Medicaid Programs & Waivers
Medicaid is health insurance for low-income and disabled individuals and seniors. Medicaid care was originally provided as institutional care, but now also covers a variety of services and benefits in ones home and community. This is to prevent and / or delay nursing home placements. In Illinois, there are two managed care health plans that are relevant to the elderly.
1) HealthChoice Illinois is for Medicaid eligible state residents of all ages, as well as those who are dual eligibles, meaning they are enrolled in both Medicaid and Medicare. Via this program, long-term care services are available and include assistance with Activities of Daily Living , such as bathing, grooming, and mobility, home health care, and adult day care. This program has lower income limits than do the HCBS Medicaid waiver programs. Learn more about program eligibility and benefits.
2) Illinois Medicaid-Medicare Alignment Initiative is intended for disabled individuals and seniors who receive both Medicaid and Medicare benefits. This health plan streamlines the services from both programs, allowing program participants to receive all services via one plan. Adult day care, personal care assistance, personal emergency response systems and other long-term supports are available via MMAI. Unfortunately, this program is not currently available statewide. To see where MMAI is available, .
- Personal care assistance
Which Services Will Medicaid Cover
The types of services covered by Medicaid will vary based on state programs. But the typical services paid for by Medicaid for those in assisted living include:
- Personal care assistance, which includes help with dressing, bathing, toileting and eating
- Specialized home care services, including house cleaning, laundry, shopping for groceries and other essentials, and meal preparation
- Transportation
Paying For Room And Board In Assisted Living
Since Medicaid only covers seniors with limited financial resources, it makes sense that beneficiaries often have trouble paying the remaining costs of room and board in an assisted living facility. However, some states do take steps to help Medicaid residents make ends meet. For example, certain states place limits on the amount assisted living facilities may charge Medicaid patients for room and board. Other non-Medicaid programs like Supplemental Security Income and optional state supplements are available to help cover costs. Another option is to seek out private programs and charities for financial assistance. Lastly, veterans and surviving spouses of veterans may also qualify for a VA pension to help cover long-term care costs.
You May Like: Does Medicare Cover Cosmetic Surgery
Are There Any Allowable Transfers
Yes. Some transfers for less than fair market value will not affect eligibility. These include:
- An applicants home transferred to certain people,
- Charitable gifts and gifts to family members which are consistent with past gifts, and
- Involuntary transfers due to bankruptcy, theft, elder abuse, the death of a spouse, or because the person was mentally unable to handle their affairs.
An applicants home may be transferred to:
- A spouse,
- A dependent, blind or disabledadult child,
- A sibling with an equity interest in the home who lived in the home for at least one year before the applicant entered the nursing home, or
- A child who had lived in the home continuously for at least 2 years before the parents admission to the nursing home. This applies if the child provided care which prevented an earlier nursing home admission
Payment to a family member or friend for providing housing, care or services will be considered a non-allowable transfer unless it is supported by written documentation made before the housing, care or services were provided.
Financial Assistance For Assisted Living In Illinois

While many seniors in Illinois pay for assisted living costs from their personal financial reserves or long-term care insurance, several other options are available for low-income residents.
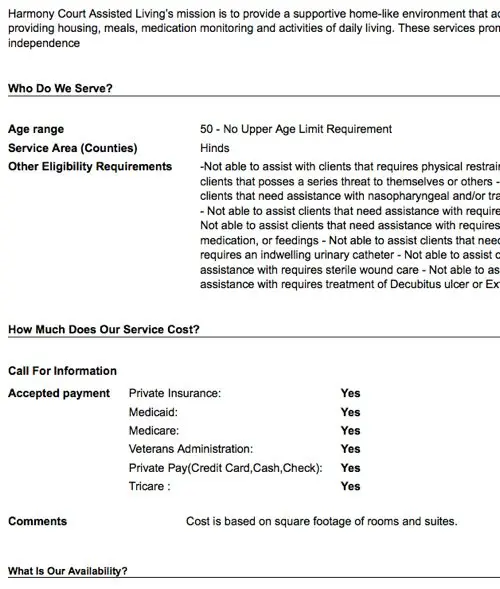
Illinois Supportive Living Program
The Illinois Supportive Living Program gives low-income seniors access to services not normally covered by Medicaid, such as those provided by living in an assisted living community. This is accomplished through a waiver to the Medicaid program. The Illinois Department of Healthcare and Family services administers the SLP program, which covers all services besides room and board. The resident remains responsible for all room and board costs.
Who Is Eligible?
Those applying for the SLP waiver must be Illinois residents. In addition, they must:
- Be 65 or older – Alternatively, they can be 22 to 64 and have a physical disability
- Have an income greater than the Supplemental Income maximum of $750 per month, as of 2018
- Not have any developmental or cognitive disabilities
How to Apply
If eligible, seniors should contact the DHF Bureau of Long Term Care for further information and instructions for application.
IMPORTANT NOTE: Assisted living communities make their own determinations on the types of payments they will accept from residents. Ask each residence youre interested in what programs they participate in, whether they offer additional programs for lower-income individuals and what payment types they prefer.
Read Also: How To Get A Lift Chair From Medicare
Does Medicare Advantage Cover Dementia
Advantage plans must offer the same benefits as Medicare. That means you can expect your Medicare Advantage plan to cover an annual dementia screening as well as medical costs.
Medicare Advantage plans come with deductibles, copays, and doctor networks, so your costs may be different than if you had Medicare.
Advantage plans could benefit dementia patients:
- A Medicare Special Needs Plan for dementia is tailored to the needs of dementia patients.
- Some Medicare Advantage plans may offer in-home long-term care benefits beyond whats available under traditional Medicare. These benefits might include adult daycare, nutrition services, or in-home caregiving.
Advantage plans vary by location. Plans geared toward dementia and long-term care may or may not be available in your area.
How Do I Pay For Dementia Care
With limited Medicare coverage, families of dementia patients often wonder how to pay for care.
Here are common approaches:
- Long-term care insurance may cover in-home care or the cost of a long term care facility
- Veterans and their spouses may be eligible for a monthly Aid and Attendance benefit
- Family members may pitch in by doing the caregiving themselves or paying for care
- Medicaid, the state insurance program for people with limited assets and income, will pay for a nursing home if the person with dementia qualifies. In some states, Medicaid will pay for assisted living. Medicaid may also help with in-home caregiving costs.
Also Check: Does Social Security Automatically Sign You Up For Medicare
Does Medicare Cover Dental
Typically, Medicare Part A and Part B does not cover most dental care, dental procedures, or supplies, like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices. There are some exceptions to this rule, such as an emergency or complicated dental procedure that requires a hospital stay. For dental coverage, the best option is a Medicare Advantage plan, which covers routine dental services, such as checkups or cleanings.
How To Find Senior Assisted Living Near Me
The U.S. Department of Health & Human Services offers a state-by-state guide to assisted living resources. In many cases, the most comprehensive information about senior assisted living near me will come from your Area Agency on Aging.
Your healthcare provider or your plan may be able to help. If you believe a different provider or plan may be more beneficial to your situation, GoHealth can help you with coverage details and compare options.
Recommended Reading: What Is The Best Medicare Part D Plan For 2020
What Types Of Activities Are Available For Residents
Most Assisted Living Communities have varied activities ranging in arts and crafts, wine tastings, live musical entertainment, visits to local attractions and events, tours, shopping and dining outings, outdoor activities, and more. Social activities and entertainment keep residents minds and bodies active and boost wellness.
How Much Does Assisted Living Cost
The median annual cost for an assisted living facility in 2020 was $4,300 a month, adding up to nearly $52,000 per year. The cost of an assisted living facility can depend on its location. Some areas of the country can be more expensive than others. Its helpful to compare available options before choosing.
You May Like: What Is The Best Medicare Advantage Plan In Washington State
What Medicaid Does Cover In Assisted Living
The exact services that Medicaid covers will vary by state and the specific program a senior enrolls in. All states offer some degree of personal care services , but the ways in which they are administered differ widely. For example, some state Medicaid programs provide eligible seniors with personal care assistance but not in an assisted living residence.
Generally, though, the fundamental services that most Medicaid programs will pay for in an assisted living facility include:
- Personal emergency response systems
How Much Income May A Nursing Home Resident Keep
A resident receiving Medicaid may keep a small portion of their income. This is called the Personal Needs Allowance . The amount changes from time to time. The current amount can be found on the IDHS website.
Deductions may be made from the income going to the nursing home. These may be for:
- Dependent children,
- Maintaining a home if the resident expects to return home within six months and there is no community spouse,
- Medicare and other health insurance premiums,
- Incurred medical expenses, or
You May Like: Does Medicare Cover Cpap Masks
Does Medicare Cover Assisted Living In California
At some point in our lives, most of us will need some type of long-term care services. If you are not able to arrange these services at home, there are facilities that accommodate people with long-term care needs. Examples are a skilled nursing facility , a continuing care retirement community and an assisted living arrangement.
Medicare Benefits Solutions
1 people found this article useful
Varied levels of careSkilled nursing facilities are synonymous with nursing homes. SNFs offer comprehensive health and personal care support. The focus is on medical care. It usually includes nursing services, 24-hour supervision, all meals and help with daily activities. SNFs are equipped to provide housing on a permanent or temporary basis.
Medicare benefits for long-term careMedicare does not cover long-term services. Also known as custodial care, long-term care includes non-medical services and non-skilled assistance, such as help with dressing, bathing and meals. However, under Part A, Medicare benefits include short-term care in an SNF under certain conditions. If you have been an inpatient in a hospital for at least three days, you may qualify for medically necessary SNF coverage for a related illness or injury. Benefits are covered for up to 100 days.
What Is Assisted Living
According to the National Institutes of Health and Eldercare.gov, an assisted living facility is a long-term care option combining housing and daily self-care support services. Typically, assisted living facilities dont offer full-time skilled nursing care, but they might help monitor your health and manage your prescription medications. You may be wondering about Medicare coverage of assisted living situations.
Medicare generally does not cover assisted living. Original Medicare includes Part A and Part B . The other two parts of Medicare, Part C and Part D , also dont cover assisted living costs.
Medicare Advantage gives you a different way to receive your Original Medicare benefits you get them through a private insurance company that contracts with Medicare instead of directly from the government. They provide all your Medicare Part A and Part B benefits except hospice care, which Part A continues to cover. Medicare Advantage plans might include other benefits, such as prescription drug coverage or routine dental care.
People who choose assisted living facilities may need help preparing meals, eating, bathing, dressing, attending to personal hygiene, and/or managing their daily medications.
Don’t Miss: How To Apply For Medicare In Alaska
Illinois Supportive Living Program
The Illinois Medicaid waiver that helps pay for some assisted living costs is referred to as the Supportive Living Program . It pays for personal care services, housekeeping, meals, exercise programs, medication supervision and assistance, and 24-hour staff to ensure residents scheduled and unscheduled needs are met. Residents are responsible for room and board costs.
Who Is Eligible?
Residents interested in applying for the SLP must meet the following age, financial, and functional requirements:
- Age 65 or older or have a physical disability
- Monthly income must be equal to or greater than the Supplemental Security Income rate of $750 for single residents or $1,125 for married residents
- Eligible for nursing home care but choose to receive care in an AL environment
If eligible, all of your monthly income except for $90 will go to the assisted living facility.
How to Apply
To apply for the SLP, residents or their legal representative should contact the ALF, and they will help complete the appropriate assessments and paperwork. Not all facilities accept the waiver, so be sure to ask if they are an SLP participant.
Interested applicants who would like more information about SLP or those with questions about an ALF, can also call the Department of Healthcare and Family Services, Bureau of Long-Term Care at 782-0545 or 528-8444.
How Much Does Medicaid Pay For Assisted Living
The amount Medicaid will pay depends on several factors, including:
- State of residence
- The state Medicaid program
- Level of care needed
A needs assessment is usually required to calculate the number of hours that Medicaid will cover. For example, those with a greater need for assistance can get a greater amount of caregiver hours per month.
Also Check: Does Medicare Require A Referral For A Colonoscopy
Background Checks For Assisted Living
Assisted living facilities in Illinois are required to comply with the Health Care Worker Background Check Act. They cannot hire or retain anyone who has been convicted of committing or attempting to commit one or more of the disqualifying offenses set forth in section 25 of the act. The only exception is if the individual has a waiver granted by the Illinois Department of Public Health .
Paying For Assisted Living With Your Life Insurance
Some life insurance policies can be used to pay for assisted living or other long-term care.
- Accelerated death benefits: Also known as ADBs, this feature gives you a cash advance on your life insurance policy. Details vary depending on your policy. Typically, you must meet certain qualifications, such as having a terminal illness, requiring long-term care, or being confined to a nursing home.
- Combination products: Some insurance companies let you combine life insurance and long-term care insurance into a single policy. This way, if you’re part of the two-thirds of people who never need long-term care insurance, there’s still a payout at the end.
- Life settlements: You may be able to sell your life insurance policy if you meet your insurer’s requirements .
- Viatical settlements: If you are terminally ill, you may choose to sell your life insurance policy to a third party and use the money to pay for long-term care. The third party that buys your policy becomes the beneficiary.
We cannot stress enough how important it is to talk to a financial advisor before making any decisions on how you’ll pay for long-term care. Most of these options have tax repercussions. And, of course, may result in either no death benefit being paid out or significantly reducing the benefit.
You May Like: Can You Get Dental On Medicare
It’s Exceedingly Rare For Health Insurance To Pay For Assisted Living And Medicare Is No Exception
As with most types of health insurance, Medicare does not pay for assisted living.
The need for assisted living is a fairly recent one, the result of Americans enjoying longer lives than previous generations. While people living longer is a good thing, it brings some unique issues our society is still figuring out how to handle. One of these is the increased need for elder care, with many adult children struggling to support their aging parents.
Although Medicare does not pay for assisted living, there are numerous options to help finance this type of long-term care.
Medicaid & Medicare Costs Coverage & Details
As of the last update, 46 states and the capital were listed as providing at least some level of payouts to those residing in an assisted living facility. Some states, specifically Louisiana, Kentucky, Alabama, and Pennsylvania do not provide Medicaid coverage for seniors who reside in assisted living homes. Though Medicaid is not offered, these states have other non-Medicaid programs that seniors may avail to help pay for their long-term care costs.
Support types and levels vary greatly from state to state. However, states that are barred from offering direct Medicaid payments create other unique solutions for seniors. Some ways states assist seniors is by placing a firm limit on the number of fees a facility that is Medicaid certified may charge. Another is by offering seniors who are Medicaid-eligible supplemental assistance for their assisted living fees. Instead of these funds originating from Medicaid, they are taken out of general state funds to help pay for senior assisted living costs.
Another way many states help senior Medicaid recipients reduce the expenses of assisted living is by covering the fees of supplemental services offered by these communities. Assisted living supplemental services may include personal care, medical assessments, coverage of nursing care, medication management, case management and medical exams.
Also Check: Who Do You Call To Sign Up For Medicare
Nursing Homes Vs Assisted Living Facilities
Many people talk about nursing homes and assisted living facilities as if theyre the same thing. But Medicare treats them very differently when it comes to coverage.
Medicare doesn’t cover help with daily living activities if it’s the only care you need. Most nursing home and assisted living care is custodial care. However, Medicare Part A may cover care in a licensed nursing facility for a limited time if you need skilled nursing care.
A common and popular alternative to a nursing home is an assisted living facility. Theyre a great option for people who no longer canor care tolive on their own, but they can be expensiveand Medicare doesnt cover them.