Within 3 Months Of Medicare Enrollment
If a person enrolls in Medicare Advantage when they first become eligible for Medicare, they can switch to original Medicare and Medigap within the first 3 months of their plan.
This benefit is available to protect people who find that the policy they first chose does not work well for their healthcare needs. A person would still be within the Medigap enrollment window, and an insurance company cannot deny an individual a Medigap policy during this time.
Understanding The Waiting Period For A Pre
Federal law doesnt require insurers to cover pre-existing conditions for the first six months. The six-month waiting period is also known as the look-back period, meaning insurers can delay coverage for health conditions that you sought treatment for before applying. During this waiting period, Part A and Part B continue to provide coverage for pre-existing conditions.
Once the waiting period ends, the Medigap policy covers costs like deductibles and copays. Its important to understand what the waiting period might mean for your health care needs.
You May Like: How Many Parts Medicare Has
How Can I Switch From Medicare Advantage To Traditional Medicare Is There A Form I Need To Fill Out
If youre already in a Medicare Advantage plan and you want to switch to traditional Medicare, you should contact your current plan to cancel your enrollment and call 1-800-MEDICARE . Note there are specific enrollment periods each year to do this. The first period when you can switch from your Medicare Advantage plan to traditional Medicare is during the Medicare Open Enrollment period that runs October 15 to December 7. When you make the switch back to traditional Medicare during the Medicare Open Enrollment period, the change will take effect on January 1 of the following year. The second period you can switch from Medicare Advantage to traditional Medicare is during the Medicare Advantage Open Enrollment Period that runs from January 1 to March 31. If you switch to traditional Medicare and you want prescription drug coverage through Medicare, you will also need to sign up for a stand-alone prescription drug plan for your drug coverage.
Read Also: Who To Talk To About Medicare
You May Like: Is Medicare Free For Disabled
Switching Back To Original Medicare
While you can save money with a Medicare Advantage Plan when you are healthy, if you get sick in the middle of the year, you are stuck with whatever costs you incur. If you decide that the Medicare Advantage Plan isn’t for you, you have the right under federal law to purchase any Medigap plan if you switch to Original Medicare within 12 months of the date that you joined a Medicare Advantage Plan for the first time.
You may also switch from your Medicare Advantage Plan to Original Medicare during the annual Open Enrollment Period or if you qualify for a Special Enrollment Period. However, you may not be able to purchase a Medigap policy . If you are able to do so, it may cost more than it would have when you first enrolled in Medicare.
Keep in mind that an employer only needs to provide Medigap insurance if you meet specific requirements regarding underwriting . The wait time for Medigap coverage can be avoided if you have what is called a “guaranteed issue right.”
A thorough breakdown of what is considered a “guaranteed issue right,” where an insurance company can’t refuse to sell you a Medigap policy, can be found on the Medicare website.
Most Medigap policies are issue-age rated policies or attained-age rated policies. This means that when you sign up later in life, you will pay more per month than if you had started with the Medigap policy at age 65. You may be able to find a policy that has no age rating, but those are rare.
What Is A Medicare Supplement Plan

Medicare supplement plans are one health insurance option for people with Original Medicare. There are standardized Medicare supplement insurance plans available that are designed to fill the gaps left by Original Medicare . These are sold by private insurance companies as individual insurance policies and are regulated by the Department of Insurance. After age 65 and for the first six months of eligibility for Medicare Part B, beneficiaries have an Open Enrollment Period and are guaranteed the ability to buy any of these plans from any company that sells them. Companies cannot deny coverage or charge more for current or past health problems. If you fail to apply for a Medicare supplement within your Open Enrollment Period, you may lose the right to purchase a Medicare supplement policy without regard to your health.
Recommended Reading: Does Medicare Cover In Home Caregivers
During The Oep For Drug Coverage
Two OEPs apply to Medicare Advantage plans. These are also the times at which a person can drop their Medicare Advantage plan and return to original Medicare.
The first enrollment period runs from each year. This is the OEP for all Medicare plans, including Medicare Advantage and Medicare prescription drug coverage.
During this time, a person can return to original Medicare. However, if they had prescription drug coverage through Medicare Advantage, they will need to enroll in Medicare Part B to maintain their prescription drug coverage.
Think Carefully When Choosing Your Medicare Coverage
Think carefully about your options and which coverage is right for your health and lifestyle. Your next opportunity to change your Medicare coverage wont be until the next years Annual Enrollment Period, unless you experience a qualifying life event and become eligible for a Special Enrollment Period.
Recommended Reading: Is There A Copay With Medicare Part D
When Can I Change Medicare Plans
If you’ve evaluated your current Medicare plan and have decided that a different option may make more sense for you, you are free to change plans during the Medicare Annual Enrollment Period , which runs from each year.
This includes switching from Medicare Advantage to Original Medicare . You may also switch Medicare Advantage plans or Prescription Drug Plans during this time.
You may also switch from Medicare Advantage to Original Medicare during the Medicare Advantage Open Enrollment Period, which runs from January 1st to March 31st each year.
You can compare Part D plans available where you live and enroll in a Medicare prescription drug plan online when you visit MyRxPlans.com.
So Should I Consider Changing From Medigap To Medicare Advantage
This is a personal decision. Medicare Advantage plans and their limitations are perfectly acceptable to many people. We have hundreds of clients happily insured with these plans.
We have found, though, that for people who have grown accustomed to the flexibility of a Medicare Supplement, the transition can be bumpy. Its much easier if you get educated on how the new coverage will operate differently than what you are used to.
Do your homework before changing from Medigap to Medicare Advantage. Get the facts. Though this new kind of coverage may mean some homework on your end, it can also save on monthly premiums. Only you know which type of coverage is best for you.
Want a personal consultation about whether changing from Medigap to a Medicare Advantage plan is right for you? Call Boomer Benefits at 855-732-9055, well walk you through it so you can decide whats right for you.
Editors Note: This post was originally published in 2016. It has been updated in 2021.
Don’t Miss: What’s Part B Medicare
The First Year Exception
There is a 12 month exception on underwriting if the Medicare Advantage plan you are in is the first one you have ever tried. If you leave that Medicare Advantage plan in the first 12 months, you can return to your Medigap plan without underwriting. In that first year ONLY, you will be guaranteed to reinstate your former Medigap plan.
Be aware of this window if you try Medicare Advantage and decide you dont like it.
Moral of the story: It has been my experience that people like their Medicare Advantage plan until they get sick. Once they develop a chronic or serious health condition, they often desperately want to go back to their Medigap plan for the fuller coverage.
However, because of that health condition, you may not be able to get back into a Medigap plan. Ask yourself if that is a risk you are willing to take in order to lower your health insurance costs now. The old motto that you get what you pay for definitely applies here.
Also Check: What Is The Monthly Premium For Medicare Plan G
How Can I Switch Do A Different Medigap Policy
Changing Medigap plans can be simple with the help of a licensed insurance agent.
- You can visit MedicareSupplement.com and request to speak to a licensed agent. If you know which Medigap plan you want, the agent can guide you through the application process. If you are unsure about which Medigap plan you want, an agent can help you review the available options in your area.
- If youre accepted into a new Medigap plan and wish to keep it , contact the company who issued your original Medigap plan and cancel it in writing. Your insurance company cannot cancel the plan for you. Again, a licensed insurance agent can help you with this.
Remember that if you move to another state, you are allowed to keep your existing Medigap policy, even if that plan is not sold in your new state. However, your new state may offer a different selection of Medigap plans with costs that may be more beneficial to you.
If you move, contact a licensed insurance agent to learn about the plan options available in your new location.
Read Also: Does Medicare Pay For Entresto
Can I Switch From Medigap To Medicare Advantage
Switching from Medigap to Medicare Advantage may save you money in monthly costs since Medigap plans tend to have higher premiums than Medicare Advantage plans. However, Medicare Advantage plans often cover fewer expenses than Medigap potentially resulting in more out-of-pocket expenses.
Medigap plans work with your Original Medicare to help pay for most or all of your out-of-pocket costs, such as copayments, coinsurance and deductibles that Original Medicare doesnt cover. This plan gives you more flexibility when it comes to doctor choice as well because you can go to anyone who accepts Medicare.
Advantage plans tend to be a great option for Medicare-eligible individuals who are looking to save money each month, but tend to have lower coverage needs. Typically, with any health insurance plan, the lower the premium, the higher the deductible. Since an Advantage plan would entail a $0 premium, you could be paying more, especially factoring in aspects like prescription costs.
Can You Enroll In Medigap
If youre switching from Medicare Advantage to Original Medicare, you can also purchase a plan Medicare Supplement plan. This kind of plan, also known as a Medigap policy, pays for gaps in Medicares coverage.
For instance, Medicare Part B pays 80% of covered costs after you pay your annual deductible. A Medigap policy would pay the remaining 20% due. But if youve missed your Medigap Open Enrollment Period, an insurer could deny you coverage due to your health history.
You May Like: Is Medicare Considered A Group Health Plan
Can I Change My Medicare Supplement Insurance Each Year
You can change Medicare Supplement insurance at any time. Unlike Medicare Advantage plans, Medigap doesnt have an Annual Enrollment Period.
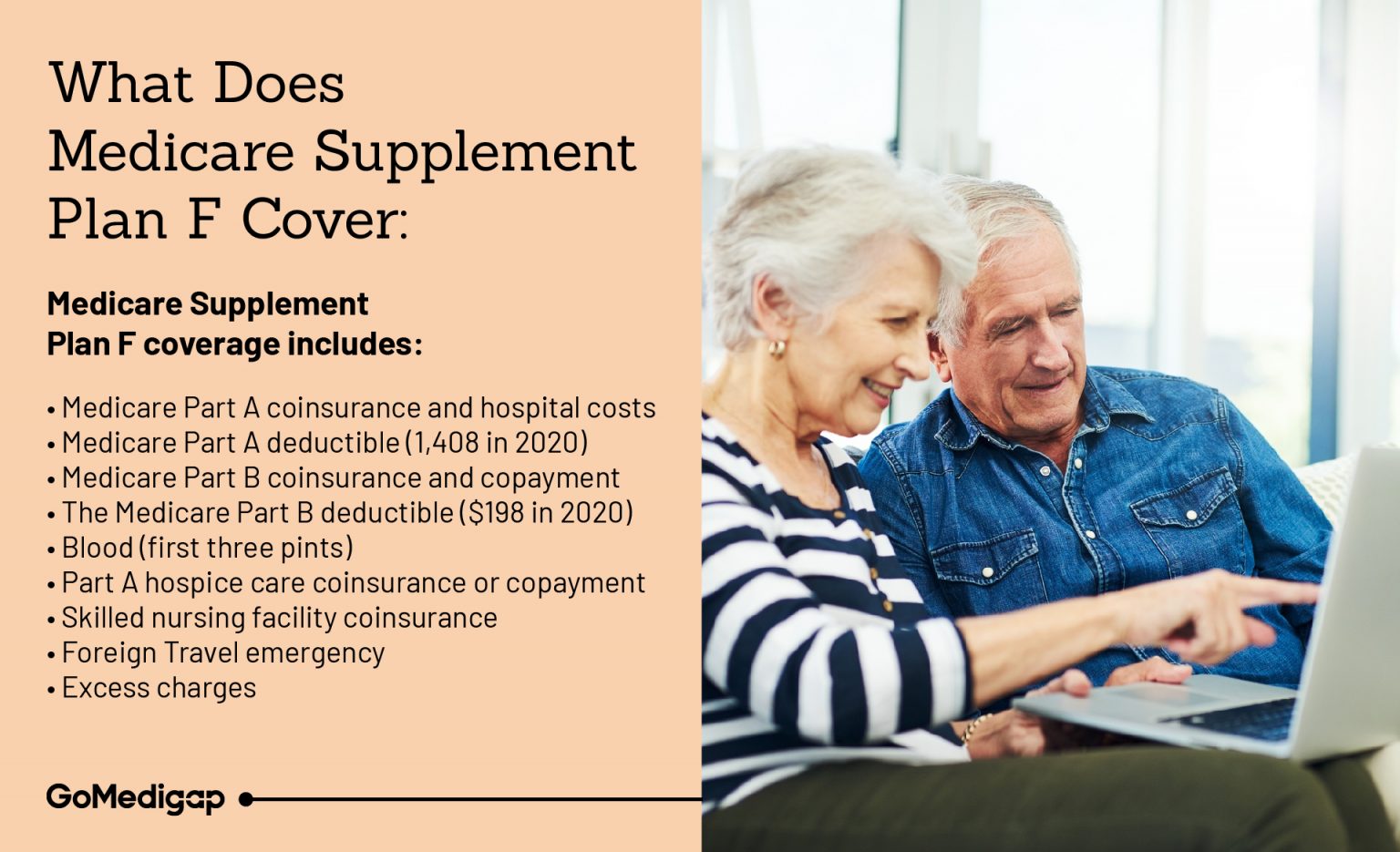
If you have a Plan F and feel like its too much insurance, a Plan G or a Plan N could prove beneficial for you, especially if you dont mind paying the Part B deductible.
On the other hand, you may consider a high deductible option to lower your monthly premiums. The general rule of thumb is the higher your copayments and coinsurances, the lower your premiums.
So, a good question to ask yourself is, would I rather pay now or later? Also, its important to understand that paying later could mean paying more too.
What Is The Medicare Supplement Free Look Period
Medigap plans come with a 30-day free look period. You can keep your old plan for 30 days after your new one starts. If you decide you liked the old one better, you can switch back and cancel the new one.
To take advantage of this, you will have to pay premiums for both plans for one month. But, if you change your mind after the free look period, you will have to reapply and meet medical underwriting guidelines.
Its important to note, beneficiaries who had an older Medigap plan that is no longer offered wont be able to go back to their old plan. If you never leave your older Medigap plan, you are automatically grandfathered in, once you change there may be no going back.
Get A Free Quote
Find the most affordable Medicare Plan in your area
Also Check: Does Medicare Cover Handicap Ramps
Can You Switch From Advantage Plan To Medigap
A person can switch from Medicare Advantage to Medicare with a Medigap policy. … Medigap plans, or Medicare supplement plans, are available to help people fund these extra costs. People can enroll in them alongside traditional Medicare. However, a person cannot enroll in both Medicare Advantage and Medigap.
Can You Switch Yes But Theres A Catch
Its logical to consider enjoying the cost savings of a Medicare Advantage plan while youre relatively healthy, and then switching back to regular Medicare if you develop a condition you want to be treated at an out-of-town facility. In fact, switching between the two forms of Medicare is an option for everyone during the open enrollment period. This Annual Election Period runs from October 15 to December 7 each year.
Heres the catch. If you switch back to regular Medicare , you may not be able to sign up for a Medigap insurance policy. When you first sign up for Medicare Part A and Part B, Medigap insurance companies are generally obligated to sell you a policy, regardless of your medical condition. But in subsequent years they may have the right to charge you extra due to your age and preexisting conditions, or not to sell you a policy at all if you have serious medical problems.
Some states have enacted laws to address this. In New York and Connecticut, for example, Medigap insurance plans are guaranteed-issue year-round, while California, Massachusetts, Maine, Missouri, and Oregon have all set aside annual periods in which switching is allowed. If you live in a state that doesn’t have this protection, planning to switch between the systems depending on your health condition is a risky business.
You May Like: Where To Send Medicare Payments
When Can You Change Medicare Supplement Plan
You can change your Medicare Supplement, or Medigap, plan anytime you choose. When you first enroll, youll have a six-month timeframe to select any supplement plans with Guaranteed Issue rights.
After this open window, youll have to apply through the carriers application process. However, some states, such as California, Oregon, Missouri and Washington, enable you to change supplement plans without fulfilling these requirements.
Enrollment Periods For Medicare Supplements
Just like Medicare has special enrollment periods throughout the year, Medicare Supplements have a special window where you need to purchase a plan.There is really only one Enrollment period for Medicare Supplements. It is referred to as the Initial Enrollment Period. This window is from 3 months prior to your 65th birthday and 3 months after.
During this period you can enroll in a Medicare Supplement without being subject to medical underwriting and policies are guaranteed issues
Dont Miss: Does Medicare Cover While Traveling Abroad
Recommended Reading: How Do I Call Medicare
Set Your Calendar For September
We recommend that people on Medicare Advantage plans set a calendar reminder to review the benefits annually in September. When your Annual Notice of Change packet from the carrier arrives, get started.
In a nutshell: Medicare Advantage plans require a bit of attention from you each year to ensure you are still enrolled in the best coverage for you. Plan ahead to review the plans coverage notice in September for the coming year.
Medicare Annual Enrollment Period

You can join, switch or drop a Medicare Advantage or Medicare prescription drug plan during the Medicare Annual Enrollment Period . AEP is October 15 to December 7. Since its the same time every year, you always know exactly how many shopping days you have until you can add or switch coverage during AEP.
Read Also: Does Medicare Cover Dental Root Canals
Can You Switch From Medicare Supplement To Advantage
Asked by: Lemuel McClure
Can you switch from Medicare Supplement to Medicare Advantage? Yes. … 7, you can make the switch to Medicare Advantage. Medicare Supplement Insurance plans cover some or all of your out-of-pocket expenses from Original Medicare, such as copayments, coinsurance and deductibles.
Can I Switch From An Advantage Plan To A Supplement
To switch from Medicare Advantage is a multi-step process. … Then, you can apply for a Medicare Supplement insurance plan. In most cases, you can only leave a Medicare Advantage plan during certain times of the year, such as: The Medicare Advantage Open Enrollment Period between January 1 and March 31.
Recommended Reading: Do Medicare Premiums Increase With Income
Additional Special Enrollment Periods
Some Medicare special enrollment periods apply on a one-time basis and are triggered by specific events, while others apply year-round for specific populations. Some apply to Medigap, while others apply to Medicare Advantage and Part D Prescription Drug Plans.
For Medicare beneficiaries who qualify for a Low-Income Subsidy , and for those who are in a nursing home or other institutional facility, enrollment in Medicare Advantage plans and Part D prescription drug coverage is not limited to the annual open enrollment period. Enrollees who qualify for Extra Help can make changes to their Medicare Advantage or Part D coverage up to once per calendar quarter. And enrollees who are institutionalized can make changes to their Medicare Advantage or Part coverage year-round, with coverage effective the first of the month following their enrollment.
. Visit this page to review our guides to Medicaid benefits available to Medicare enrollees in each state.)
Medicare beneficiaries who qualify for a State Pharmaceutical Assistance Program also have the option to join a Medicare Advantage or Part D plan at any point during the year, but only once per year.