Banner University Family Care / Ahcccs Complete Care
B UFC/ACC is a health plan for participants in the Arizona Health Care Cost Containment System , which is Arizonas Medicaid program.
As of October 1, 2018, physical and behavioral health care services, or integrated care, will be coordinated under B UFC/ACC. The new integrated system, AHCCCS Complete Care, will improve coordination of care between providers and improve health outcomes for our members.
Q How Much Income Can I Receive And Still Be Eligible For Medicaid
A. Income is money that you get from working, or money that someone gives you, or checks that you receive, such as a Social Security check, unemployment benefits, child support, retirement benefits, or sick pay. Whether your income level qualifies you or your family for Medicaid depends on the size of your family and the Medicaid program for which you are applying.
Income limits are set each year by the federal government to define the Federal Poverty Level for different family sizes. In general, if your household income is at or below the current 100% Federal Poverty Level for your household size, your family is likely to be eligible for Medicaid. Children from age 1 to under age 6 can qualify for Medicaid benefits when household income is at or below 133% of the Federal Poverty Level. Pregnant women and infants under age 1 qualify for Medicaid with family income at or below the 200% Federal Poverty Level, and pregnant women count as 2 family members.
See our tables of income limits for applying for DMMA programs to find out where your family income is, in relation to these income benchmarks.
Medical assistance programs other than Medicaid have different income level requirements. For example, uninsured children under age 19 who live in families with incomes at or below the 200% Federal Poverty Level are eligible for low cost health insurance under the Delaware Healthy Children Program.
New And Updated Medical Assistance Resources For Covid
According to an , one in seven Americans said theyd skip medical care related to the novel coronavirus if they had symptoms due to medical-bill fears. Federal legislation and health insurance companies are taking steps to reduce the likelihood of that care avoidance from happening.
The federal Families First Coronavirus Response Act, which went into effect April 1, 2020, requires all health insurance plans whether theyre private, government-sponsored , military, or purchased through the Healthcare Insurance Marketplace, subsidized or not to pay for COVID-19 tests and doctor’s fees associated with testing with no out-of-pocket costs to consumers such as copays or meeting your deductible first, according to the Kaiser Family Foundation.
The act also requires employers to pay for sick leave and family leave if you become infected with or must care for a family member with COVID-19, according to the U.S. Department of Labor.
In addition, large health insurers including Aetna, Anthem, Blue Cross Blue Shield, Cigna, Humana, and UnitedHealthcare announced earlier this spring they were waiving patient costs for coronavirus treatment. That could save you an estimated $1,300 in out-of-pocket costs for treating a severe infection, according to data published in March by the Kaiser Family Foundation. Insurers set end dates on this extra benefit that range from late May to September, so contact your health insurer to see if waivers are still in effect.
Guide
Don’t Miss: Will Medicare Pay For Liposuction
Q How Will I Receive My Medical Care
A. In Delaware, Medicaid benefits are provided mainly through a managed care organization, or MCO, under contract with the state. Managed care is an organized way to ensure that people receive the quality medical care they need in the most cost-effective manner. Some Medicaid recipients in Delaware those who also receive Medicare and those in Long Term Care Medicaid programs such as the Nursing Facility program do not receive their medical care through a managed care organization.
DMMA provides a choice of managed care organizations so you can select the MCO plan that is best for you and your family. Delaware contracts with two managed care plans AmeriHealth Caritas and Highmark Health Options.
The Medicaid MCO provides almost all of the care for Medicaid members who join their plan. Prescription and non-emergency medical transportation services are covered directly by Medicaid, not through the MCO. Medicaid recipients need to show their Medicaid card to pharmacies and transportation providers when receiving these services.
What Is The Ship Program Medicare

A national SHIP program facilitates access to individual one-on-one assistance, counseling, and information to Medicare beneficiaries, their families, and caregivers so that they may make informed decisions about their health care. Under the vision of SHIP, Medicare information is to be readily available to the public, trusted, and publicly recognized.
Recommended Reading: How Does Medicare Part D Deductible Work
Mn Medicaid Coverage And Costs
The MN Medicaid program is usually referred to as the Minnesota Medical Assistance program. Its a very comprehensive program, but keep in mind that in some cases, a doctor will have to prove that your treatment is medically necessary and submit it to Medicaid for approval before you can receive coverage for that treatment.
Costs are very limited for this program. Some adults may need to pay a monthly deductible of less than $3 before receiving full coverage. Copays are usually $0 or $1 and are never more than $3.50. Kids, pregnant women, care facility residents, those in hospice, and those in the breast/cervical cancer program will not owe any copays. Every month, your out-of-pocket maximum will be 5% of your monthly household income.
Coverage includes treatments and services related to:
- Alcohol and substance abuse
- Urgent care
What Are Dual Health Plans
Dual health plans are designed just for people who have both Medicaid and Medicare. Theyre a special type of Medicare Part C plan. Dual health plans combine hospital, medical and prescription drug coverage. Youll keep all your Medicaid benefits. Plus, you could get more benefits than with Original Medicare. And you could get it all with as low as a $0 plan premium.
View the “Do I Lose My Medicaid Benefits?” article.
You May Like: What Is Medicare Plan F
Who Is Eligible For Medicaid
You may qualify for free or low-cost care through Medicaid based on income and family size.
In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level.
- First, find out if your state is expanding Medicaid and learn what that means for you.
- If your state is expanding Medicaid, use this chart to see what you may qualify for based on your income and family size.
Even if you were told you didn’t qualify for Medicaid in the past, you may qualify under the new rules. You can see if you qualify for Medicaid 2 ways:
- Visit your state’s Medicaid website. Use the drop-down menu at the top of this page to pick your state. You can apply right now and find out if you qualify. If you qualify, coverage can begin immediately.
- Fill out an application in the Health Insurance Marketplace. When you finish the application, we’ll tell you which programs you and your family qualify for. If it looks like anyone is eligible for Medicaid and/or CHIP, we’ll let the state agency know so you can enroll.
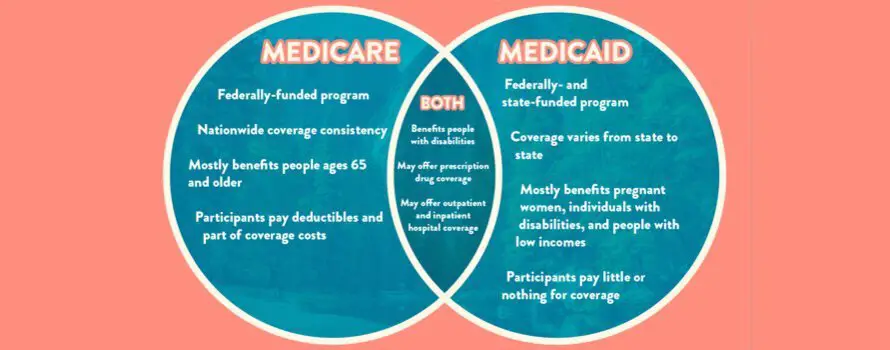
Medicare And Medicaid Funding
Medicare is funded:
- In part by the Medicare payroll tax
- In part by Medicare recipients premiums
- In part by general federal taxes
The Medicare payroll taxes and premiums go into the Medicare Trust Fund. Bills for healthcare services to Medicare recipients are paid from that fund.
Medicaid is:
- Partially funded by the federal government
- Partially funded by each state
The federal government pays an average of about 60% of total Medicaid costs, but the percentage per state ranges from 50% to about 78%, depending on the average income of the state’s residents .
Under the ACA’s expansion of Medicaid, however, the federal government pays a much larger share.
For people who are newly eligible for Medicaid due to the ACA , the federal government pays 90% of the cost, while the states pay just 10% of the cost.
Read Also: How Much Does Medicare Pay For A Doctors Office Visit
Opting For Part A Only
Some people choose only to have Medicare Part A coverage so that they dont have to pay the monthly premiums for Medicare Parts B and D. If you still have insurance through a current employer , you can add the other parts later with no penalty.
However, if you decline Parts B and D and don’t have another insurance plan in place, you’ll face a late enrollment penalty when you add the other parts later.
In the past, Medicaid programs typically didn’t offer a lot of choice in terms of plan design. Today, most states utilize Medicaid managed care organizations . If there’s more than one MCO option in your area of the state, you will likely be given the option to select the one you prefer.
Dual Eligible Special Needs Plans
People who are dual eligible for Medicare and Medicaid may be able to enroll in a Dual Eligible Special Needs plan, also known as D-SNP.
Any D-SNP provides at least the same coverage as Medicare Part A and Part B along with Part D prescription drug coverage. But they usually include more coverage on top of that.
Extra benefits can include dental, hearing and vision coverage, help buying health-related products and transportation assistance to get to and from a health care provider.
A Dual Eligible Special Needs plan will not replace your existing Medicaid plan or change your eligibility for the program.
You May Like: How Do I Replace My Medicare Card Online
How To Get Both Medicare And Medicaid In Minnesota
If you meet the eligibility requirements for MN Medicaid and are eligible for Medicare, you can benefit from both programs! In fact, you may be eligible for a Dual-Eligible Special Needs Plan, or DSNP. DSNPs are Medicare Advantage plans designed specifically for people who benefit from both Medicare and Medicaid. Most people with a DSNP wont pay anything for their Medicare coverage.
For help finding out if you qualify and for help selecting a Dual-Eligible Special Needs Plan, complete this form, and well have one of our licensed agents reach out to you ASAP.
What Are The Ahcccs Income Limits To Receive Medicaid In Arizona
The Medicaid program in Arizona is called AHCCCS . AHCCCS is jointly federal and state funded and helps to support low-income individuals who are younger than 65 . You might qualify for benefits through this program if you earn 138 percent of the FPL or less. As of 2019, this is $35,535 for a household with four family members and $17,236 for an individual.
If youre over 65, youll need to apply for Medicaid benefits through the ALTCS . Unlike other Medicaid services, which place a limit on how many participants can enroll, ALTCS offers benefits as an entitlement. In other words, if you meet the requirements for eligibility, you can access services.
The income and asset limits for ALTCS is can be tricky to navigate. Well go into detail on that soon, in addition to ways you can qualify even if you dont meet the requirements.
Also Check: How Do You Apply For Extra Help With Medicare
Basis Of Eligibility And Maintenance Assistance Status
Medicaid does not provide medical assistance for all poor persons. Under the broadest provisions of the Federal statute, Medicaid does not provide health care services even for very poor persons unless they are in one of the following designated groups. Low income is only one test for Medicaid eligibility for those within these groups their resources also are tested against threshold levels .
States generally have broad discretion in determining which groups their Medicaid programs will cover and the financial criteria for Medicaid eligibility. To be eligible for Federal funds, however, States are required to provide Medicaid coverage for certain individuals who receive federally assisted income-maintenance payments, as well as for related groups not receiving cash payments. In addition to their Medicaid programs, most States have additional State-only programs to provide medical assistance for specified poor persons who do not qualify for Medicaid. Federal funds are not provided for State-only programs. The following enumerates the mandatory Medicaid categorically needy eligibility groups for which Federal matching funds are provided:
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
Read Also: What Is Better Original Medicare Or Medicare Advantage
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
You May Like: Do You Have To Get Medicare When You Turn 65
Expansion Under The Affordable Care Act
As of December 2019, 37 states and the District of Columbia have accepted the Affordable Care Act Medicaid extension. Among adults aged 18 to 64, states that expanded Medicaid had an uninsured rate of 7.3% in the first quarter of 2016, while non-expansion states had a 14.1% uninsured rate. Following a 2012 Supreme Court ruling, which held that states would not lose Medicaid funding if they did not expand Medicaid under ACA, several states rejected the option. Over half the national uninsured population lives in those states.
The Centers for Medicare and Medicaid Services estimated that the cost of expansion was $6,366 per person for 2015, about 49 percent above previous estimates. An estimated 9 to 10 million people had gained Medicaid coverage, mostly low-income adults. The Kaiser Family Foundation estimated in October 2015 that 3.1 million additional people were not covered in states that rejected the Medicaid expansion.
Studies of the impact of Medicaid expansion rejections calculated that up to 6.4 million people would have too much income for Medicaid but not qualify for exchange subsidies. Several states argued that they could not afford the 10% contribution in 2020. Some studies suggested that rejecting the expansion would cost more due to increased spending on uncompensated emergency care that otherwise would have been partially paid for by Medicaid coverage,
Ahcccs Freedom To Work And Medicare
If you are eligible for both AHCCCS Freedom to Work and Medicare, it will help you to have both because:
- If your income is low enough, AHCCCS Freedom to Work may pay your Part B premium . In some cases it may even pay for Medicare deductibles, co-insurance, and copayments.
- You will automatically qualify for the Part DLow Income Subsidy. The Low Income Subsidy means you may not have to pay a premium for your Part D or any deductibles. All you would pay for prescription drugs are Part Ds copayments, which range from $1.30 to $9.20.
To learn more, read DB101s detailed information on Medicare Savings Programs for Parts A and B and the Part D Low Income Subsidy.
Depending on your situation, you might get employer-sponsored coverage, AHCCCS Freedom to Work, and Medicare all at the same time. This can sound confusing, but it can help you, because one form of coverage may pay for costs that your other coverage wont pay for.
The rules about how your different types of coverage pay for things are very complicated, so its important to check with your health coverage plans when you have questions about which plan will pay for what expenses.
Generally speaking, AHCCCS Freedom to Work will only pay for expenses that it covers and that your other coverage wont pay for.
Recommended Reading: Is Shingrix Vaccine Covered By Medicare
Mental Health And Addiction Treatment
The Minnesota Medicaid program takes mental health treatment very seriously. Its often a benefit that is forgotten about because mental illnesses are not always conditions you can see. However, treatment for mental health concerns is just as important as physical health treatments. These are some of the care options you can receive through Minnesota Medical Assistance:
- Adult Rehabilitation Facilities
- At-home Assertive Community Treatment
- Certified Community Behavioral Health Clinics
- Certified peer specialists
- Inpatient and outpatient hospital treatments
- Psychosis treatment
