Coverage Amounts And Co
While some services are covered fully, such as depression screenings, others may require the beneficiary to pay 20% of the Medicare-approved amount. That includes visits to a healthcare provider to diagnose mental health conditions. Services that are provided by hospital outpatient services may be subject to additional co-pays.
Co-pays can be reduced by combining Medicare with other insurance plans.
Inpatient Mental Health Care
Some mental health care requires individuals to be admitted to a hospital as an inpatient. These services are given either in a general or psychiatric hospital.
In this case, Medicare Part A will pay for up to 190 days of inpatient psychiatric hospital services over your entire lifetime in as many benefit periods as you need. Keep in mind, Medicare wont cover:
-
Private duty nursing.
-
A phone or television in your room.
-
Personal items, like toothpaste, socks, or razors.
-
A private room, unless medically necessary.
Outside of these, Medicare will help cover the costs associated with inpatient mental health care. For additional services your healthcare provider recommends , you will have to pay some or all of those costs. Talk with healthcare provider for guidance.
If you or someone you know is in crisis, call the National Suicide Prevention Lifeline at 1-800-273-TALK . TTY: 1-800-799-4TTY . You can call and speak with a counselor 24 hours a day, 7 days a week.
Reference Links
Medicare Plus A Medicare Supplement Plan Can Help You Save Money For Mental Health Treatment
Navigating mental health problems can be challenging, but Medicare helps ensure you have one less thing to worry about.
Original Medicare can cover common treatment options, and a Medicare Supplement plan can help ease your financial burden during this already stressful time by paying for certain Medicare deductibles, coinsurance, copays and more. That means you can focus on improving your mental health without worrying about the cost of treatment.
A licensed agent can help you decide on a Medicare option that works for you. Call today to speak with a licensed agent and compare the Medigap plans that are available where you live.
You May Like: What States Have Medicare Advantage Plans
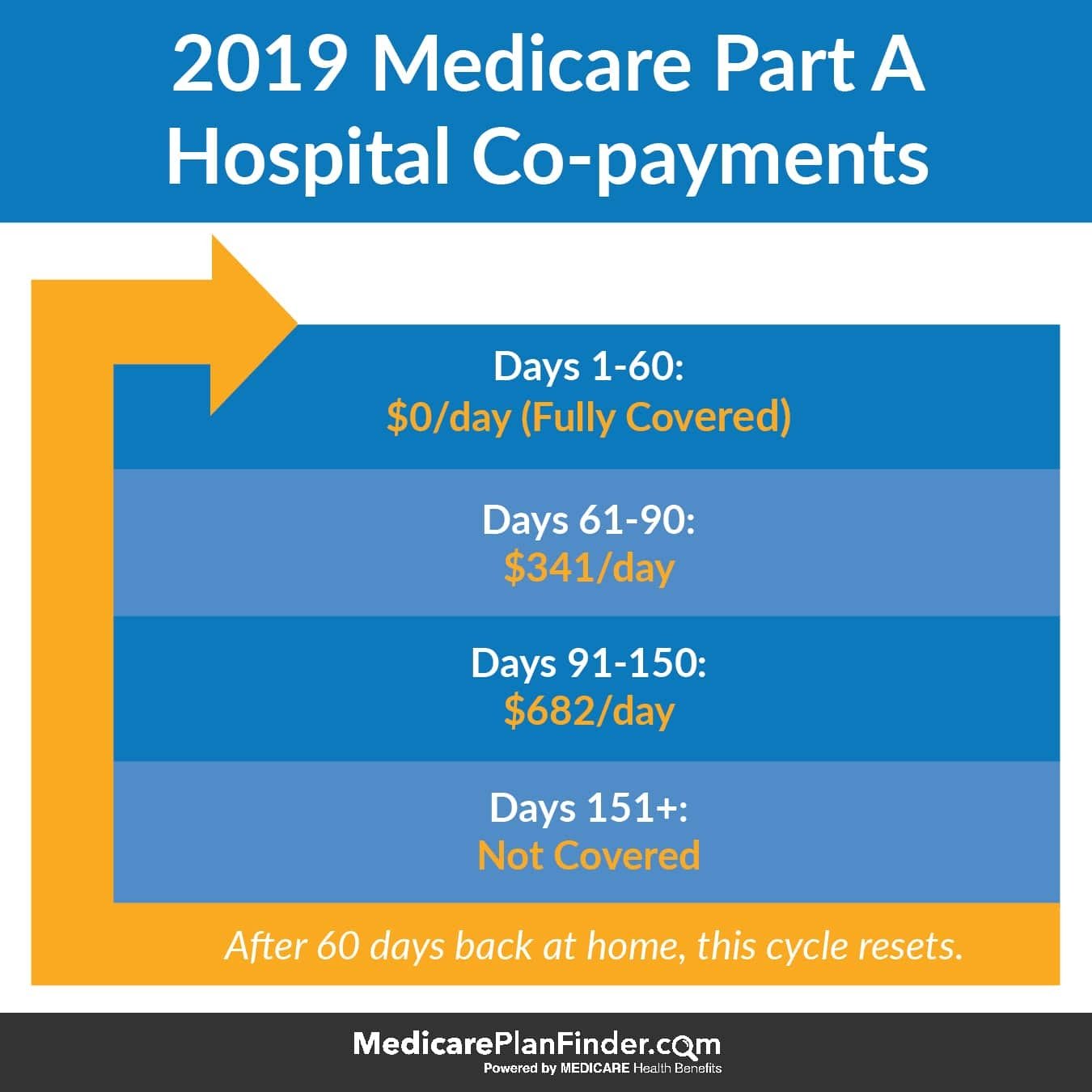
What Youll Pay For Inpatient Mental Health Care
A deductible of $1,484 applies to inpatient psychiatric care for each benefit period. You will owe no coinsurance for the first 60 days of a hospital stay for psychiatric treatment. But you will owe copays of 20% of the Medicare-approved amount for mental health services you receive from doctors and other providers while you’re an inpatient.
For days 61 through 90 of a psychiatric hospital stay, youll owe $371 per day in coinsurance. Your daily coinsurance jumps to $742 per each lifetime reserve day after day 90. After that, you pay all costs.
Prescription Drug Coverage Under Medicare
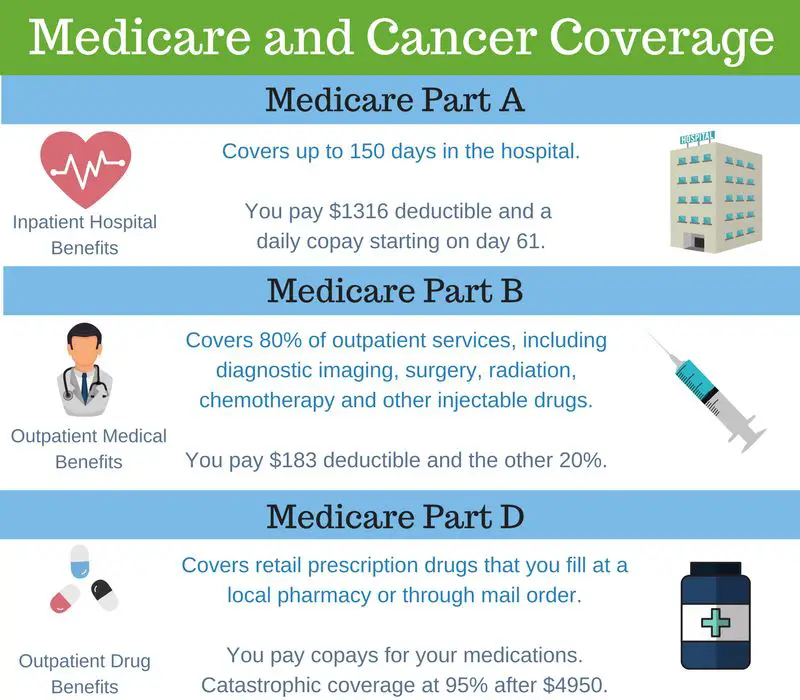
Sometimes doctors might prescribe drugs to treat mental health conditions. Medicare Part A and Part B have limited prescription drug coverage. You might want to look into prescription drug coverage under Medicare Part D. You can get prescription drug coverage either through a stand-alone Medicare Part D prescription drug plan, or a Medicare Advantage prescription drug plan. These plans are offered by private insurance companies approved by Medicare. Read more about Medicare Part D.
If you enroll in a Medicare prescription drug plan, you may want to be sure your medications are covered. Each plan has its own formulary, which is a list of covered drugs. All plans are required to cover basic medications used for mental health treatment, including antidepressants, antipsychotics, and anticonvulsants. Make sure your specific medications in your plans formulary.
Don’t Miss: Does Medicare Pay For Licensed Professional Counselors
Do I Qualify For Medicare Mental Health Coverage
If youve been diagnosedwith a mental health condition, you most likely qualify for the mental healthservices that Medicare offers. Common conditions include anxiety, depression,addiction, and eating disorders. Symptoms of mental health conditions caninclude, but arent limited to:
- Loss of interest/lack ofenergy
- Feeling of hopelessness
- Poor appetite
- Suicidal thoughts oractions
If you or someone youknow is experiencing these symptoms, proper treatment can help tremendously.
When To Enroll In Medicare Part B
The periods to enroll in Medicare Parts A or B are the same. You are eligible to enroll in Medicare Part B if you are a US citizen who is 65 or older. If you meet these requirements, you can first sign up during the 7-month Initial Enrollment Period. For most people, this begins three months before their 65th birthday and ends three months after.
Continue reading: When to signup for Medicare?
If youre receiving retirement benefits, you dont need to worry about signing up you will automatically be enrolled in Medicare Parts A and B when you turn 65.
If you miss the initial enrollment period and havent begun collecting retirement benefits , you can enroll in Medicare Part B during the General Enrollment Period. This period begins at the start of every calendar year and continues for three months .
Agent Tip
If you dont enroll in Medicare Part B on time, you can be subject to a life-long penalty. If you are unsure if you should sign up you give us a call at .
Finally, some people can sign up for Part B during a Special Enrollment Period . SEPs provide a way for people covered under a group health plan to sign up for Part B. However, even if you do have a group health plan, youre only eligible if youre working or have finished work within the last eight months.
Don’t Miss: What Is Medicare Premium Assistance
What Medicare Covers For Inpatient Mental Health Services
Medicare Part A, your hospital insurance, covers mental health services that require your admission to a psychiatric or general hospital. If youre in a psychiatric hospital, youre covered for only up to 190 days of inpatient services over your lifetime. After that, youd need to receive mental health services in a general hospital to be covered.
Your costs will also be substantial: For long hospital stays, they could amount to $10,000 or more in total charges.
Does Medicare Cover Family Counseling
Medicare Part B may help pay for family counseling if the goal of the therapy is related to helping your treatment. In addition, grief and loss counseling may be covered by Medicare for qualified hospice patients and their families, if it is provided by a Medicare-approved hospice and available in that state. Medicare does not cover other types of relationship counseling, such as marriage counseling. Youre only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Don’t Miss: Does Medicare Part C Cover Home Health Care
Compare Medicare Advantage Plans That Cover Counseling
For California residents, CA-Do Not Sell My Personal Info, .
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
What Part Of Medicare Covers Mental Health Care
Medicare Part A covers mental health care in an inpatient setting. Part A mental health care is in a general hospital or a psychiatric hospital only for people with mental health concerns. If you get inpatient care in a psychiatric hospital, Part A will cover up to 190 days in a lifetime. There is no limit to the number of benefit periods you can have for mental health care in a general hospital.
Part A covers your room , meals, nursing care , therapy and treatment, lab tests, medications, and other services and supplies you need. Part A does not cover personal items or a phone or TV in your room.
Medicare Part B covers mental health care on an outpatient basis in these types of settings:
- A doctors or other health care providers office
- A hospital outpatient department
- A community mental health center
And from these types of providers :
- Psychiatrist or another doctor
- Clinical psychologist, social worker, or nurse specialist
- Nurse practitioner
- Physician assistant
Part B helps pay for these outpatient mental health services:
Part D helps cover self-administered prescribed drugs.
Medicare Advantage plans cover all services offered through Original Medicare Part A, Part B, and usually Part D. Copays and coinsurance amounts vary, depending on your plan. Providers and services must be in-network and typically require referrals and prior authorizations before you can receive services.
You May Like: How To Get Prior Authorization For Medicare
Does Medicare Cover Substance Abuse Treatment
Mental health conditions and substance abuse can often go together, according to the Centers for Disease Control and Prevention. When your provider determines you require reasonable and necessary professional treatment for substance abuse, Medicare might cover both outpatient and inpatient care. Coverage may include diagnosis and treatment, patient education, and psychotherapy.
As with mental health services, Medicare Part A may cover hospitalization for substance abuse. Medicare Part B may cover outpatient care at a clinic or hospital. If you are enrolled in a Medicare prescription drug plan, your medications might be covered. Medicare prescription drug plans are required to cover medications necessary to treat substance use disorders.
How Much Does Medicare Part B Cost
In 2022, Medicare Part B has an out-of-pocket annual deductible of $233 which must be met before medically necessary services will be covered.
In addition to the annual deductible, youll pay a monthly premium. The standard monthly premium for Medicare Part B in 2022 is $170.10.
If youre still working and have an annual income of more than $91,000, your monthly premium may be higher. If youre married and you and your spouse have an annual income of more than $182,000, your monthly premium may be higher.
Don’t Miss: Does Medicare Cover Gastric Bypass Revision
More About Medicare Part D And Mental Health Coverage
As mentioned earlier, Part D covers prescription drugs. In this case, it covers drugs that treat a mental illness.
Unfortunately, Part D doesn’t cover all such drugs. It does cover nearly all anticonvulsant, antidepressant, and antipsychotic medications, however.
Of course, there are exceptions. Before you enroll in a Part D plan, make sure it covers whatever drugs you take for your condition.
Note: you can do this quickly and easily at medicare.gov/find-a-plan.
What Is Grief Counseling
Grief counseling, also called bereavement counseling, can help guide people through the grieving process. While grief counseling is often related to the loss of a loved one, people can also grieve over other big life changes, such as the loss of a relationship or job.
Grief counseling can involve services such as:
- individual counseling services
Any qualified mental health professional can lead you through the grieving process, but some specialize in mental health conditions that often accompany grief, like depression and anxiety.
No matter which treatment route you choose, working with a mental health professional can help you get the support you need during the grieving process.
Even if youre covered for mental health services under your Medicare plan, you may still need to pay some out-of-pocket costs associated with your care.
These costs may include:
- Part A premium of up to $458 per month
- Part A deductible of $1,408 per benefits period
- Part A coinsurance of $352 or more per day after 60 days
- Part B premium of $144.60 or more per month
- Part B deductible of $198 per year
- Part B coinsurance of 20 percent of the Medicare-approved amount
- Part C premium, deductible, drug premium, and drug deductible
- Part D premium and deductible
- Medigap premium
Part C, Part D, and Medigap costs depend on the type of plan and coverage your plan offers, among other factors.
Don’t Miss: What Income Is Used To Calculate Medicare Premiums
Medicare Coverage Of Preventive Mental Health Services
Medicare Part B covers preventive services that address your mental health, including screenings to identify your risk for depression or substance abuse. You generally need to get these services from a Medicare-assigned health provider in a Medicare-enrolled facility to make sure Part B covers them.
Preventive benefits related to mental health coverage include:
- Depression screening: All Medicare Part B beneficiaries are covered for one depression screening every year at no cost, so long as the doctor accepts Medicare assignment.
- Alcohol misuse screening: All Medicare Part B beneficiaries who arent alcohol-dependent are covered for one alcohol misuse screening every year. If your doctor determines you misuse alcohol, you may qualify for up to four counseling sessions per year.
- Welcome to Medicare visit: This one-time preventive exam includes a review of your overall health and includes an evaluation of your risk for depression. The visit is completely covered if you have the visit within the first year of having Medicare Part B.
- Wellness visit: After the introductory visit, all Medicare Part B enrollees are covered for one preventive visit every year. If you have any questions or concerns about your mental well-being, youll have the chance to speak with your doctor during this exam. Your doctor may discuss treatment options or refer you for additional care.
Does Medicare Advantage Cover Mental Health Care
Medicare Advantage does cover mental health care. While Medicare Advantage plans replace Original Medicare with a smaller, local network, they must cover what Medicare covers however, the costs for each service may vary. You will want to check with each plan to see how much Medicare Advantage will cost you for mental health services.
To learn more call a Senior65 agent at 800-930-7956.
Related Articles:
- New to Medicare: Everything you need to know. Medicare is the United States federal health insurance program for Americans 65 and older, as well as people with certain disabilities or End Stage Renal Disease .
- Pros and Cons of Medicare Advantage Finding the right Medicare insurance can be rather confusing for seniors – especially when parsing through the 150-page “Medicare and You” booklet that the government sends out as you approach age 65. We have made a list of the advantages and disadvantages of choosing a MA plan that should help
- Medicare Insurance Switching: Ultimate Guide With so many different plans, carriers, deductibles and what not, picking the wrong plan happens. A lot. Check out your options.
Read Also: Is A Psa Test Covered By Medicare
Mental Health Care Services Covered By Medicare Part B
Your Part B benefits include:
- One yearly screening for depression, when performed in a primary care doctor’s office or primary care clinic that provides referrals and/or follow-up treatment. You pay nothing for your annual depression screening. Go to Medicare.gov for more details.
- Alcohol misuse screening and counseling for Medicare beneficiaries who are not considered alcohol dependent. Includes up to four face-to-face counseling sessions per year. Telehealth services are also available. You have no out-of-pocket costs assuming your provider accepts assignment.
- Diagnostic tests.
- Family counseling, assuming it is related to your mental health treatment.
- Medication management.
- Opioid use disorder treatment services, including counseling, drug testing, individual and/or group therapy, and medication. Counseling and therapy services may be in-person or via telehealth. You pay nothing for these services if you use a Medicare-enrolled opioid treatment program.
- Partial hospitalization.
- Psychiatric evaluation.
- Psychotherapy either individual or in a group setting assuming the provider is licensed to practice in your state.
- Some prescription medications that are usually administered by a healthcare provider, such as injections.
- Testing to determine whether your treatment is helping and if you could benefit from additional services.
- Your one-time Welcome to Medicare visit .
- Your yearly Medicare wellness visit .
How Much Does Counseling Cost
The cost of counseling without coverage varies by the area, the counselors specialization, and the length of counseling sessions. Counseling costs usually range between $65 to $250 per hour, but they can be higher if the counselor has a greater reputation and specialization.goodtherapy.org, How much does therapy cost?, Accessed November 17, 2021
Medicare Part B will cover 80 percent of approved costs for counseling services ordered by your doctor once you have paid the annual Part B deductible. As an inpatient, Medicare Part A will cover all approved counseling services once the Part A benefit periodA benefit period is a method used in Original Medicare to measure a beneficiaries use of hospital and skilled nursing facility services. With each new benefit period, the beneficiary is charged a new benefit… deductible has been paid. If the counselor charges Excess ChargesA Medicare Part B excess charge is the difference between a health care providers actual charge and Medicares approved amount for payment…., you will pay those out-of-pocket unless you have a Medicare Advantage plan or a MedigapMedicare Supplements are additional insurance policies that Medicare beneficiaries can purchase to cover the gaps in their Original Medicare health insurance coverage…. policy that covers Excess Charges.
You May Like: Does Medicaid Cover More Than Medicare
The Basics Of Medicare And Mental Health Care Coverage
With that out of the way, here’s what you need to know about how Medicare does and doesn’t cover mental health care.
According to medicare.gov, Medicare Part A helps pay for the following during inpatient hospital stays:
- You room
- Nursing care
- Other related services and supplies
Medicare Part B, on the other hand, helps pay for mental health services provided outside of a hospital. A few examples:
- Psychiatrist or other physician appointments
- Clinical psychologist or clinical social worker visits
- Doctor-ordered lab tests
Something else Part B covers: partial hospitalization for people who require coordinated outpatient care.
Finally, Medicare Part D covers prescription drugs needed to treat a mental illness or mental health condition.
