Does Medicare Cover Cancer
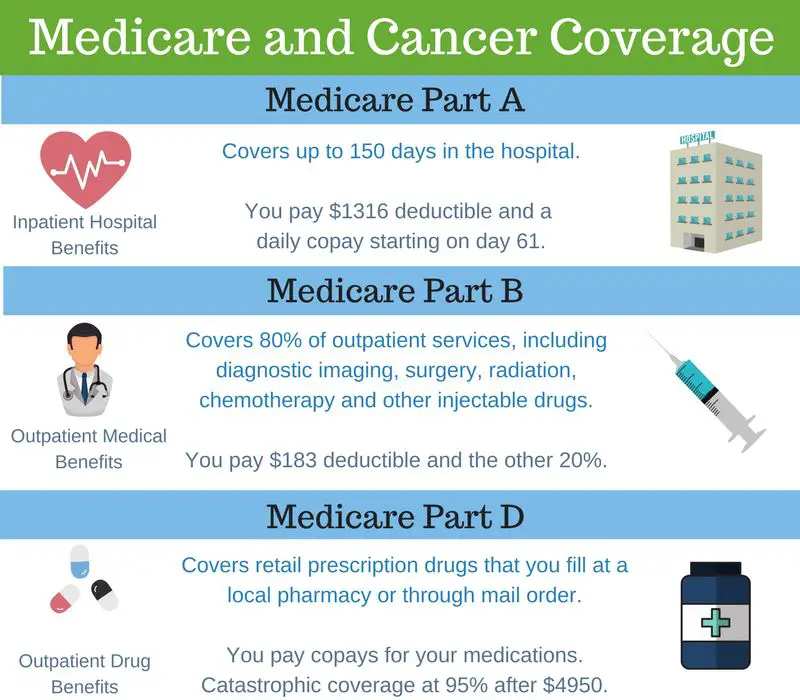
Depending on your specific cancer and circumstances, your doctors will work together to develop a treatment plan for you that meets your needs. Medicare helps cover the services, tests and items you may need for your cancer treatment. Typically, these may include surgery, chemotherapy, immunotherapy and/or other treatments, which would be covered either under Part A, Part B or Part D.
How Can I Clean My Prostate
10 diet & exercise tips for prostate health
Will Medicare Cover My Breast Cancer Costs
Medicare offers coverage for medically necessary cancer expenses. However, itâs not full coverage. You will still have coinsurance, deductibles, and copays, which is why we recommend supplemental coverage called a Medicare Supplement.
These are very inexpensive to have, especially if youâre used to paying for traditional health insurance!
If we didnât go over a breast cancer service or test that youâre interested in, on your smartphone. There, you can type in any item, test, or service, and Medicare will tell you if itâs covered and what your costs will be.
For non-medical costs like loss of income, transportation to specialized facilities, lodging at those out-of-town hospitals, and more, we recommend securing a cancer insurance policy.
Cancer insurance is very inexpensive to have , and they pay you a lump sum as soon as you are diagnosed with cancer.
Also Check: Who Has The Best Medicare Supplement
Total Or Simple Mastectomy
A total mastectomy is the removal of the entire breast. It does not include the removal of lymph nodes in the underarm area or muscles underneath the breast.
A doctor may recommend this procedure for people with multiple cancers or large areas of cancer in their ducts, or people with a high risk of breast cancer who want to undergo prophylactic surgery.
Is Cancer Gone After Mastectomy
Even though the entire breast is removed in a mastectomy, breast cancer can still return to the chest area. If you notice any changes around the mastectomy scar, tell your health care provider. The more lymph nodes with cancer at the time of the mastectomy, the higher the chances of breast cancer recurrence.
Read Also: How To Get Medical Equipment Through Medicare
Medicare Advantage Plans Cover Breast Cancer Treatments And Screenings
Medicare Advantage plans are required to offer all of the same benefits that are covered by Original Medicare, combined into a single plan.
This means that the breast cancer screenings, treatments and drugs listed above are covered by Medicare Advantage plans in the same way that they are covered by Medicare Part A and Part B.
Some Medicare Advantage plans may also offer coverage for potentially more breast cancer drug costs than what Original Medicare covers.
Two out of every three cases of invasive breast cancer occur in women over the age of 55.1 And breast cancer accounts for the second-highest number of cancer-related deaths for U.S. women, behind only lung cancer.2
Dont let your breast cancer screenings and treatment go without adequate medical attention and insurance coverage.
If you want to learn more about how a Medicare Advantage plan could help offer the benefits you need, call to speak with a licensed insurance agent today or compare plans online, with no obligation to enroll.
Find Medicare Advantage plans in your area
Or call 1-800-557-6059TTY Users: 711 to speak with a licensed insurance agent. We accept calls 24/7!
About the author
Christian Worstell is a senior Medicare and health insurance writer with MedicareAdvantage.com. He is also a licensed health insurance agent. Christian is well-known in the insurance industry for the thousands of educational articles hes written, helping Americans better understand their health insurance and Medicare coverage.
How Far Along Your Breast Cancer Is Will Greatly Impact Your Costs
What will have the greatest impact on overall medical costs is how far along the breast cancer has progressed.
A 2016 study completed by Helen Blumen, Kathryn Fitch, and Vincent Polkus examined the costs of care depending on which stage the breast cancer was when diagnosed.
This study found that overall, treatment costs were higher for patients whose cancer was more advanced when they were diagnosed. This is largely due to chemotherapy, which was responsible for the highest percentage of total costs for stage 4 patients.
In the second year after being diagnosed, chemo costs were the single largest contributor to treatment costs in every single stage of the disease.
However, for patients who were diagnosed early on , their surgery costs were more than double those with stage 4 breast cancer, which reflects the curative nature of surgery for early-stage disease.
When looking at the average costs per patient allowed by the insurance company in this study, the expenses range from $60,000-$134,000 depending on how advanced the breast cancer was at diagnosis.
Those numbers can be striking, so itâs important to know: does Medicare cover breast cancer?
Also Check: Do You Have To Have Medicare At 65
Other Types Of Covered Breast Screening
Medicare covers one baseline screening mammogram for women 3539 years old and annual screening mammograms for women 40 years and older. There is no age cap.
To be clear, Medicare specifically limits screening to women. Transgender individuals may also be covered if a screening mammogram was considered medically appropriate based on their biology and whether they have undergone hormonal or surgical procedures.
Diagnostic mammograms may be performed more often than every 12 months if your healthcare provider considers them medically necessary. These tests can be ordered for anyone who has an abnormal mammogram finding, a prior history of breast cancer, or symptoms related to the breasts.
Breast ultrasound is a diagnostic test and is not considered preventive screening in the eyes of Medicare. Again, Medicare will cover the test if it is deemed medically necessary. For example, a woman with dense breasts on a mammogram or a person of any sex or gender with breast-related symptoms may qualify for an ultrasound.
Does Medicare Cover A Double Mastectomy
A mastectomy is a surgical operation to remove one or both breasts, partially or completely. This is done to treat breast cancer, but occasionally, it is done as a preventative measure for women with a very high risk.
Across the board, Medicare covers medically necessary surgical procedures. This means that Medicare will cover a double mastectomy as long as it is medically necessary.
If youâre considering a mastectomy as a preventative measure, you will need to talk with your doctor about what your costs may be. If your doctor does not feel the mastectomy is medically necessary, Medicare will not cover the procedure.
Breastcancer.org explains that Medicare helps cover breast reconstruction.
Medicare Part A, or your hospital insurance, helps cover surgically-implanted breast prostheses after a mastectomy if the surgery took place in an inpatient setting. If the surgery took place in an outpatient setting, Medicare Part B will help cover it.
Please remember: just because Medicare covers a mastectomy does not mean you will have no out-of-pocket costs!
It is highly advised to get a Medicare Supplement, which will either completely cover or greatly assist with the expensive 20% coinsurance as well as some deductibles and copays.
Don’t Miss: What Is The Medicare Expansion
Using Your Own Tissue
Reconstruction using your own skin, fat and muscle is called tissue flap reconstruction. There are two main types of tissue flap reconstruction. These are attached flaps and free flaps.
- Attached flaps use skin, fat and muscle from your back or abdomen. A portion of tissue and muscle is tunnelled under the skin from your back or abdomen to your chest where the new breast is formed.
- Free flaps use skin, fat and muscle removed from your abdomen or buttock. The arteries and veins are cut and then attached to the blood supply of the chest wall.
The main advantages of tissue flap reconstruction are:
- it produces a more natural looking breast
- the breast will gain and lose weight as your body gains and loses weight.
The main disadvantages of tissue flap reconstruction are:
- it requires longer surgery and recovery time
- you will have a scar on your back or stomach
- you may lose strength in your stomach muscles if your reconstruction uses abdominal tissue
- there is a small risk that the flap may die due to lack of blood supply if this happens it may need to be removed and another operation may be required.
Medicare Coverage For Genetic Testing
In general, Medicare insurance does not cover genetic testing however, there are some circumstances in which the program will cover genetic testing for breast cancer as long as you have met certain requirements, including having a personal or family history of breast cancer.
If covered under Original Medicare, genetic testing benefits will be provided by Medicare Part B for any services rendered through your doctors office or a lab. If testing is conducted while you are admitted to a hospital or skilled nursing facility, Medicare Part A would likely apply instead.
TIP: Are you ready to get the most out of Medicare? Head on over to our Medicare basics guide.
Don’t Miss: Is Medical Assistance The Same As Medicare
If You Want To Change Your Medicare Plan Post
If you receive a cancer diagnosis and want to change your Medicare plan, the CMS says that this request can only take place during very specific times. For instance, if you want to change your policy from Original Medicare to Medicare Advantage, you can only do so during open enrollment, which is between October 15th and December 7th of each year, with coverage initiating January 1st of the following year. However, if your goal is to disenroll in Medicare Advantage and go back to Original Medicare, the time frame for this is January 1st to February 14th.
Are You Looking For Free Insurance Quotes

Your one-stop online insurance guide. Get free quotes now!
Secured with SHA-256 Encryption
Editorial Guidelines: We are a free online resource for anyone interested in learning more about insurance. Our goal is to be an objective, third-party resource for everything insurance related. We update our site regularly, and all content is reviewed by insurance experts.
|
D. Gilson is a writer and author of essays, poetry, and scholarship that explore the relationship between popular culture, literature, sexuality, and memoir. His latest book is Jesus Freak, with Will Stockton, part of Bloomsburys 33 1/3 Series. His other books include I Will Say This Exactly One Time and Crush. His first chapbook, Catch & Release, won the 2012 Robin Becker Prize from Seve… |
Also Check: Does Blue Cross Medicare Advantage Cover Dental
Breast Cancer: What Medicare Covers
by alAdmin | Oct 20, 2021 | Medicare |
Breast cancer is the second most widespread cancer in women. In fact, about 1 in 8 U.S. women will emerge with invasive breast cancer. The best way to go about treating breast cancer, and cancer in general, is by identifying it at an early stage. Generally, it is suggested that all women aged 40 and above get a yearly mammogram. Regular screenings can identify a lump or irregularity years before it can be physically detected. Wondering what Medicare covers in relation to breast cancer screenings? Were here to help.
Does Medicare Cover Needle Biopsies
Needle biopsies involve inserting a needle into your body to get cells from your muscles, bones, or organs for testing. Needle biopsies may detect cancer or diagnose other conditions such as infections or inflammations.
There are two types of needle biopsies: Fine needle aspiration and core needle biopsy. Medicare covers both kinds of needle biopsies. Coverage is the same as for other types of biopsies Medicare also covers anesthesia and imaging tests such as CT scans, which your doctor may administer before or as part of the biopsy procedure.
Recommended Reading: When Can I Get My Medicare
For Lung Cancer Medicare Part B Will Cover The Following Screening:
A Low-Dose Computed Tomography if all of the following conditions are met:
- Youre over age 55
- You get a written order from your doctor
- Youre either a current smoker or have quit within the last 15 years
- You have a history of smoking an average of one pack or 20 cigarettes per day for 30 years
- You dont exhibit any signs or symptoms of lung cancer
How Medicare Covers Breast Cancer Prevention And Treatment
Medicare does cover certain breast cancer screenings and treatments.
Medicare Part A helps cover the costs associated with any inpatient hospital breast cancer treatment, such as surgery and chemotherapy. Medicare Part B helps cover the costs of your outpatient care and annual mammograms.
Learn more about how Medicare helps to cover the costs associated with detecting and treating breast cancer.
Don’t Miss: Is Joe Biden For Medicare For All
How Much Does A Mammogram Cost
Humana plans cover annual preventive mammograms with no out-of-pocket costs to Humana members beginning at age 40.
The cost for a diagnostic mammogram, such as to diagnose a medical condition, can vary based on your insurance coverage, age, what state you live in or your income.6 Humana Medicare Advantage plans generally include a diagnostic mammogram if ordered by a doctor. Cost share may vary depending on the plan.
If you have Medicare Part B or Medicare Advantage, you are covered for all of the costs of yearly screening mammograms and up to 80% of the cost of necessary diagnostic mammograms. However, there may be some additional out-of-pocket costs for diagnostic mammograms.7
Several government programs and nonprofits provide low-cost or free mammograms for low-income or uninsured women across the U.S., such as the
Does Medicare Cover Mammograms
A mammogram is a low-energy X-ray of the breast to detect breast cancer.
Medicare is a huge advocate for screenings and preventive medicine, which is why Medicare Part B fully covers a screening mammogram once per year. Diagnostic mammograms can be done more frequently if itâs medically necessary.
Screening mammograms are free, and diagnostic mammograms come with a 20% coinsurance. A Medicare Supplement, if you choose to get one, would pick up that coinsurance.
Get more information: Mammograms and Medicare: What You Need to Know
Don’t Miss: How Do I Stop Medicare Junk Mail
Family History And Genetics
Certain people may be at increased risk for breast cancer based on their genes , medical conditions , or family history of breast and/or ovarian cancer, especially in first-degree relatives .
Females with a BRCA-1 gene mutation have a 72% lifetime risk for developing breast cancer, and those with the BRCA-2 gene mutation have a 69% risk. These genes also increase ovarian cancer risk.
When It Comes To Cancer What Does Medicare Advantage Cover

Medicare Advantage, also known as Medicare Part C, replaces coverage for Medicare parts A, B, and sometimes D. According to the Centers for Medicare & Medicaid Services, all Medicare Advantage plans must provide the same services as Original Medicare, including:
- Inpatient hospital stays such as inpatient cancer treatments
- Outpatient radiation treatment
- Some cancer screenings
Because chemotherapy is covered under Medicare Part D, a Medicare Advantage plan with Part D included will cover chemotherapy treatments.
âWhen chemo and radiation are administered, the most a Medicare Advantage plan can charge in coinsurance is 20 percent. While the coinsurance can vary from plan to plan, almost all pay to charge the max of 20 percent. There are some that charge less, but those are rare,â Christopher Duncan, founder and independent broker at Trusted Benefits Direct, tells WebMD Connect to Care.
Medicare Advantage plans must provide the same coverage as Original Medicare. The Centers for Medicare & Medicaid Services notes that, for breast cancer patients, this coverage includes:
- Surgically-implanted breast prostheses after a mastectomy
- Post-mastectomy external breast prostheses, including a post-surgical bra
Medicare Advantage HMO plans have a restrictive network. Aside from emergency care, you would have to see the doctors, hospitals and providers within your chosen HMO network.
Read Also: Stage 4 Breast Cancer Life Expectancy Without Treatment
Don’t Miss: Which Medicare Insurance Is Best
Do I Need Medicare Part B If I Have Employer Insurance
Summary: You are not required to have Medicare Part B coverage if you have employer coverage. You can drop Medicare Part B coverage and re-enroll in it when you need it. … You also may choose to defer enrollment in Medicare Part B coverage if you are employed at age 65 or older and eligible for Medicare.
Its All About You We Want To Help You Make The Right Coverage Choices
Advertiser Disclosure: We strive to help you make confident insurance decisions. Comparison shopping should be easy. We are not affiliated with any one insurance provider and cannot guarantee quotes from any single provider.
Our insurance industry partnerships dont influence our content. Our opinions are our own. To compare quotes from many different insurance companies please enter your ZIP code on this page to use the free quote tool. The more quotes you compare, the more chances to save.
On This Page
- Medicare covers breast reconstruction surgery after a lumpectomy due to breast cancer
- Medicare doesnt cover any breast surgery that is considered cosmetic in nature
- You will have to pay coinsurance after your deductible is met
Does Medicare cover breast reconstruction after lumpectomy? Medicare will cover any breast reconstruction surgery that is medically necessary as a result of breast cancer surgeries. This includes breast reconstruction after mastectomy and lumpectomy. Your Part A coverage will pay for inpatient hospital costs, while Medicare Part B covers medical costs such as tests and doctor visits. Both parts have a deductible, and Part B has a 20 percent coinsurance. You can supplement your Medicare health insurance with a Medigap plan that will pay for some or all of these out-of-pocket costs.
To shop for a Medicare plan that covers breast reconstruction surgery after a lumpectomy out-of-pocket expenses, enter your ZIP code.
Read Also: Are Medical Alert Systems Covered By Medicare
