.
Read on to learn what a D-SNP is and whether you may be eligible for one.
You May Like: Does Medicare Cover A1c Test
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the Member Handbook. Limitations, copays, and restrictions may apply. For more information, call UnitedHealthcare Connected Member Services or read the UnitedHealthcare Connected Member Handbook. Benefits, List of Covered Drugs, pharmacy and provider networks and/or copayments may change from time to time throughout the year and on January 1 of each year.
Recommended Reading: Does Medicare Part A Cover Dental
Who Can Apply For Dual Eligibility
To qualify for dual eligibility, you need to meet the enrollment criteria for both the Medicare and Medicaid program.
To get Medicare coverage, you will need to be either:
-
65, or turning 65 in the next three months.
-
Suffer from ESRD .
To get Medicaid coverage, you will need to:
-
Be a citizen or lawful permanent resident of the U.S.
-
Be a resident of the state in which you are receiving Medicaid coverage.
-
Pass a state-specific income and asset eligibility test to determine if you qualify.
Specific individuals are exempt from the income eligibility requirement. You can learn more about this by visiting the Medicaid.gov website.
If you meet both the Medicare and Medicaid enrollment criteria you will become dual eligible, and Medicaid will assist in covering the cost of your Medicare coverage.
Income and asset requirements are different for each state. Here are three examples to show you what these are in 2022 for different parts of the U.S.
Financial Criteria To Qualify For Slmb Status
| Maximum Monthly Income |
|---|
| At least 100% but less than120% | Equals FMAP |
What is a Specified Low-Income Medicare Beneficiary Status?
SLMB individuals exceed the usual financial criteria for full Medicaid coverage. However, they are still eligible to receive partial Medicaid assistance for Medicare costs and Medicaid health care.
What does SLMB status cover?
SLMB status will mean that Medicaid will pay for your Part B premiums only. You will not be covered for Part A premiums or other Medicare-related costs such as deductibles, coinsurance or Part B premiums.
Don’t Miss: Does Medicare Cover Home Sleep Apnea Test
Types Of Medicaid Coverage
Mandatory Medicaid benefits are mandated by the federal government. They include inpatient hospital services, laboratory services, outpatient services, and physician services.
Optional Medicaid coverage is state-specific and can include medical insurance for prescription drug coverage, dental services, occupational therapy, and hospice care.
Can A Medicare Advantage Plan Be Secondary
Medicare Supplement plans are secondary payers to Medicare. … Since Medicare doesn’t cover 100% of your medical services, looking into a form of secondary coverage, such as Medigap or Medicare Advantage, to help cover out-of-pocket costs you are left responsible to pay will reduce your financial obligation.
Read Also: Are Chiropractors Covered Under Medicare
Who Is Dual Eligible For Medicare And Medicaid
To be Medicare dual eligible, you have to meet the requirements for Medicare and your states Medicaid program.
To be eligible for Medicare, you must:
- Be at least 65 years old or having a qualifying disability
- Be a U.S. citizen or permanent legal resident
- Be eligible for benefits through Social Security or the Railroad Retirement Board
Generally speaking, Medicaid provides health insurance to low-income individuals and families, children and pregnant women. The best way to find out if you are eligible for Medicaid is to visit your states Medicaid website.
If you’re eligible for Medicaid and want to find out if you’re also eligible for a dual-eligible Medicare Medicaid plan, you can all to speak with a licensed insurance to find out if you’re eligible. An agent can help you compare the plans that are available where you live and find out what they may cover, which could include benefits like prescription drugs and other services.
Find $0 premium Medicare plans in your area
Or call 1-800-557-6059TTY Users: 711 24/7 to speak with a licensed insurance agent.
Dual Eligible And Medicare Advantage
Certain dual eligibles are still allowed to enroll in Medicare Advantage plans. These are called Special Needs Plans and are designed to cater to dual eligibles and other specific groups.
You can learn more about Medicare Advantage by reading our guide, What is Medicare Part C?.
If you have questions about finding or enrolling in a dual-eligible Medicare Advantage plan, reach out to PolicyScout via .
Don’t Miss: Where Do I Sign Up For Medicare Part D
What Is Medicare Vs Medicaid
Medicare
An animated white speech bubble appears over an animated character’s yellow and blue head.
ON SCREEN TEXT: Medicaid 101
The speech bubble and character fall away. Blue text appears on a light blue background. White text appears in two animated circles below. The blue and green circles overlap.
ON SCREEN TEXT: Medicaid is a joint federal and state health program. Federal State
The text and circles fall away. Blue text appears surrounded by blue animated disks with dollar signs on them. Animated individual and family character graphics appear below the text.
ON SCREEN TEXT: It is for individuals, families and children with limited income & resources.
The text and graphics fall away. A white map of the continental U.S. appears on a light blue background. Green map marker icons dot the map. Blue text appears in the center of the map.
ON SCREEN TEXT: Each state creates its own Medicaid programs based on federal guidelines.
The map disappears. Blue text appears surrounded by animated green and white form and plus sign graphics.
ON SCREEN TEXT: Medicaid programs have mandatory benefits & optional benefits.
The text and graphics fall away. Blue text appears over an animated dark blue scale graphic. Yellow animated coins pile up on the left side of the scale and animated books pile up on the right side.
ON SCREEN TEXT: Medicaid costs will vary based on a person’s income and the state’s Medicaid rules.
ON SCREEN TEXT: Eligibility varies based on a state’s Medicaid rules.
Historical Challenges With The Dually
Historically, one of the major challenges for the dually-eligible has been care coordination between Medicare and Medicaid. These two systems of care do not “talk to each other” systematically, so one physician that bills primarily through Medicare may not be familiar with benefits that are available through Medicaid. Additionally, since Medicaid benefits vary by state, it is difficult for care providers and consumers to understand the complexity that is inherent within the Medicaid system.
Because duals tend to be the most vulnerable, and often sickest, adults, their care has historically been expensive, totaling $319.5 billion in 2011. One proposed reason for this significant cost would be that many Medicaid programs, prior to the 2010 passage of the Affordable Care Act used a fee-for-service model. Fee-for-service models are typically more costly because they allow providers to charge for the quantity of care they provide, rather than the quality.
In order to resolve these pain points, the ACA includes provisions that specifically address the coverage and care of duals. On a federal level, the Centers for Medicare and Medicaid Services has established two new offices: The Federal Coordinated Health Care Office as well as the Center for Medicare and Medicaid Innovation in order to both strategize and monitor the type and quality of care afforded to duals. These offices focus on both monetary expenses as well as care innovation and quality for dual eligible beneficiaries.
Also Check: Does Medicare Cover Hearing Test For Tinnitus