Types Of Health Insurance Plans
When purchasing health insurance, your choices typically fall into one of three categories:
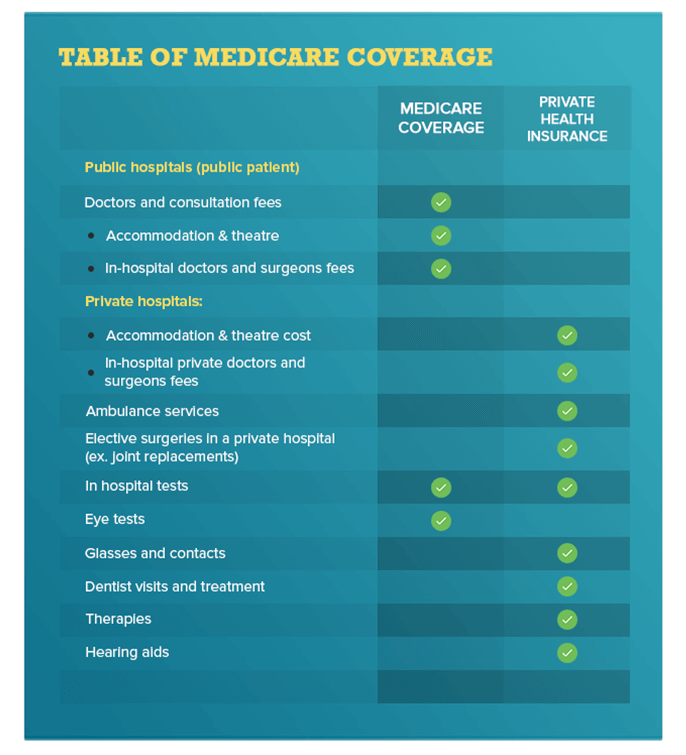
- Traditional fee-for-service health insurance plans are usually the most expensive choice. They offer the most flexibility in choosing health care providers.
- Health maintenance organizations offer lower co-payments and cover the costs of more preventive care. Your choice of health care providers is limited to those who are part of the plan.
- Preferred provider organizations offer lower co-payments like HMOs but give you more options when selecting a provider.
Does Medicare Provide Minimum Essential Coverage
Some Medicare options provide MEC, but not all do. According to HealthCare.gov, if you have Medicare Part A, then you also have MEC. That means you wont be penalized.
If you only have Part B, however, you dont meet MEC guidelines. Youll have to pay the fee or foot the bill for hospital coverage, since you havent received premium-free Part A.
Can I Choose Marketplace Coverage Instead Of Medicare
Generally, no. You can choose Marketplace coverage instead of Medicare if you have to pay a Part A premium. Before making this decision, check if Marketplace coverage meets your needs and fits your budget. Also consider:
- If you dont sign up for Medicare when youre first eligible , you might have to wait to sign up. You might also have to pay monthly late enrollment penalties.
Recommended Reading: Is Obamacare Medicaid Or Medicare
I Am In My Early 60s And Have Signed Up For A Marketplace Plan So That I Have Health Insurance Coverage Until I Qualify For Medicare At Age 65 What Happens When I Go On Medicare
When you turn 65, you should sign up for Medicare and notify your Marketplace plan that you now qualify for Medicare coverage. Your Marketplace coverage will not be cancelled automatically by your plan when you turn 65 and sign up for Medicare, but if you receive premium tax credits to help you pay for your Marketplace plan premium, your eligibility for these tax credits will end when your Medicare Part A coverage starts .
If you choose to enroll in Medicare Part A and keep your Marketplace coverage, you will have to pay the full price for your Marketplace plan, and Medicare will be the primary payer. If you were receiving financial assistance for your Marketplace coverage prior to signing up for Medicare, you will receive a letter in the mail from the Marketplace informing you that you are no longer eligible to receive this financial assistance since you are enrolled in Medicare Part A. You should contact your Marketplace plan to make sure that your financial assistance is stopped when your Medicare coverage begins. If you do not stop receiving the premium tax credit and other financial assistance for your Marketplace plan when your Medicare coverage begins, you may have to repay some or all of the amount of financial assistance you received for the months you had both types of coverage.
Understanding The Health Insurance Marketplace
The Health Insurance Marketplace is an insurance exchange that allows you to buy plans that are subsidized by the government through the Affordable Care Act. These plans will only be available to qualifying individuals, and will usually come at lower costs than other plans available on the broader market.
Many features of the Healthcare Marketplace could be discussed, but well focus only on those that relate to Medicare coverage.
Also Check: Do Medicare Supplements Cover Pre Existing Conditions
You Can’t Join A Healthcare Marketplace Plan If You Qualify For Medicare But If Your Spouse Doesn’t Qualify They Can
Obamacare plans, more officially known as Marketplace plans, are health plans available to individuals who qualify as a result of the Affordable Care Act, or ACA. The Healthcare Marketplace is a tool that allows eligible individuals to qualify for these lower-cost health plans. If you have one of these plans or are going to enroll in one, then understanding how they relate to Medicare is essential.
Well cover some general rules regarding Marketplace plans and Medicare, as well as a few specific scenarios you may find yourself in if you have one or both of these health insurance plans.
Health Coverage For People With Disabilities
If you have a disability, you have three options for health coverage through the government.
-
Medicaid provides free or low-cost medical benefits to people with disabilities. Learn about eligibility and how to apply.
-
Medicare provides medical health insurance to people under 65 with certain disabilities and any age with end-stage renal disease . Learn about eligibility, how to apply and coverage.
-
Affordable Care Act Marketplace offers options to people who have a disability, dont qualify for disability benefits, and need health coverage. Learn about the .
Read Also: Does Medicare Part A Cover Cataract Surgery
More Answers: Changing From The Marketplace To Medicare
- Can I get help paying for Medicare?
-
If you need help with your Part A and B costs, you can apply for a Medicare Savings Program.
-
You may also qualify for Extra Help to pay for your Medicare prescription drug coverage if you meet certain income and resource limits.
- What if Im eligible for Medicare, but my spouse isnt and wants to stay covered under our current Marketplace plan?
-
If someone gets Medicare but the rest of the people on the application want to keep their Marketplace coverage, you can end coverage for just some people on the Marketplace plan, like a spouse or dependents.
Key Things To Remember About Marketplace Plans
The variety of different scenarios can make understanding how Marketplace interacts with Medicare a bit complicated. Although there are many different possibilities, including ones not described here, there are a few key things to remember.
In general, you should not try to mix Medicare and Marketplace plans or switch from Medicare to Marketplace. There are a few situations in which it is possible, but it is not advised and will not be possible under most circumstances. If you are eligible for Medicare, you should transition to it in most circumstances. If you think you have a good reason to stay with a Marketplace plan, make sure to talk to the Centers for Medicare and Medicaid Services or Social Security to find out more information.
Read Also: Where Is The Nearest Medicare Office
What If I Have A Marketplace Plan Then Become Eligible For Medicare
If you are already enrolled in a Marketplace health plan, and then become eligible to enroll in Medicare, then you should cancel your Marketplace coverage to coincide with the beginning of your Medicare coverage.
Once you are either eligible for or enrolled in Part A of Medicare, you wont be eligible to receive help paying for your Marketplace plan premiums anymore. Technically, you can keep your Marketplace plan even when you have Medicare. But, you will no longer receive any help paying for your plan.
How Does The Affordable Care Act Affect Medicare
Those with Medicare coverage are unaffected by the Health Insurance Marketplace. We can assist you if you presently have a plan via the Marketplace but are aging in or are becoming eligible as a result of a disability. Until the start of your Medicare, you can continue with your current plan through the Marketplace.
Don’t Miss: Is Methadone Covered By Medicare
You Have Private Insurance Coverage Through Your Employer Or A Spouses Employer
When youre eligible for Medicare, you can still have private insurance coverage provided by an employer. Generally speaking, youre eligible for Medicare when you:
- have a qualifying disability
- receive a diagnosis of ESRD or ALS
How Medicare works with your group plans coverage depends on your particular situation, such as:
- If youre age 65 or older. In companies with 20 or more employees, your group health plan pays first. In companies with fewer than 20 employees, Medicare pays first.
- If you have a disability or ALS. In companies with 100 or more employees, your group health plan pays first. When a company has fewer than 100 employees, Medicare pays first.
- If you have ESRD. Your group health plan pays first during a 30-month coordination period. This is regardless of the number of employees your company has or whether youre retired.
Its possible that your company may offer you coverage under a group plan after you retire. This is called retiree coverage. In this case, Medicare pays first and your retiree coverage pays second.
Some health insurance plans, such as Health Maintenance Organization and Preferred Provider Organization plans, require you to use in-network providers. If this is the case with your group health plan and it pays first, you may not be covered by Medicare if you choose to use an out-of-network provider.
I Am Turning 65 Years Old Next Month But I Am Not Entitled To Medicare Without Having To Pay A Premium For Part A Because I Have Not Worked Long Enough To Qualify Can I Sign Up For A Marketplace Plan
Yes, in general, people age 65 or older who are not entitled to premium-free Medicare can purchase health insurance coverage in the Marketplace . If you sign up for a Marketplace plan, you will be eligible for premium tax credits to make the coverage in the Marketplace more affordable if your income is at least 100% of the federal poverty level .
Keep in mind that if you are able to continue working, you may be able to earn enough work history to qualify for premium-free Medicare in the future. So another option for you to consider would be to sign up for Part A and Part B coverage when you turn 65 , and when you become eligible for premium-free Part A through your work history, you will then only have to pay a premium for Part B.
Browse more questions in the section.
Also Check: What Age Can You Begin Medicare
No Automatic Plan Termination
Prior to 2014, coverage in the individual market generally terminated automatically when an enrollee reached age 65. Age was a limiting factor for enrollment people 65 and over typically could not obtain coverage in the individual market, nor could they keep it once they reached 65, even if they were not eligible for Medicare.
That has changed under the Affordable Care Act, so youll need to actively cancel your exchange coverage in order to transition to Medicare.
And under regulations that CMS finalized in 2018, insurers that offer individual market coverage along with Medicare Advantage coverage cannot automatically transition their individual market enrollees to their Medicare Advantage plan. Consumers can opt into this feature, but seamless automatic enrollment is only allowed when a person is already enrolled in the insurers Medicaid managed care plan and is going to be transitioned to a special needs plan for dual-eligible enrollees.
Medicare As Qualifying Health Coverage
The Affordable Care Act established the Individual Shared Responsibility provision that requires individuals to have qualifying health care coverage , also referred to as minimum essential coverage, qualify for an exemption, or make a payment when filing their tax return.
Medicare Part A plan) qualifies as QHC. Beneficiaries who had 12 months of QHC in 2017 simply need to check a box on their tax return to indicate that they had health coverage. Medicare mails this notice to people who had Medicare Part A coverage for part of the year.
Also Check: Does Plan N Cover Medicare Deductible
When You Can First Sign Up For Medicare
Youre first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease , or ALS .
Your first chance to sign up is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Avoid the penalty
If you miss your 7-month Initial Enrollment Period, you may have to wait to sign up and pay a monthly late enrollment penalty for as long as you have Part B coverage. The penalty goes up the longer you wait. You may also have to pay a penalty if you have to pay a Part A premium, also called Premium-Part A.
How To Enroll And Get Answers To Your Questions
You can learn more about and apply for ACA health care coverage in several ways.
-
Visit HealthCare.gov to apply for benefits through the ACA Health Insurance Marketplace or you’ll be directed to your state’s health insurance marketplace website. vary by state.
-
Find a local center to apply or ask questions in person.
-
Download an application form to apply by mail
Find the answers to common ACA questions about submitting documents, getting and changing coverage, your total costs for health care, tax options, and more.
Read Also: Is Humana Gold A Medicare Advantage Plan
How Medicare Works With Other Insurance
If you have
and other health insurance , each type of coverage is called a “payer.” When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then sends the rest to the “secondary payer” to pay. In some rare cases, there may also be a third payer.
Getting Medicare If You Already Have Marketplace Coverage
Even if you have coverage through the Marketplace, you should generally sign up for Medicare when youre first eligible to avoid a delay in Medicare coverage and the possibility of a Medicare late enrollment penalty.
Once youre eligible to sign up for Part A:
- Your Marketplace plan may not renew your coverage at the end of the year. This means you and your family could have a gap in your coverage starting January 1 of next year.
- You wont qualify for help from the Marketplace to pay your Marketplace premiums or other medical costs. If you keep getting help to pay your Marketplace plan premiums after youre eligible for Part A, you may have to pay back all or part of the help you got when you file your federal income taxes.
Once you sign up for Medicare, you need to drop your Marketplace coverage the day before your Medicare coverage starts, to avoid an overlap in coverage.
Also Check: Does Aetna Medicare Advantage Have Silver Sneakers
Appendix: Estimating Spending By Selected Marketplaces
While it is impossible to compare different exchanges costs on a truly apples-to-apples basis, examining the budgets of longstanding exchanges both state-run and the FFM that serve millions of people can provide a sense of what it costs to operate one. As discussed in this paper, the new SBMs plan to operate at a lower cost than several existing SBMs, in the range of $100 to $200 per marketplace enrollee per year in several cases. For four first-generation SBMs that we examined, as well as FFM states, it costs about $240 to $360 per marketplace enrollee per year to operate. We arrived at these ranges using the following sources:
States differ in how much they invest in functions such as marketing and outreach to hard-to-reach populations and in how much they support small business enrollment. States also have different funding sources for their operations an important parameter for what its exchange might have available to spend. Most exchanges charge user fees or assessments that are calculated as a percentage of the premiums that insurers charge, though states have made different decisions about which insurers pay the fees. Some state exchanges receive state appropriations, and those that handle enrollment for other programs can receive Medicaid cost-allocation funding for the relevant exchange functions that support those enrollees.
Use The Shift To An Sbm To Achieve Broader Policy Changes
A states decision to set up its own marketplace creates an opportunity for more significant policy changes. In particular, operating an SBM makes it easier for a state to provide state-funded subsidies to supplement those the federal government already provides to help people afford marketplace plans. States that rely on the FFM have no way to seamlessly integrate state-funded subsidies with federal premium tax credits. If a state is willing to invest in a supplemental state tax credit, this is a good reason to make the transition to an SBM.
Several states with SBMs have moved or are considering moving in this direction:
- Massachusetts has long provided sizable subsidies to people with incomes up to 300 percent of the federal poverty level. For example, people with incomes below 150 percent of poverty are guaranteed a $0 premium plan option with low out-of-pocket costs, compared to premiums of $48 to $63 per month for benchmark coverage in other states.
- Vermont provides supplemental premium and cost-sharing assistance to people with incomes between up to 300 percent of poverty.
- California provides state subsidies, beginning in 2020, for people with incomes between 400 and 600 percent of poverty and supplemental subsidies for people with incomes between 200 and 400 percent of poverty.
- Marylands exchange is studying boosting subsidies for younger people, with the goals of reducing uninsurance among this group and improving the risk profile of its individual market.
Recommended Reading: How To Check My Medicare Coverage
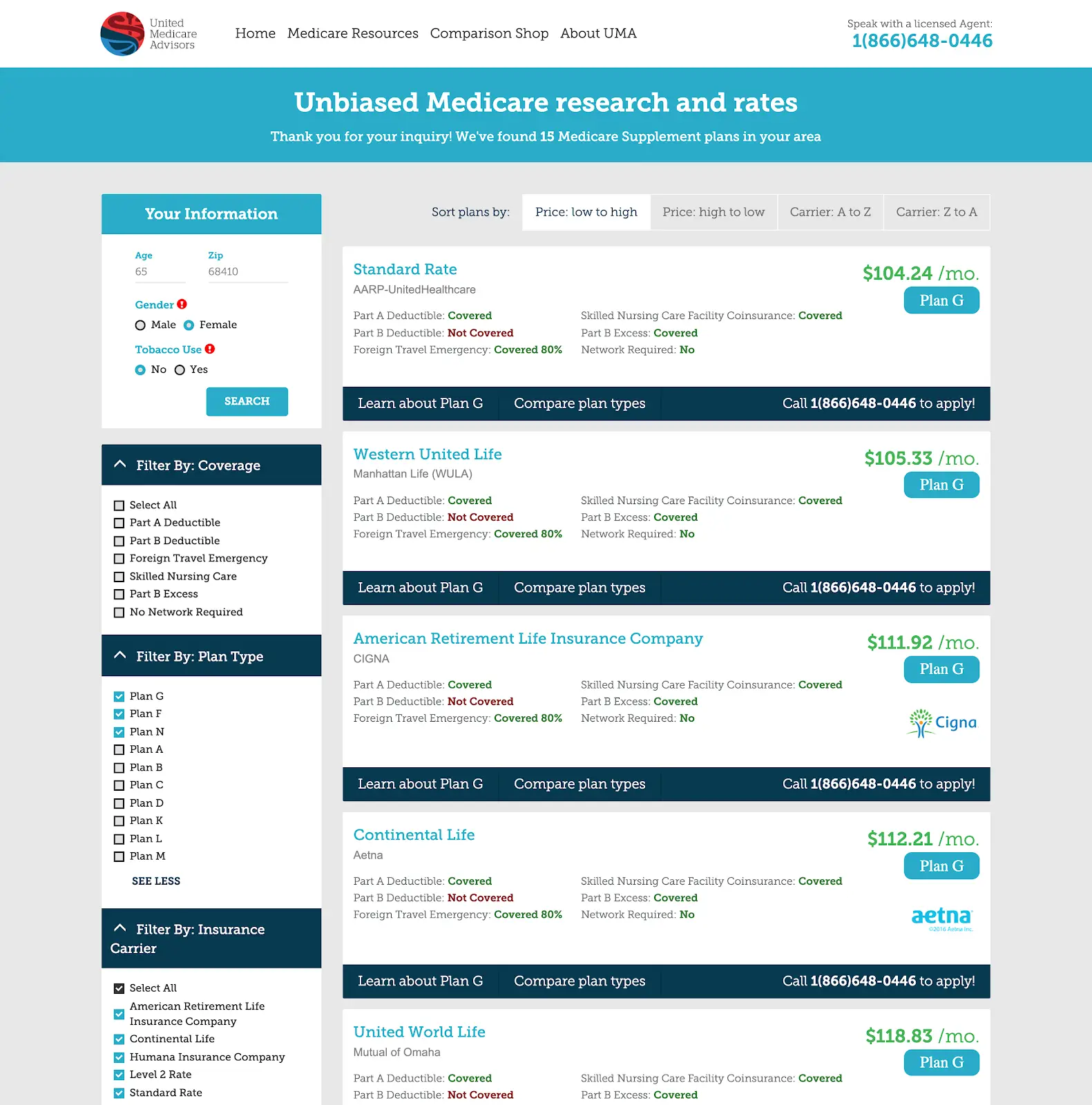
Can You Have Both Medicare And Marketplace Coverage
As a general rule, you cant have Medicare coverage and a plan from the Health Insurance Marketplace. Thats because Medicare has put several precautions in place to protect recipients. If an insurance agent knows that you have Medicare, he or she cant legally sell you a plan from the Marketplace.
- Employer-Sponsored Marketplace Plans: If you have a Marketplace plan through your employer, you can maintain your employer-sponsored plan and delay Medicare Part B enrollment. Youd typically have to pay a fee for late enrollment. Losing employer health care upon retirement, however, grants you a special enrollment period.
- Individual Marketplace Plans: If you have an individual Marketplace plan but youll qualify for Medicare coverage soon, you can cancel your Marketplace plan as soon as youve enrolled in Medicare. Dont cancel it until your new Medicare coverage begins, though. You dont want to risk getting a fine for lack of coverage or incurring medical bills during a gap period between policies. Theres no charge for canceling your Marketplace plan when you choose a Medicare plan.