How Is Osa Diagnosed
A normal breathing problem that causes mild symptoms can go undiagnosed for years. Although some people may believe they have sleep apnea, a thorough diagnosis is required in order to receive coverage for any treatments. Patients must participate in a sleep study in order to be diagnosed. The patient spends the night at a sleep laboratory for monitoring during the sleep study. Blood oxygen levels, breathing rate, brain-wave activity, leg movements, and how many partial inhalations are taken each hour are all examined.
If a patients sleep study shows that he or she has sleep apnea, a doctor will either recommend using a CPAP machine or an oral apparatus to help them get some rest. Because a CPAP machine requires users to wear a mask while sleeping and requires them to plug the equipment into an outlet all night, not everyone is successful with it. Thats why people resort to mouthpieces instead. Mouthpieces are intended to provide a similar therapy as a CPAP machine, with the exception of the mask and requirement for an outlet.
Patients wear these custom-made mouthpieces while sleeping. Mouthpieces are used to help the lower jaw move forward and relax the tissues at the back of the throat. This ensures that the base of the tongue does not collapse, preventing airway obstruction. Patients who have mild to severe instances of sleep apnea benefit from mouthpieces.
Book Your Bulk Billed Sleep Study Today
To book a sleep study, email us at , call us on the number below, or use the enquiries box.
NSW: 9798 2322
Locations: Ashfield, Auburn, Bankstown, Baulkham Hills, Bonny Hills, Brookvale, Burwood, Camden, Campbelltown, Chatswood, Fairfield, Hurstville, Liverpool, Moorebank, Macquarie Park, Maroubra, Miranda, Mosman, Parramatta, Penrith, Rozelle, Toronto, Warrawong, Woolloomooloo.
VIC: 9017 3631
Locations: Belmont, Berwick, Boxhill, Croydon, Frankston, Wheelers Hill, Geelong West.
QLD
Coomera – Contact Jack on 5580 0429Gympie – Contact Tracey, Merry, or Indoorooopilly – Contact Paul, Jenna, or Vy on 3878 3635
Get Enrolled In Medicare That Will Help You Pay For A Cpap Machine
From does Medicare cover CPAP machines? to does Medicare pay for walk-in tubs?, we can answer all of your Medicare questions.
We can also help you get some of the costs covered from a Medicare plan thats right for you. Talk with a local Medicare specialist that can help you find the right plan to cover your sleep study, CPAP machine, replacement parts, and more. Costs may vary and plans can even vary state to state.
Learn more about your Medicare options from a local Medicare pro today! Click the button below to get a free Medicare quote.
You May Like: Sleep Number Bed Billings Mt
Read Also: Must I Enroll In Medicare At Age 65
How Much Does A Cpap Machine Cost With Medicare
You will pay a 20 percent coinsurance based on the Medicare-approved amount for a CPAP machine. Medicare Part B covers the other 80 percent of the cost. The Part B deductible applies.
Medicare helps pay to rent your CPAP machine for a total of 13 months, but only if you continue to use it without interruption. After 13 months of rental, you own the CPAP machine.
If you have a Medicare supplement plan , the plan may cover your CPAP coinsurance payment for the rental period. If you have a Medicare Advantage plan , you need to check with the plan for details about what a CPAP machine would cost. Medicare Advantage plans must provide at least the same coverage as Part B, but each plan sets its own cost terms.
Read Also: Does Medicare Cover Lasik Eye Surgery
Genioplasty And Genial Tubercle Advancement
Song and associates performed a systematic review and meta-analysis for studies evaluating genioplasty alone, genial tubercle advancement alone, and GTA with hyoid surgery for the treatment of OSA. Three authors searched through November 15, 2015 10 databases were used. A total of 1,207 studies were screened 69 were down-loaded and 13 studies met inclusion criteria. A total of 111 patients were included, with 27 standard genioplasty, 10 modified genioplasty, 24 GTA, and 50 GTA-HS patients. For standard genioplasty, the AHI reduced from a mean ± standard deviation of 18.8 ± 3.8 to 10.8 ± 4.0 events/hour , p = 0.0001. Genioplasty improved lowest oxygen saturation from 82.3 ± 7.3 % to 86.8 ± 5.2 % , p = 0.0032. For modified genioplasty AHI increased by 37.3 %. For GTA, the AHI reduced from an M ± SD of 37.6 ± 24.2 to 20.4 ± 15.1 events/hour , p = 0.0049. Genial tubercle advancement improved LSAT from 83.1 ± 8.3 % to 85.5 ± 6.8 % , p = 0.2789. For GTA-HS, the AHI reduced from an M ± SD of 34.5 ± 22.1 to 15.3 ± 17.6 events/hour , p < 0.0001 GTA-HS improved LSAT from 80.1 ± 16.6 % to 88.3 ± 6.9 % , p = 0.0017. The authors concluded that standard genioplasty, GTA and GTA-HS can improve OSA outcomes such as AHI and LSAT. Moreover, they stated that given the low number of studies, these procedures remain as an area for additional OSA research.
You May Like: How Do I Join Medicare
Ama Disclaimer Of Warranties And Liabilities
CPT is provided âas isâ without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Read Also: A Good Night Sleep Store Fayetteville Nc
Medicare Guidelines For Cpap
Read Also: Issues With Sleep Number Beds
You May Like: What Is The Difference Medicare Part A And B
Does Medicaid Cover Cpap
Many sleep study diagnoses are treated using therapies such as CPAP, particularly for beneficiaries experiencing severe and unambiguous obstructive sleep apnea. The use of CPAP is covered under Medicaid when prescribed by the attending licensed technician.
However, if the beneficiary has been utilizing CPAP therapy under a different insurance plan and is looking to switch to Medicaid, the issue requiring CPAP may be considered a preexisting condition. In this case, the beneficiary must first be found in accordance with all applicable policy guidelines. This typically includes an initial doctors visit, even in the event that you are currently using CPAP therapy or have in the past.
To find out more about how much your sleep study may cost you, talk to your doctor or health care provider.
Does Medicare Cover Sleep Studies
by Christian Worstell | Published January 19, 2022 | Reviewed by John Krahnert
Medicare typically does cover sleep studies to determine whether or not you suffer from sleep apnea.
A Medicare Supplement plan can help pay for your sleep study Medicare costs, such as Medicare deductibles, copays, coinsurance and more.
Read Also: Is Genetic Counseling Covered By Medicare
Does Medicare Cover Sleep Apnea
Sleep apnea can be a serious health problem. It occurs when your normal breathing is interrupted during sleep. Medicare does help cover some sleep apnea tests and treatment.
Those who go untreated may wake up dozens or even hundreds of times throughout the night. Because of this, the brain, and often the rest of the body, does not get enough oxygen.
The effects of the disorder can be major. Sleep apnea can result in:
-
Higher blood pressure
-
Worsening performance of everyday activities
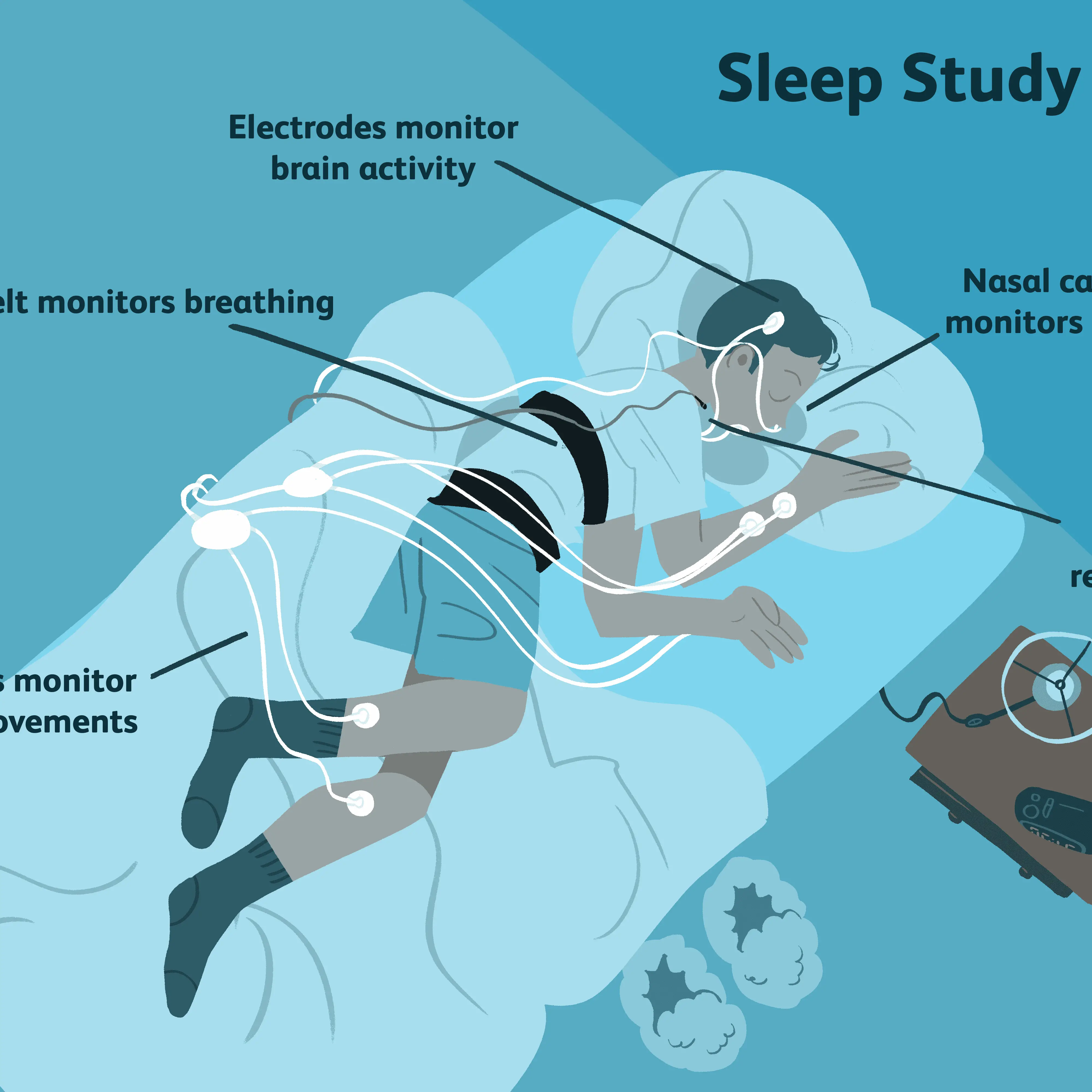
If your doctor suspects you have sleep apnea, he or she may order that you undergo a polysomnography test.
-
During the test, you will be hooked up to equipment such as electrodes, which will be attached to your face and scalp. These record signals generated by your brain and muscles while you sleep.
-
Youll be fitted with a belt around your chest and abdomen, in order to measure your breathing.
-
Youll also receive a probe on your finger, which will measure oxygen in your blood.
Whether your sleep study uses these or other equipment, a sleep specialist will review the results of your exam, and determine whether or not you have sleep apnea.
Are There Alternative Treatments For Sleep Apnea Besides Cpap Machines Covered By Medicare
If you have sleep apnea, there are a number of different treatment options available to you.
The most common treatment is a breathing device called a CPAP machine, but there are also other options such as oral appliance therapy, nerve stimulation, positional therapy, and weight loss.
Each of these has its own pros and cons, so its important to talk to your doctor about which one might be right for you.
Depending on the treatment plan you may have to pay your Medicare Part B deductible if you have Original Medicare along with 20% coinsurance.
You May Like: What Is The Best Medicare Insurance Company
Search For A Medicare Policy
Go to the CMS Centers for Medicare & Medicaid Services website to search the Medicare Coverage Database. The Medicare Coverage Database includes documents such as articles and policies related to all Medicare programs including but not limited to Part B coverage and DME. Use the advanced search feature to perform a search. Several frequently accessed sleep related policies can be found here.
Why Pay For Sleep Studies And Cpaps

For Americans on Medicare, the benefits of CPAP therapy often outweigh the costs of your deductible plus 20% copayment for sleep studies, CPAP equipment, and CPAP replacement parts. As you use your CPAP, youll have a wide range of long-term benefits such as:
- Reduced risk of heart problems like congestive heart failure and coronary artery disease
- Reduced risk of stroke
- Reduced risk for Type 2 Diabetes
- Reduced risk of causing motor vehicle accidents
Youre also likely to experience the following physical benefits:
- Increased daytime alertness
- Reduced or eliminated snoring
Additionally, untreated, severe sleep apnea can cause serious damage to brain tissue over time. For those undergoing CPAP therapy, they will begin to develop a more regular sleeping pattern and ensure that the amount they sleep is quality sleep thereby repairing the damage done to your brain. You shouldnt rule out being able to experience improvements to your well-being in these ways:
- Increased concentration
- Increased emotional stability
- Improved memory
- Better relationships with your partner through improved mood reduction in irritability reduction in depressive symptoms and finally letting your partner get their own quality sleep without being disturbed by snoring.
Read Also: How To Order A Medicare Card
Does Medicare Cover In
Yes.
In 2008, the Centers for Medicare and Medicaid Services updated the National Coverage Determination for CPAP to include home sleep apnea testing as a means to qualify patients with obstructive sleep apnea for CPAP therapy .
HST is a type of diagnostic polysomnography which is self-administered by the patient in his/her home. It is used to diagnose sleep apnea by recording several channels of information: respiratory effort, pulse, oxygen saturation, nasal flow and snoring. HST is a cost-effective alternative to in-center sleep testing for many patients if it is highly likely that the patient has moderate to severe sleep apnea, and if the patient has no other significant medical issues such as pulmonary diseases, neuromuscular disease or congestive heart failure. HST cannot be performed on children and cannot diagnose other sleep disorders such as restless leg syndrome, periodic limb movement disorder or narcolepsy. These patients should be tested in a sleep center .
You can read the American Academy of Sleep Medicine clinical guidelines for home sleep testing here.
Does Medicare Cover A Sleep Study
Do you need to get a sleep study?
In other articles weve written about Medicare coverage of CPAP machines and other sleep apnea treatments. In many cases, before you get one of those treatments, you need to get a sleep study.
Sleep studies are helpful in diagnosing someone with a sleep disorder. And, once you have a diagnosis, you can get a treatment plan to help you get a better nights sleep.
There are actually four types of sleep studies. We will cover them later in this article.
But whatever type you need, a common question many people have is, Does Medicare cover a Sleep Study? In this article, we answer the question in clear, plain English. You will also find the average costs of a sleep study, as well as other helpful info.
Read Also: What Is The Medicare Discount Card
Compliance Monitor For Oral Appliances
The American Academy of Sleep Medicine and the AADSMs clinical practice guideline on The treatment of obstructive sleep apnea and snoring with oral appliance therapy stated that There are several recent non-RCTs published that report on the use of objective adherence monitors in OAs. Further RCTs are needed to evaluate the efficacy of these monitors and also to compare it with the CPAP objective adherence rate.
Furthermore,, an UpToDate reviews on Oral appliances in the treatment of obstructive sleep apnea in adults does not mention the use of compliance monitors.
Is A Sleep Study Worth It
Sleep disorders can lead to health challenges. If you are facing irregular sleep patterns, its important to consult with a doctor regarding next steps.
The CDC has conducted an extensive review of clinical studies on the effectiveness of sleep studies. There is no gold standard like there is for cancer which uses tissue biopsies and other diseases.
But the research shows that sleep studies generally provide an effective diagnosis. According to the CDC, sleep studies will identify a significant proportion of patients with OSA who will respond clinically to CPAP and will exclude a significant proportion of those who will not.
Because of this assessment, Medicare agreed to provide coverage for sleep studies. This has also been the case with various Medicaid programs.
Recommended Reading: What Is Medicare Part B Monthly Premium
Is Sleep Test Covered By Medicare
No. The fee for a Home Sleep Study is $400. This is partially covered by Medicare . In order to receive a rebate you must have a valid Medicare card and a current GP or specialist referral.
How often can you have a sleep study with Medicare?
How Often Does Medicare Pay for a Sleep Study? Testing frequency depends significantly on the reasons behind needing a new study. There isnt a lifetime limit on sleep studies. You may need a new study if you discontinue CPAP therapy or fail during the three-month trial period, which is when testing and trials restart.
What diagnosis will cover a sleep study?
Polysomnography is covered only if the beneficiary has the symptoms or complaints of narcolepsy, sleep apnea, impotence, or parasomnia which must be documented in the medical record. Polysomnography for chronic insomnia isnt covered.
Does Medicare Cover Cpap Supplies
In addition to CPAP machines, Medicare Part Bs durable medical equipment benefit also covers CPAP supplies, such as face masks, tubing and filters. Medicare Part B pays 80 percent of the Medicare-approved amount, while you pay 20 percent as coinsurance. Your coinsurance may be paid by your Medicare supplement plan, or your cost may be different if you have a Medicare Advantage plan.
Since CPAP supplies can get dirty and lose effectiveness with use, Medicare covers replacement supplies on a regular schedule. Depending on the item, you may need replacements every two weeks to every six months. Talk with your doctor or supplier about scheduling replacement supplies.
Also Check: Why Do I Sometimes Pee In My Sleep
Read Also: Why Is My First Medicare Bill For 5 Months
When Does Medicare Pay For A Sleep Study
Sleep studies are covered by Medicare Part B health care coverage. And because Medicare Advantage insurance plans are required by law to provide all of the same coverage as Part A and Part B, sleep studies are covered by these private Medicare plans as well.
In order to qualify for Medicare coverage, your doctor must confirm that you display clinical signs and symptoms of obstructive sleep apnea. The sleep study must be deemed medically necessary and requested by a Medicare-approved doctor.
All four levels of sleep studies are covered by Medicare. But a Type I study, which requires you to sleep overnight in a sleep lab facility under the supervision of a sleep specialist, must be specifically ordered by a doctor before Medicare will cover it.
Medicare may also pay for medically necessary sleep studies to test for:
- Periodic limb movement disorder
- REM sleep behavior disorder.
A Medigap Plan Can Help Pay For Sleep Apnea Medicare Costs

The cost of sleep apnea testing and treatment can be lowered even more with the help of a Medicare Supplement Insurance plan.
There are eight standardized Medigap plans that fully cover the cost of the 20% Part B coinsurance payment required for covered sleep apnea testing and CPAP machine treatment.
A licensed agent can help you decide on a Medicare option that works for you. Call today to speak with a licensed agent and compare the Medigap plans that are available where you live.
Recommended Reading: Does Medicare Cover Inogen One G4
