Philips Cpap Machine Recall
In June 2021, millions of CPAP and BiPAP machines were recalled by Philips Respironics due to the degrading of sound abatement foam inside the machines, which can break down and lead to serious health issues like inflammation in the respiratory system, cancer and other dangerous effects.
The recall was classified by the U.S. Food and Drug Administration as a Class I recall due to the toxic effects from the machines as capable of causing severe injury or death.
According to Philips, these products are not affected by the recall:
Are Cpap Cleaners Covered By Medicare
Unlike CPAP machines themselves or their tubing, masks or replacement parts, CPAP cleaners arent covered by Medicare. Because CPAP cleaners and sanitizers arent considered DME, theyre not eligible for coverage. They can, however, be purchased with HSA/FSA funds. Always read the rules carefully for your specific health policy to ensure your HSA or FSA funds can be used to purchase any equipment or pay for services.
In addition to not paying for cleaning machines, Medicare usually wont help pay for things like mask liners, mask wipes, hose holders or tube covers. Many of these items are expensive, so buy with care.
Does Medicare Cover Sleep Apnea Machines
Yes. Original Medicare Part B , which pays for , helps cover some of the costs of sleep apnea machines if:4
- Your doctor diagnoses you with OSA after a sleep study, opens new window
- Your doctor and device provider participate in the Medicare program
- Youre up-to-date in paying your Part B premiums
- Youve met your annual Part B deductible
Once youve met your annual Part B deductible, Original Medicare helps pay up to 80% of the Original Medicare-approved amount for covered equipment.5
Also Check: How Old For Medicare Part B
What Is Sleep Apnea And How Is It Treated Through Cpap Therapy
Sleep apnea is a common condition that often plagues older adults. It is a potentially serious disorder that is characterized by repeated breathing disruptions during sleep, when ones breathing may start and stop irregularly. Sleep apnea is officially diagnosed when ones airflow stops for at least ten seconds.
Common symptoms of sleep apnea include:
- Gasping for air during sleep
- Waking up with a dry mouth
- Waking up feeling unrested or excessive daytime sleepiness
- Headaches in the morning
Sleep apnea most commonly occurs in those who are overweight, suffer from certain medical conditions (such as congestive heart failure, use tobacco, or regularly use alcohol or other sedative drugs. Sleep apnea is more common in men than women, but can affect both sexes.
There are two primary types of sleep apnea: Obstructive Sleep Apnea , in which the airway at the back of ones throat becomes blocked during sleep, and Central Sleep Apnea , which occurs when there is a miscommunication between ones brain and the control of their breathing during sleep.
Both forms of sleep apnea are typically treated through the use of a Continuous Positive Airway Pressure, or CPAP, machine, which delivers a flow of pressurized air through a mask that fits over your mouth and nose during sleep. This treatment, known as CPAP therapy, helps to keep your airway open and assist you in breathing more easily during sleep.
Medicare Guidelines For Cpap
Patients must have a face-to-face evaluation with a physician of their choice and obtain:
- Documentation of obstructive sleep apnea symptoms through a baseline sleep study
- Completed Epworth Sleepiness Scale
- Focused cardiopulmonary and upper airway system evaluation.
Note: The appointment with the physician must always come before the baseline sleep study.
Patients currently using CPAP who become Medicare patients
Patients must:
- Complete a baseline sleep study that meets Medicare criteria – It does not matter now long ago this baseline was performed.
Physicians must:
- Document that the patient’s symptoms have improved with CPAP treatment.
Patients who do not have enough OSA
- The patient must follow the “New Patients” steps, above, and try to re-qualify for CPAP.
- If the prior baseline met Medicare criteria, the first face-to-face with the physician after going on Medicare must include documentation about the patient’s CPAP compliance according to Medicare guidelines.
Don’t Miss: What Are The Qualifications For Medicare
How Much Does Medicare Cover For A Cpap Machine
Whether you have Part B through Original Medicare or enrolled in Medicare Advantage, Medicare will cover your CPAP machine similarly to other benefits. First, youll pay your deductible. Then, Medicare will pay its portion. Youll pay the remainder or coinsurance.
- How much does Medicare pay for CPAP machines? 80% of the Medicare-approved amount.
- How much will you have to pay for a CPAP machine? The remaining 20%.
In most cases, Medicare will help pay to rent your CPAP machine for 13 continuous months if you use it without interruption. After this period, you own the CPAP machine. You will still be responsible for paying the coinsurance on the rental costs.
If you have Original Medicare, you may be able to sign up for Medicare Supplement Insurance . Many states offer Medigap plans that can help cover your CPAP coinsurance during your rental period.
You May Like: How Long Does It Take For Medicare To Become Effective
How Do I Find Medicare
Once youve had a sleep test and approved for CPAP therapy, youll need to choose a CPAP machine through a Medicare-approved supplier. You can ask your doctor for recommendations or search for a nearby supplier online. Make sure your CPAP machine is Medicare-approved. If not, you may be stuck paying the total price for a device that wont work.
Recommended Reading: Does Medicare Cover When Out Of Country
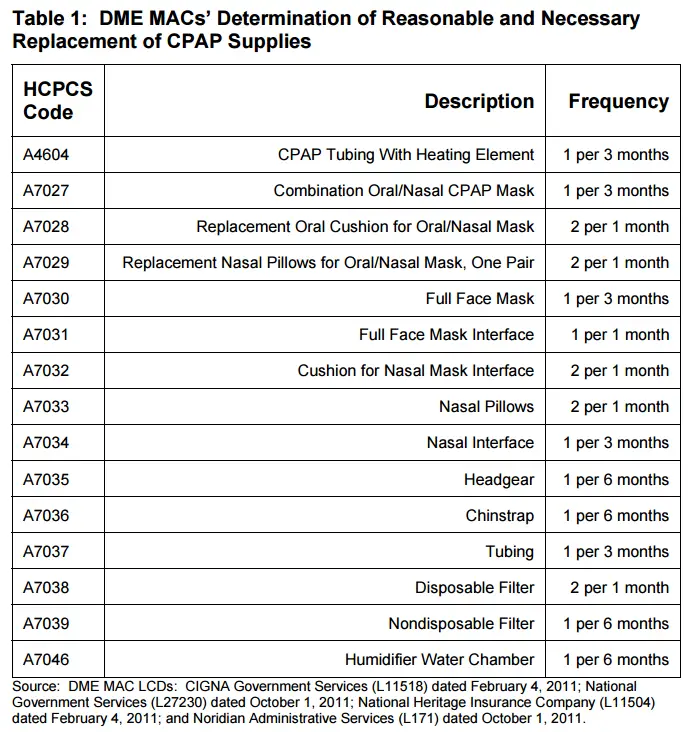
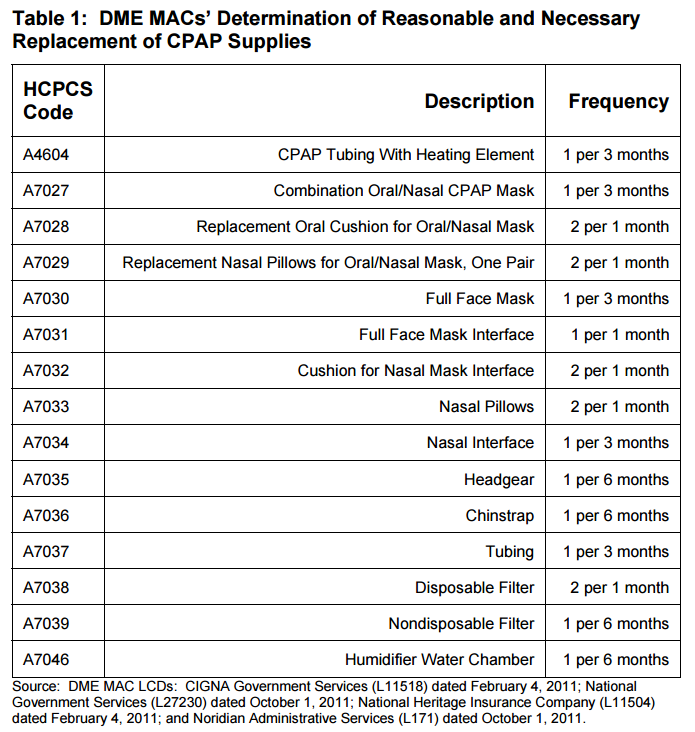
Medicare Cpap Supplies Replacement Schedule
With time and use your CPAP equipment will begin to break down, reducing the effectiveness of your CPAP therapy. To keep your treatment both effective and hygienic Medicare will cover replacements for your CPAP supplies according to the following schedule:
- Full Face Mask Cushions – 1 every month
- Nasal Pillows/Nasal Mask Cushions – 2 every month
- Disposable Filters – 2 every month
- Reusable Filters – 1 every 6 months
- CPAP Mask – 1 every 3 months
- CPAP Tubing – 1 every 3 months
- CPAP Headgear – 1 every 6 months
- CPAP Chin Strap – 1 every 6 months
- Humidifier Water Chamber – 1 every 6 months
- CPAP Machine – 1 every 5 years
It may seem like a lot to keep track of, but dont get overwhelmed! Your personal Sleep Specialist from AeroflowSleep.com can keep track of what you qualify for and when. When youre ready for fresh equipment, well send you a reminder. To get started, fill out a simple qualify form and well handle all of the paperwork for you!
When Will Medicare Cover Cpap Machines
Medicare Part B covers the use of CPAP machines by adult patients with obstructive sleep apnea. Medicare initially will cover the cost of the CPAP for up to three months if your sleep apnea diagnosis is documented by a sleep study. Medicare will cover the sleep apnea machine after the initial three-month trial period if your doctorafter meeting youdocuments in your medical record that you meet certain conditions about using the device and that you benefited from CPAP during the initial trial period.
Upon completion of the trial period, you must be re-evaluated to determine whether there is a medical necessity to warrant Medicare coverage of the CPAP machine beyond those initial three months. Medicare wont continue coverage for subsequent months without this re-evaluation.
Recommended Reading: Does Medicare Cover Spinal Fusion Surgery
What Is Medicare Cpap Compliance
Once you receive your CPAP or BiPAP equipment, youll begin a compliance period. Think of it like a three-month trial period. This is to demonstrate both that youre using your equipment and that its an effective treatment option for your OSA.
During the compliance period your doctor will monitor how often you use your CPAP. This is recorded by your CPAP device, either through an SD memory card or via Bluetooth connectivity.
To meet compliance, Medicare requires that you use your CPAP machine 1) at least 4 hours per night, 2) for at least 70% of nights, 3) for 30 consecutive days of the first three months.
That can be a little confusing, but what you need to know is: Use your CPAP machine for 30 days in a row, and at least 21 of those days need to be 4 hours or more per night.
Lastly, youll need to meet with your doctor between the 31st and 90th day of the compliance period!
Who Is Eligible For Medicare
If you are 65 or older and a U.S. citizen or have been a permanent legal resident of the United States for five consecutive years, you may automatically qualify for Medicare part A and B. An easy way to tell if you qualify is if you already receive Social Security benefits or Railroad Retirement Board benefits.
If you do not automatically receive Medicare part A and B, youll need to enroll during the initial enrollment period This period begins 3 months before you turn 65 years old and ends 3 months after your 65th birthday. The date when your coverage starts depends on when you sign up during your 7-month IEP.
There are a handful of other reasons you may qualify for Medicare that are not related to your age too. For example, you may have a disability or debilitating condition like End Stage Renal Disease people with permanent kidney failure who require either dialysis or a transplant. Check with your doctor to see if your condition meets Medicare requirements, if you are not yet 65 years of age.
Don’t Miss: What Preventive Services Are Covered By Medicare
Does Original Medicare Cover Cpap Machines
The good news is, Original Medicare may cover certain aspects of CPAP machines, CPAP supplies, and CPAP therapy depending on several conditions. First, you must have been formally diagnosed with sleep apnea by a doctor who deems CPAP therapy to be a medically necessary treatment.
After this condition is met, Original Medicare Part B will usually cover a three-month trial of CPAP therapy, but this duration may be extended if you meet in person with your doctor to assess the level of need you require and it is determined that CPAP therapy is an effective treatment for you.
What Is Sleep Apnea And How Is It Treated
Sleep apnea is a potentially serious disorder in which your breathing repeatedly stops and starts during sleep. Apnea occurs when your airflow stops for at least 10 seconds.
According to the Mayo Clinic, if you snore loudly and feel tired the next day even after a full nights sleep, you may have sleep apnea.
Most Common Types of Sleep Apnea
- Obstructive Sleep Apnea
- Occurs when the airway at the back of your throat becomes physically blocked. This obstruction causes you to temporary stop breathing.
- Central Sleep Apnea
- Occurs when there is a problem with how your brain controls muscles involved in respiration, which leads to slower and shallower breathing.
Research has found OSA to be much more common than CSA. When people use the generic term sleep apnea, theyre usually referring to OSA.
Common Signs and Symptoms of Sleep Apnea
- Excessive daytime sleepiness
Sleep apnea is most common in people who are overweight, use alcohol or sedatives, smoke or suffer from certain medical conditions such as congestive heart failure.
The condition is also more common in men than women.
The most common treatment for moderate to severe sleep apnea is a breathing device, such as a Continuous Positive Airway Pressure, or CPAP, machine.
CPAP therapy delivers a flow of pressurized air from a machine through a mask that fits over your mouth or nose. This helps keep your airway open and breathe more easily while you sleep.
Also Check: Can You Have Medicare Part D And Private Insurance
How Do I Qualify For Coverage
To qualify for Medicare coverage of a CPAP machine, your doctor has to diagnose you with OSA. This often requires a sleep study. Medicare Part B covers the cost of sleep studies as well.
If you have been newly diagnosed with OSA, Medicare will cover a 3-month trial of a CPAP machine. If your doctor documents that CPAP therapy is helping your condition and writes an order for continued therapy, Medicare will keep covering your CPAP machine.
Cpap Therapy Comes With Continuing Expenses
CPAP therapy requires periodic purchase of replacement supplies, including masks, filters, headgear, the water reservoir in the humidifier and the tubing that connects the CPAP machine with your face mask. Medicare has an approved schedule for replacing supplies and covers them on varying schedules. Your CPAP supplier should be willing to help you optimize the timing of these purchases.
Not all supplies are covered under Medicare Part B. Make sure you have a clear understanding of the additional supplies youll need.
Read Also: What Is The Requirement For Medicare
Can I Just Buy A Cpap Machine
No. In order to buy a CPAP machine, you must have results from a sleep study and a CPAP prescription from your doctor or healthcare professional.
The reason for this is that CPAP devices are a class II medical device under FDA regulation, meaning you require a prescription in order to obtain one, and in order to get the prescription, you need to undergo a sleep study and have a board-certified sleep specialist physician interpret your results and prescribe CPAP treatment before you undergo CPAP therapy.
Medigap And Cpap Machines
Medigap, also known as Medicare Supplemental Insurance, covers the gaps of Original Medicare and can provide additional coverage related to CPAP therapy. For instance, certain Medigap plans in tandem with Medicare coverage might be able to cover the full cost of CPAP machine rentals or accessories needed for the machine for your sleep apnea, as long as your physician certifies that it is medically necessary and is improving your health.
Pro Tip: There are currently 10 different types of Medigap plans offered by private insurers. To help you get started, read my list of affordable medicare supplement plans.
You May Like: What Type Of Insurance Is Medicare Part D
Option : Use Medicares Website
If you have a Medicarehealthcare plan, you can also find in-network durable medical equipment providers by using Medicares Supplier Directory. After you click the link, enter your zipcode and select the corresponding product category. For CPAP machines and related supplies, select . After you click the search button, the website will provide you with a list of vendors in your area that provides CPAP equipment and accepts Medicare insurance.
For the lucky few of you, you may be able to find a MedicareDME provider that is relatively close to you however, for others, the drive from your home could be long and inconvenient. Luckily, Health Sqyre will ship your desired CPAP products right to your door!
Read Also: How Do You Qualify For Medicare In Texas
Do Medicare Advantage Plans Cover Cpap Machines
Yes. Remember, Medicare Advantage plans must prove at least the same coverage as youd get from Parts A and B with Original Medicare. The most significant difference may be in what you pay out of pocket. To find out exactly what your coverage options are with your Medicare Advantage plan, contact your insurance carrier. You can also call GoHealth. Our licensed insurance agents will go through your benefits and help you understand whats covered and how. Breathe easier knowing GoHealth can help you get the CPAP machine and supplies you need.
Also Check: Can I Keep Medicare If I Get A Job
Get An Initial Clinical Evaluation
For Medicare to cover a CPAP machine, you must first have a face-to-face evaluation with your primary care physician to assess you for obstructive sleep apnea. Youll then take a sleep test that your doctor will use to document in your medical record symptoms of sleep apnea. If you have sleep apnea, Medicare may cover your CPAP machine for an initial three-month trial period.
How Much Does A Cpap Machine Cost With Medicare

Generally, Medicare covers 80 percent of costs related to sleep apnea machines. The Part B deductible applies.
You may pay less or owe nothing if you have Medicaid as your secondary payer.
Medicare Advantage plans also generally cover CPAP machines and therapy because these plans must offer at least the same coverage as Original Medicare.
Many Medicare Advantage plans require doctors to submit a prior authorization request before the insurer will pay for a sleep study or CPAP machine.
Because CPAP treatment doesnt work for everyone, Medicare initially covers the machine for a three-month trial period after you are diagnosed with sleep apnea.
Medicare may extend coverage if your doctor determines that the therapy is helping your condition.
After this three-month trial, you will owe 20 percent of the Medicare-approved cost to rent the machine as durable medical equipment.
The equipment supplier will provide you with instructions on how to use the CPAP machine.
Medicare pays its share to the supplier to rent the machine for 13 months. After that, you own the machine outright.
You must rent your device from a supplier enrolled in Medicare, and the doctor who orders your sleep apnea machine must also accept Medicare.
Medicare will usually cover the cost of a new CPAP machine every five years.
If you had a machine before enrolling in Medicare, Medicare may cover some of the costs for a replacement CPAP machine rental and accessories if you meet certain requirements.
Read Also: Does Medicare A Have A Deductible
What Is A Cpap Machine
If you have OSA, continuous positive airway pressure machines, opens new window are one of the most common treatments. A CPAP machine is a device with a face or nose mask attached to a small pump. The pump pushes pressurized air through a hose, into the mask and into your airway. The steady flow of air keeps the airway open to improve breathing and sleep quality. Some people may require extra CPAP supplies like humidifiers and heating tubes for effective treatment.3
You May Like: Does Medicare Cover Oral Surgery Biopsy
